2019 Volume 247 Issue 2 Pages 75-86
2019 Volume 247 Issue 2 Pages 75-86
Bisphosphonates (BPs) have been used as antiresorptive agents to treat patients with osteoporosis or metastatic bone cancer, each of which is characterized by bone loss due to the increased bone resorption. However, BPs could cause osteonecrosis of the jaw (ONJ), known as bisphosphonate-related osteonecrosis of the jaw (BRONJ). ONJ is associated with severe pain and deteriorated quality of life. ONJ is also caused by administration of denosumab, a monoclonal antibody against receptor activator of NFκB ligand (RANKL), that functions as a powerful antiresorptive agent. Accordingly, antiresorptive agent-related ONJ (ARONJ) has been advocated, the incidence of which is continuing to increase in Japan as a super-aging society. Importantly, the jawbone is more susceptible to infection compared with bones in other parts of the body, due to the unique anatomical and physiological characteristics; for example, the jawbone with a high remodeling rate is stimulated by teeth during mastication. The risk factors of ARONJ include dental infection, poor occlusal or oral hygiene status, and bone-invasive dental treatment, such as tooth extraction, dental implants, and dentures. Proper collaboration between doctors and dentists is of utmost importance to understand the current status of ARONJ and prevent developing ARONJ. It is also important to ensure that the patients treated with BPs or denosumab can receive appropriate dental treatment. More recently, angiogenesis inhibitors were reported to cause ONJ; thus, medication-related ONJ (MRONJ) has been advocated. This article overviews the concept of MRONJ by focusing on antiresorptive agents and the status of BRONJ in Japan.
Osteomyelitis of the jaw may occur in either the maxilla or the mandible, but it is often seen in the mandible, particularly the molar region, due to the differences in bone structure between trabecular bone and compact bone. Osteomyelitis that develops following radiation therapy for malignant cervicofacial tumor is known as radiation-induced osteomyelitis and is frequently encountered in regular clinical practice (Marx 1983; Dhanda et al. 2016). It is the result of dental infection in the jawbone where there is reduced capability for cellular activity, and for this reason, tooth extraction or implant therapy within the irradiation field is generally considered to be contraindicated (Katsura et al. 2008; Koga et al. 2008).
Since Marx (2003) reported avascular necrosis of the jaw caused by injectable bisphosphonates (BPs) in patients with malignancy, the term “bisphosphonate-related osteonecrosis of the jaw (BRONJ)” has been advocated for this condition, which resembles radiation-induced osteonecrosis or osteomyelitis. BPs have been used as antiresorptive agents to treat patients with osteoporosis or metastatic bone cancer. There have subsequently been numerous reports of BRONJ not only from Western countries (Advisory Task Force on Bisphosphonate-Related Ostenonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons 2007; Mavrokokki et al. 2007; Filleul et al. 2010), but also from Japan (Yoneda et al. 2010, 2017; Urade et al. 2011). Based on a large-scale study, including 4,797 patients with BRONJ (Shibahara et al. 2018), the most common site is the mandible (Fig. 1A). BRONJ causes severe pain and greatly impairs the patient’s quality of life (Fig. 1B-D). However, the pathogenesis and the treatment strategy of BRONJ remain to be clarified; namely, recommended treatments and prevention strategy of such a serious complication are not yet established, despite the continuous increase in BRONJ cases.
In 2008, the Japanese Allied Committee on Osteonecrosis of the Jaw was launched through cooperation among six academic societies in the fields of medicine and dentistry: the Japanese Society for Bone and Mineral Research, the Japan Osteoporosis Society, the Japanese Society for Oral and Maxillofacial Radiology, the Japanese Society of Periodontology, the Japanese Society of Oral and Maxillofacial Surgeons, and the Japanese Society of Clinical Oral Pathology. Subsequently, the Japanese Allied Committee has published position papers (Yoneda et al. 2010, 2017) to set out objective measures and policies for reducing BRONJ onset. However, the position papers might have caused confusion among patients taking BPs with regard to dental care; namely, numerous people taking BPs have avoided dental treatment with the fear of osteonecrosis of the jaw (ONJ). Moreover, some dentists have avoided dental treatment for the patients taking BPs. On the other hand, it appears that many doctors administer BPs without sufficient thought for the specific features of the jawbone.
This article aims to review the clinical status of BRONJ and antiresorptive agent-related osteonecrosis of the jaw (ARONJ), with an attempt to clarify the ideal measures.
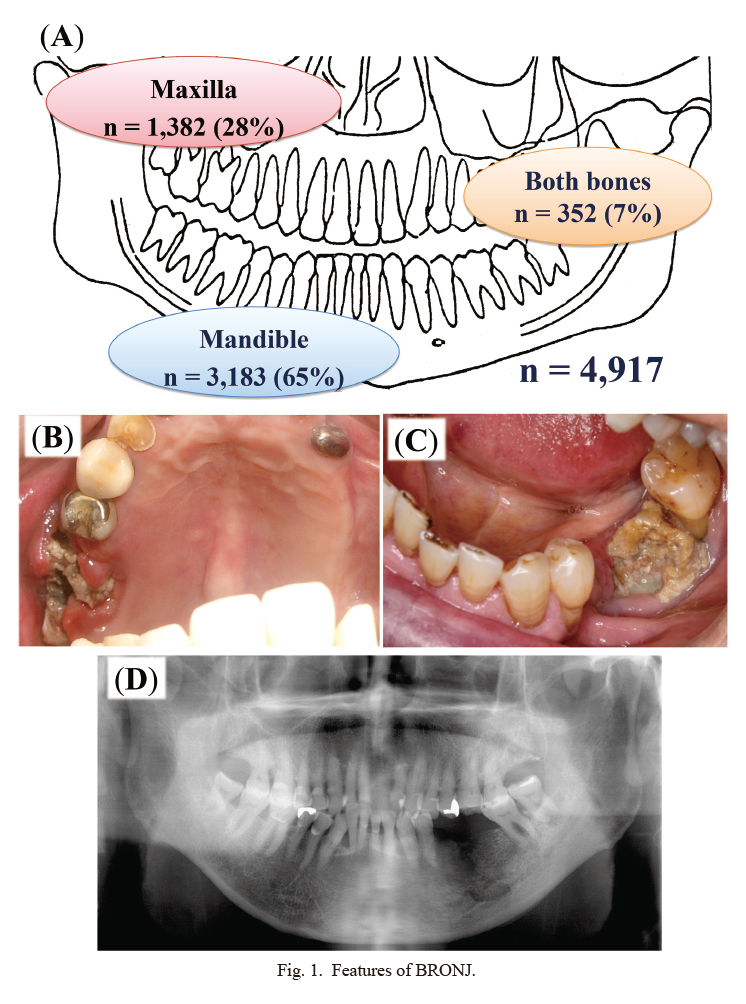
Features of BRONJ.
(A) Predilection sites of BRONJ. Among 4,917 cases of BRONJ, the mandible is most frequently affected (Shibahara et al. 2018). (B) Exposed necrotic bone in the left maxilla. Note that the photo represents a mirror image of the lesion. This photo is presented with the patient’s permission. (C) Exposed necrotic bone in the left mandible. The photo is presented with the patient’s permission. (D) X-ray image of the affected mandible of the patient shown in C.
Osteonecrosis occurs only in the jawbone, but not in other bones such as long bone and cranium due to the following reasons that are related to the anatomical and physiological characteristics (Fig. 2).
(1) Teeth erupt from the jawbone by breaking the oral epithelium; thus, sources of infection can readily reach the bone directly from the affected teeth through the epithelium.
(2) The jawbone is covered only with thin oral mucosa, which is susceptible to injury from everyday actions such as mastication, and infection due to mucosal injury can directly spread to the jawbone.
(3) Over 800 types of bacteria are present in the mouth as sources of infection at concentrations of 1011-1012/cm3.
(4) Inflammation can readily spread to the jawbone through dental infections (caries, pulpitis, apical periodontitis, and periodontal disease).
(5) The jawbone is directly exposed to the interior of the mouth, and thus susceptible to infection, as a result of invasive procedures such as tooth extraction or implant therapy.
The jawbone is more susceptible to infection compared with bones in other parts of the body, and such unique environment plays a crucial role in the pathogenesis of BRONJ. In this context, Cardemil et al. (2013) reported that the expression levels of ossification markers and bone resorption markers are different between the jawbone and tibia; such differences may reflect bone remodeling capability and affect the process of osteonecrosis. The jawbone is stimulated by teeth during mastication, and its remodeling occurs at a higher rate compared with other bone in the body.
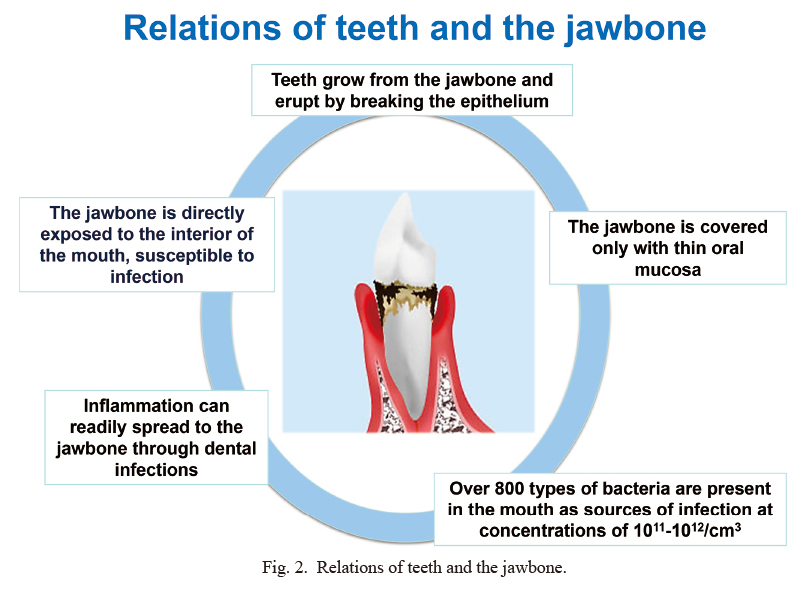
Relations of teeth and the jawbone.
The jaw bone has the unique anatomical and bacteriological characteristics.
With osteoporosis or metastatic bone cancer lesions, clear bone loss or bone breakdown is induced by increased bone resorption by osteoclasts. Various antiresorptive agents have been developed to prevent or treat bone loss or bone breakdown. These include BPs, which have powerful antiresorptive actions and are widely used as effective drugs for the prevention and treatment of bone loss in osteoporosis or metastatic bone cancer (Rosen et al. 2003; Van Poznak et al. 2011).
Following the development of BPs, the anti-RANKL (Receptor Activator of NFκB Ligand) antibody, denosumab, a powerful antiresorptive drug, was reported to be effective against bone loss in osteoporosis patients (Bekker et al. 2004). In a large-scale clinical study of 7,868 female osteoporosis patients, increased bone mass with no onset of ONJ was reported in patients who were administered denosumab (Cummings et al. 2009). However, the first report of ONJ in patients treated with denosumab was published by Taylor et al. (2010). In 2011, a large-scale clinical study of BPs and denosumab in prostate cancer patients reported that ONJ occurred at the same or higher frequency with denosumab as with BPs (Fizazi et al. 2011; Henry et al. 2011). Thus, the name, denosumab-related ONJ (DRONJ), was proposed for ONJ associated with denosumab treatment (Ristow et al. 2014). In fact, denosumab was reported to show the higher incidence of ONJ compared with BPs (Stopeck et al. 2016).
It has become clear that ONJ is caused by administration of the antiresorptive agents BPs and denosumab, and in 2011, the American Dental Association proposed the comprehensive name ARONJ for ONJ related to BP or denosumab (Hellstein et al. 2011). Subsequently, in 2014 the American Association of Oral and Maxillofacial Surgeons (AAOMS) proposed the name “medication-related ONJ (MRONJ)” to include ONJ caused by anti-angiogenesis agents as well as antiresorptive agents (Ruggiero et al. 2014) (Fig. 3). The anti-angiogenesis agents include tyrosine kinase inhibitors, anti-VEGF (vascular endothelial growth factor) human monoclonal antibodies, and mTOR (mammalian target of rapamycin) inhibitors (Nicolatou-Galitis et al. 2019). There is the report that romosozumab (anti-sclerostin monoclonal antibody) also induced MRONJ, although this is a bone-forming agent, but not an antiresorptive agent (Cosman et al. 2016; Saag et al. 2017). There are still many points to be unclarified with regard to the mechanism of MRONJ onset due to these drugs. The clinical features of MRONJ are summarized in Table 1.
In 2017, the Japanese Allied Committee on Osteonecrosis of the Jaw published “Antiresorptive agent-related osteonecrosis of the jaw: Position Paper 2017 of the Japanese Allied Committee on Osteonecrosis of the Jaw” (Yoneda et al. 2017). The 2017 position paper used the name ARONJ, which was also used by the International Task Force on Osteonecrosis of the Jaw. For details of ARONJ, including diagnosis, incidence, clinical condition and staging, and risk factors, please refer to the 2017 position paper.
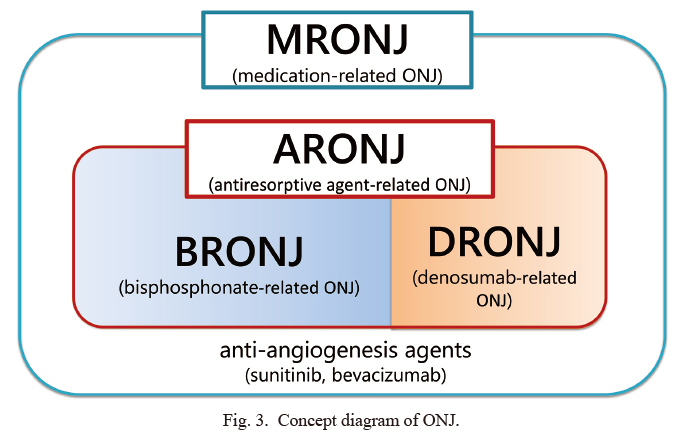
Concept diagram of ONJ.
BP, bisphosphonate.
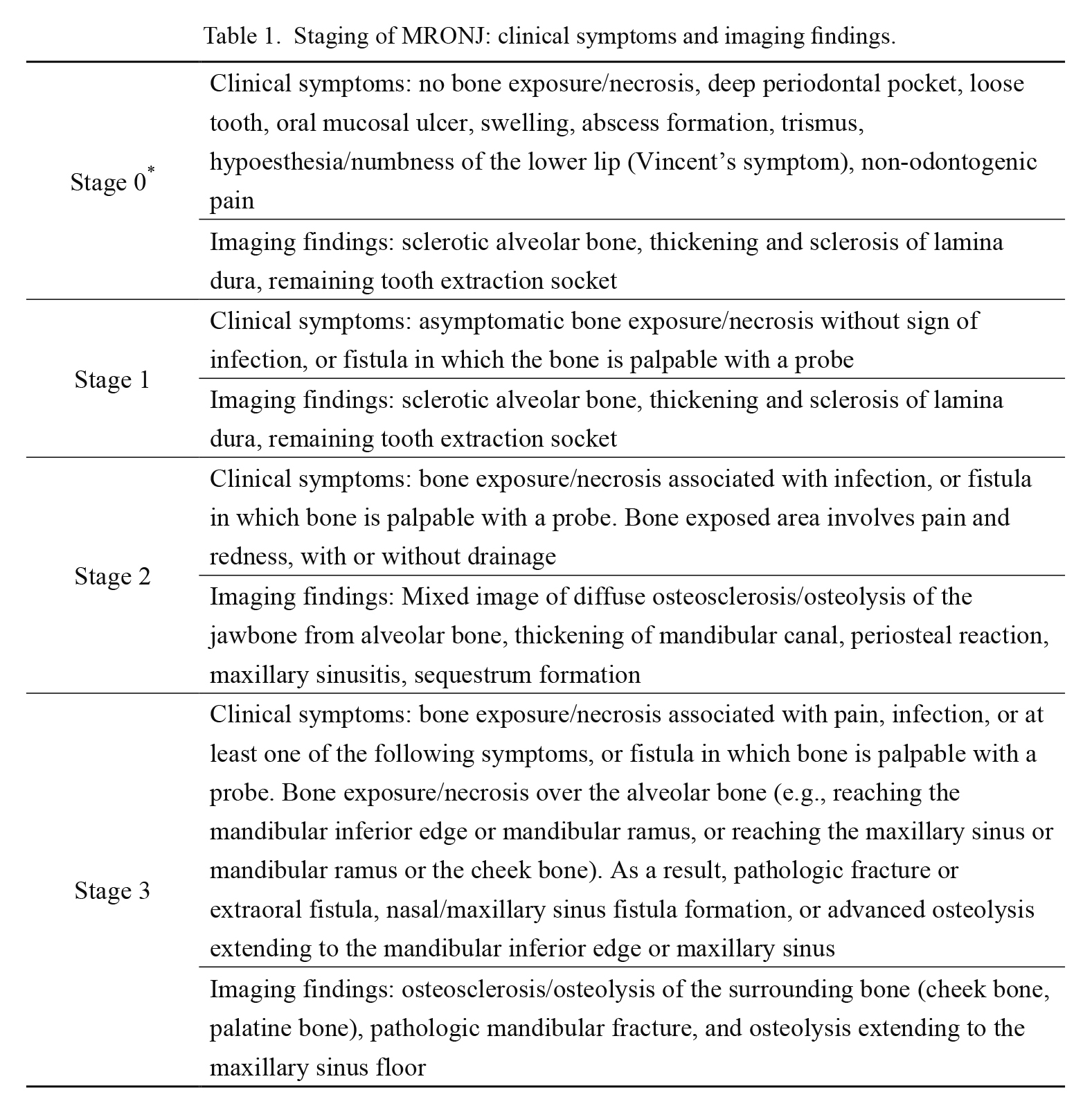
Staging of MRONJ: clinical symptoms and imaging findings.
*Care should be taken to avoid overdiagnosis because half of Stage 0 cases do not progress to ONJ.
The incidence of BRONJ due to oral BPs was estimated to be 0.01% of patients using BPs by the AAOMS (Ruggiero et al. 2014), 0.01-0.04% by the European Association for Cranio-Maxillo-Facial Surgery (EACMFS) (Mavrokokki et al. 2007), and 0.001-0.069% by the International Task Force on Osteonecrosis of the Jaw (Khan et al. 2017). In Japan, the incidence of BRONJ due to oral BPs was estimated to be 0.01-0.02% (Yoneda et al. 2010). However, BRONJ due to high dose BPs was estimated to be 0.8-12% by the AAOMS (Advisory Task Force on Bisphosphonate-Related Ostenonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons 2007), 0.88-1.15% by the EACMFS (Mavrokokki et al. 2007), and 1-2% in Japan (Yoneda et al. 2010).
Based on the large-scale report in Japan (Shibahara et al. 2018), the prevalence of BRONJ was 28 in 2006, 263 in 2008 (87.7 per year), and 4,797 in 2015 (1,599 per year). Thus, by 2015 there had been an appalling increase of 18.2 times the 2008 and 57.1 times the 2006. Our 2018 report represents patients with stage 1 and higher in BRONJ. If stage 0 (latent ONJ) and data from general practice dental clinics were included, the numbers would probably reach horrifying proportions.
Tooth extraction was the most common trigger for BRONJ in 2006 (75% of cases) and in 2008 (41.1%) (Urade et al. 2011). Likewise, tooth extraction was the most common trigger for BRONJ in other country (67.0%) (Filleul et al. 2010). In addition, among cases of surgical treatment for stage 2 BRONJ in 2015, tooth extraction was the most common trigger (48.1%), followed by apical periodontitis (13.5%) and marginal periodontitis (10.8%) (Fig. 4) (Shibahara et al. 2018). Because the teeth had been extracted due to marginal periodontitis or apical periodontitis, dental infections might have resulted in BRONJ. The incidence of BRONJ with general dental treatment is believed to be low, but its incidence increases with bone-invasive dental treatments such as tooth extraction, dental implant surgery and apical/periodontal surgery (Advisory Task Force on Bisphosphonate-Related Ostenonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons 2007).
Among 4,797 cases of BRONJ, including 3,393 women, the most common primary disease associated with BP administration was malignant neoplasm (46.5%) including of the breast, prostate, and lung, followed by osteoporosis including its prevention (45.3%) (Fig. 5) (Shibahara et al. 2018).
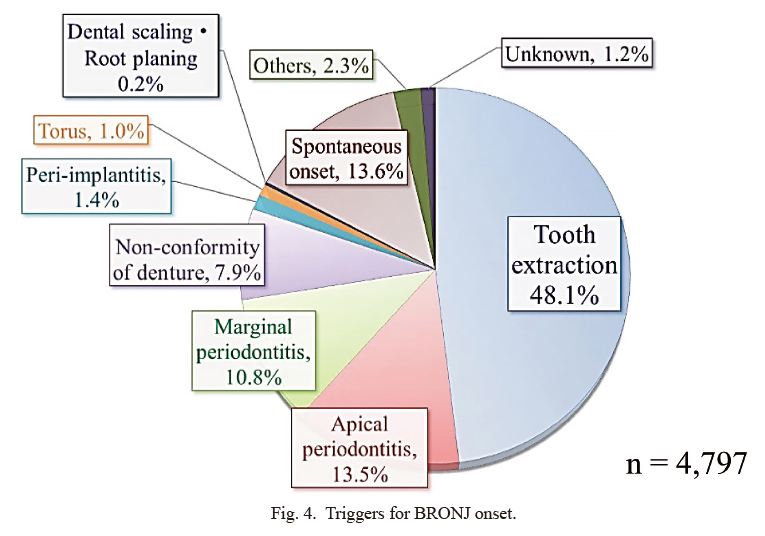
Triggers for BRONJ onset.
The commonest trigger for onset of BRONJ was tooth extraction (48.1%), followed by apical periodontitis (13.5%). The data are taken from the published paper (Shibahara et al. 2018).
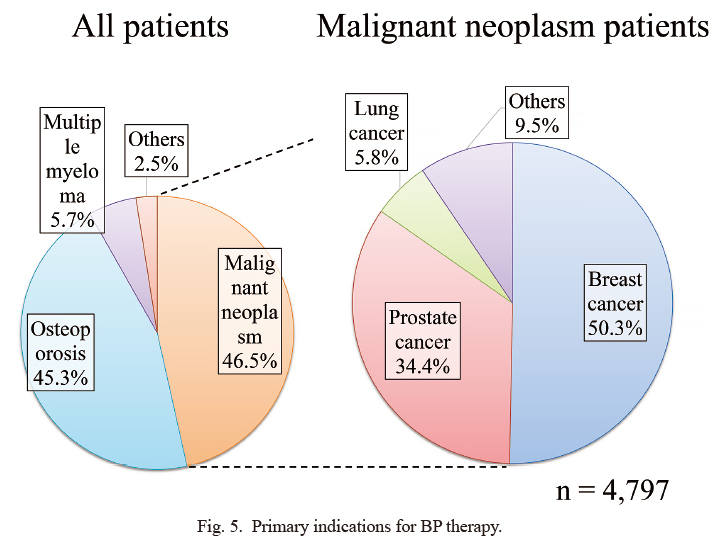
Primary indications for BP therapy.
The most common primary diseases that were indications for bisphosphonate therapy were malignant neoplasms (46.5%), followed by osteoporosis (including prevention; 45.3%). This figure was reproduced from the published paper (Shibahara et al. 2018) with permission.
BPs are classified according to the side chain on the carbon atom of the basic P-C-P structure into first-generation BPs, such as etidronate, second-generation BPs, such as alendronate, ibandronate, and pamidronate, and third-generation BPs, such as risedronate and zoledronate (Fig. 6). The nitrogen-containing BPs show the stronger antiresorptive activities compared with etidronate (Yamaguchi et al. 2018).
BPs have strong affinity for hydroxyapatite so that about 50% of given BPs are accumulated into the bone matrix and are retained there for a long time. The half-life of alendronate in the bone tissue is believed to be 10 years (Khan et al. 1997). BPs that have settled in the bone tissue are incorporated into osteoclasts through the resorption process, which in turn impairs the function of osteoclasts (Fig. 7) (Fleisch 1998). In fact, nitrogen-containing BPs inhibit the mevalonate metabolic pathway, the cholesterol synthetic pathway, and they disrupt the localization of various signaling factors on the cell membrane and their migration to their target proteins, thus disrupting formation of the cytoskeleton (Fleisch 2002). As a result, the osteoclast cytoskeleton breaks down, and the ruffled border disappears, inducing apoptosis.
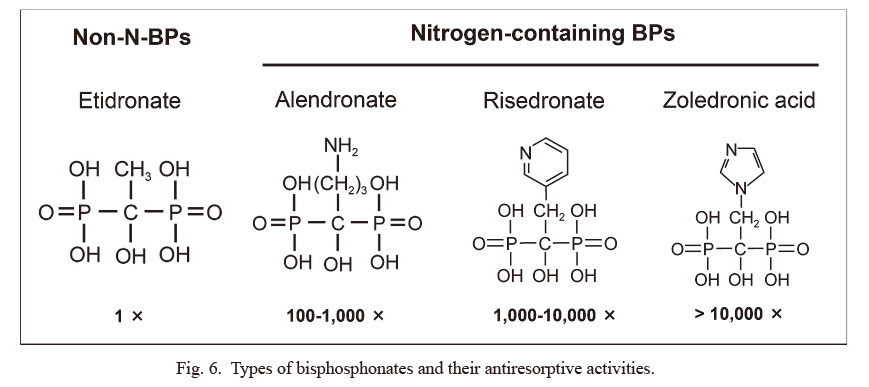
Types of bisphosphonates and their antiresorptive activities.
Bisphosphonates (BPs) are classified according to the side chain on the carbon atom of the basic P-C-P structure into first-generation BPs (etidronate), second-generation BPs (alendronate), and third-generation BPs (risedronate and zoledronate). Each value at bottom indicates the relative intensity of the antiresorptive activity compared with etidronate (Yamaguchi et al. 2018).
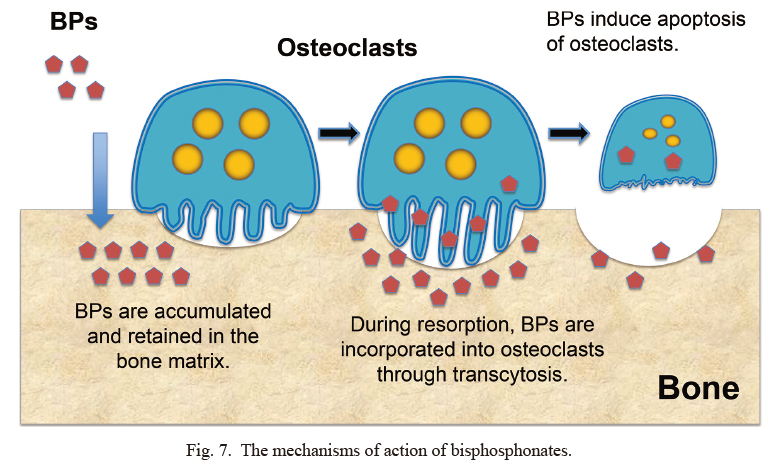
The mechanisms of action of bisphosphonates.
Bisphosphonates (BPs) are accumulated and retained in the bone matrix, and the retained BPs are incorporated into osteoclasts through transcytosis. As a result, BPs inhibit resorption of bone by inducing apoptosis of osteoclasts.
RANKL is one of the most important cytokines regulating the differentiation, function, and survival of osteoclasts. RANKL is produced by osteoblasts and mesenchymal cells (Fig. 8), and it promotes osteoclast differentiation and function when it binds to RANK expressed in osteoclast precursors (Yasuda et al. 1998). At the same time, osteoblasts and mesenchymal cells produce the RANKL decoy receptor osteoprotegerin (OPG), which inhibits binding of RANKL to RANK, thus suppressing osteoclast differentiation and function (Yasuda et al. 1998). The differentiation and function of osteoclasts are therefore regulated by the balance between RANKL and OPG produced by osteoblasts and mesenchymal cells. Hence, a RANKL neutralizing antibody was developed as a drug to suppress osteoclastic bone resorption.
The fully human antibody to RANKL (denosumab) that is in current use has powerful antiresorptive effects, acting to increase bone density and prevent fractures in osteoporosis patients (Bekker et al. 2004). Denosumab has also been shown to reduce the occurrence of skeletal-related events such as pathological fractures, spinal cord compression, or hypercalcemia in cases of metastatic bone cancer (Fizazi et al. 2011). It is currently approved in Japan for use in patients with bone lesions due to osteoporosis or multiple myeloma and bone lesions due to solid tumor metastasis. RANKL antibody not only suppresses the function of mature osteoclasts in the same way as BPs, but it also suppresses the differentiation of osteoclasts that have matured from osteoclast precursors expressing RANK (Fig. 9).
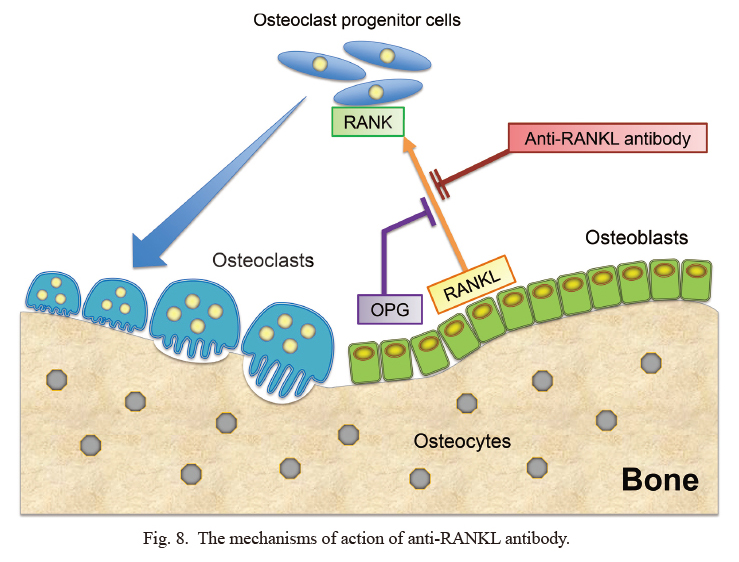
The mechanisms of action of anti-RANKL antibody.
Anti-RANKL antibody not only suppresses the function of mature osteoclasts, but it also suppresses the differentiation of osteoclasts that have matured from osteoclast precursors expressing RANK. OPG binds to RANKL, thereby preventing the interaction between RANKL and RANK. Thus, OPG inhibits the differentiation of osteoclasts. Osteocytes, buried in the formed bone tissue, are derived from osteoblasts.
OPG, osteoprotegerin; RANK, receptor activator of NFκB; RANKL, RANK ligand.
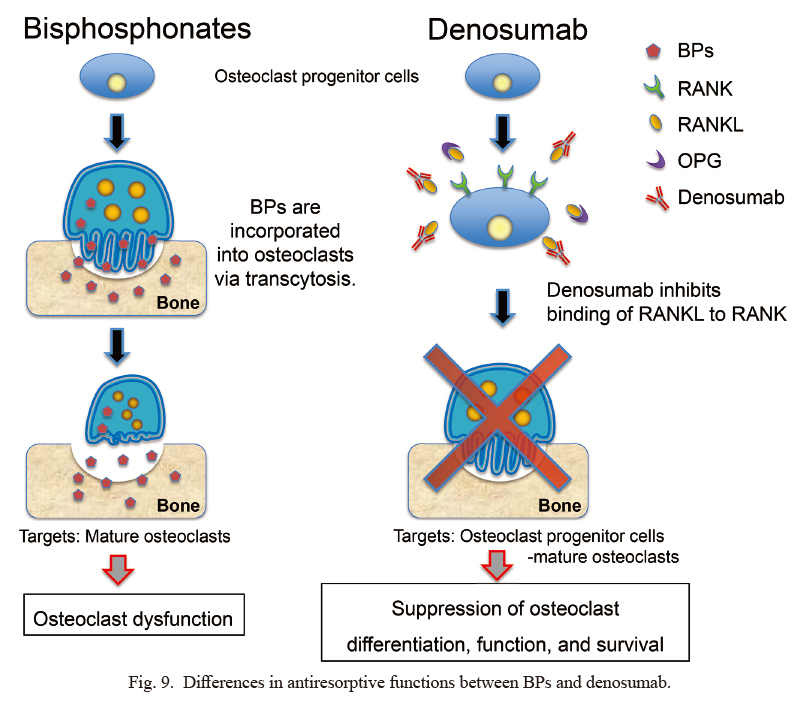
Differences in antiresorptive functions between BPs and denosumab.
This figure is constructed based on Baron et al. (2011).
BPs, bisphosphonates; OPG, osteoprotegerin; RANK, receptor activator of NFκB; RANKL, RANK ligand.
The antiresorptive mechanisms of BPs and denosumab are completely different (Baron et al. 2011). As already noted, BPs, buried in the bone matrix, are incorporated into osteoclasts during the process of bone breakdown, and BPs disrupt the functions of the cytoskeleton and accelerate apoptosis, thus suppressing resorption through osteoclast dysfunction. Denosumab, on the other hand, suppresses the function of the molecule RANKL, which is essential for osteoclast differentiation and function, thus inhibiting resorption through suppression of osteoclast differentiation, function, and survival (Fig. 8). The fact that these two drugs with differing antiresorptive mechanisms induce ONJ suggests that the decrease in the bone turnover rate may represent a risk factor for ONJ. Thus, among patients treated with a powerful antiresorptive drug, ONJ is readily triggered by infections or other causes. From the pharmacokinetics of BPs and denosumab (Yamaguchi et al. 2018), it is conceivable that jawbone disorders due to BPs may be irreversible, but those due to denosumab may be reversible. However, Niimi et al. (2018) reported rebound-associated vertebral fractures after discontinuation of denosumab. This serious problem is still uncertain.
ARONJ presents with various clinical symptoms depending on the progress of the condition, and findings from imaging are essential to grasp the extent of the condition. Initially when BRONJ was reported (Marx 2003), appropriate treatment methods were not adequately established because the condition was not fully understood, and for this reason, there was often inconsistency in the understanding of BRONJ between the doctors who prescribed BPs and the dentists who treated ONJ. Unfortunately, the confusion has yet to be resolved in Japan, and the number of ARONJ cases is increasing. Perhaps because the 2010 position paper rather exaggerated the fear of ONJ and BPs (Yoneda et al. 2010), there seems to have been a period when many dentists were reluctant to carry out dental treatment. In the 2017 position paper (Yoneda et al. 2017), it was clarified that if a tooth which has been infected is left not only prior to BP administration but also during administration, the tooth could become a source of infection and provoke ONJ. Invasive dental treatments need attention, but if it is non-invasive treatments, including oral management, should be carried out following careful examination of the patient’s condition and the details of the treatment.
There are differences of opinions among prescribing doctors, pharmaceutical companies, and dentists regarding a drug holiday during invasive dental treatment or during treatment for ARONJ, and a full consensus has yet to be reached. The opinion of doctors is that though a drug holiday for the treatment when ARONJ has occurred is acceptable if the patient’s condition permits it, preventive withdrawal of the drug in patients without ONJ is pointless. Similarly, recent papers in Japan suggest no need of drug discontinuation before tooth extraction to prevent ONJ (Hasegawa et al. 2017). It would be highly desirable for dentists to acquire accurate understanding of the mode of action of antiresorptive drugs and the primary diseases for which they are indicated, and to consider the risks of ARONJ and the benefits of bone fracture prevention from antiresorptive drugs.
A major difference between the 2017 position paper (Yoneda et al. 2017) and the previous position paper (Yoneda et al. 2010) was the approach to treating stage 2 MRONJ (Table 2). Until then, the drug had been withdrawn whenever possible, and the main supportive therapy had been local cleansing and administration of antibacterial drugs (regular scaling with oral cleansing using 0.05% chlorhexidine, 0.2% benzethonium chloride, and 1% povidone iodine). In 2017, the effectiveness of proactive surgical treatment was stressed (Yoneda et al. 2017). If there were sequestra in lesions, or if there were mobile teeth that should be extracted, these could be sources of infection and make ARONJ progress; thus, they should be removed. A survey of stage 2 cases (866 cases) in Japan found that, in many cases, surgical treatment has been provided after supportive therapy, mainly oral management during a mean of 6.6 months (Shibahara et al. 2018). In any case, it is difficult to cure ARONJ by supportive therapy alone, and it is preferable to shift to surgical treatment at an opportune time.
Where a drug holiday is possible, it is preferable to start before invasive dental procedures (about two months). The drug holiday should be continued after the procedure until bone recovery has been achieved (about two months). If a drug holiday is not indicated due to the patient’s general condition, it would be advisable to carry out appropriate invasive dental treatment (pre- and postoperative administration of antibacterial drugs, removal of bony spines, and complete closure of the wound) when the blood concentration of the antiresorptive drug is relatively low. In addition, based on the pharmacokinetics of BPs and denosumab, it is likely that BPs prolong bone healing because they are retained in the apatite of bony tissue for a long time (Khan et al. 2017).
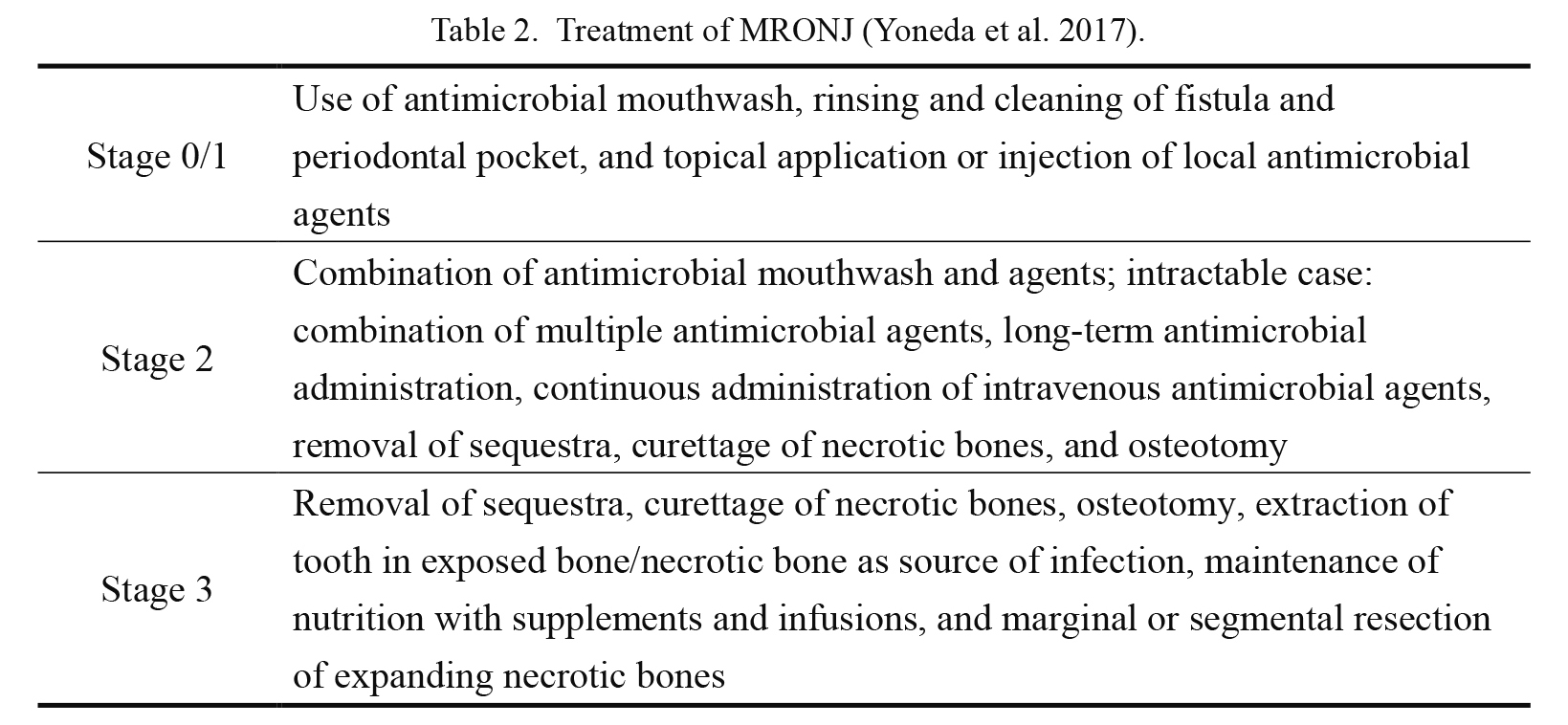
Treatment of MRONJ (Yoneda et al. 2017).
Isolated sequestra are removed without exposing bones outside lesions, regardless of disease stage. A tooth with symptoms in exposed necrotic bones is extracted; extraction itself is unlikely to exacerbate necrosis.
It has been reported that half of the cases of latent ARONJ (stage 0) progress to stages 1-3, and stage 0 is thus important from the point of view of early detection (Fedele et al. 2010). Undue conservation of the teeth with poor prognosis can spread infection and may lead to the progression of ARONJ. The approach of avoiding tooth extraction due to excessive fear for ONJ should be reconsidered.
With regard to the risk factors that can cause ARONJ, risk factors were recognized in 30.6% of cases, in which the highest proportion were anticancer drugs (55%), followed by corticosteroids (32%) (Filleul et al. 2010). Moreover, in surgical treatment for stage 2 BRONJ (Shibahara et al. 2018), a risk factor was recognized in 67.1% of cases, in which the most frequent was anticancer drugs (26.0%), followed by corticosteroids (23.6%) (Fig. 10) (Shibahara et al. 2018).
The risk factors for ARONJ onset can be broadly divided into local factors, systemic factors, hereditary factors, life history, and concomitant drugs. Local factors include bone-invasive dental treatment such as tooth extraction or dental implants, occlusal or oral hygiene status, and dental infection. Onset due to decubitus ulcer from ill-fitting dentures or prostheses and spontaneous onset due to excessive bite force have been reported (Yoneda et al. 2017), and the importance of oral management by dentists has been reaffirmed. In addition, it is important to understand the type of BPs, primary disease, administration route, dosage, and administration period. Systemic factors include cancer, diabetes mellitus, rheumatoid arthritis, renal dialysis, anemia, and Paget’s disease of bone. With cancer, the risk is high because multiple risk factors can apply, particularly because there is lowered immunity due to the effects of anticancer treatment such as anticancer drugs or hormone therapy. Anticancer drugs that suppress bone marrow cause conditions with lowered immunity such as anemia or leukopenia and increase susceptibility to infection. Methotrexate and corticosteroids are believed to cause secondary osteoporosis. Corticosteroids are a risk factor for aseptic osteonecrosis and induce both acceleration of bone resorption and suppression of ossification. They also increase susceptibility to infection and are thus considered a major risk factor.
In Japan, the primary disease of many ARONJ patients is osteoporosis. Every drug used for osteoporosis will have to be investigated for the risk of ARONJ or MRONJ. In addition, establishing the method of treatment and prevention for MRONJ is an urgent task. It is also important to ensure the proper coordination between medicine and dentistry so that patients with cancer or osteoporosis receive the appropriate dental treatment.
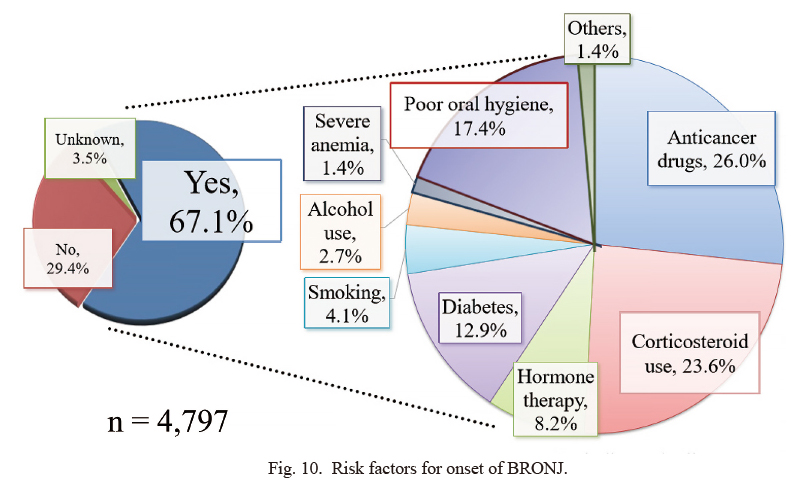
Risk factors for onset of BRONJ.
The incidence of risk factors, such as anticancer drug therapy and corticosteroid therapy, was 67.1%. The data are taken from the published paper (Shibahara et al. 2018).
We have to consider the benefits (efficacy) and risk (ONJ) of BP administration to avoid femoral fracture. Doctors should understand the risk of ONJ due to antiresorptive drugs and encourage dental treatment even during antiresorptive drug prescription. Furthermore, it is desirable for dentists to have an accurate understanding of the risk of MRONJ so that they can proceed with dental treatment for patients treated with antiresorptive drugs. Thus, closer collaboration between dentists, prescribing doctors, and pharmacists is of the utmost importance to prevent developing MRONJ.
The author would like to thank Dr. Akira Yamaguchi (Oral Health Science Center, Tokyo Dental College, Japan) for helpful discussion and encouragement.
The author declares no conflict of interest.