2019 Volume 248 Issue 1 Pages 13-17
2019 Volume 248 Issue 1 Pages 13-17
Synovial fat deposition, also known as lipoma arborescens, is a rare articular disorder with villous synovial proliferation, commonly seen in the knee. We explored the relationship between the degree of synovial fat deposition on the magnetic resonance imaging (MRI) and the severity of degenerative joint disorder, also called osteoarthritis, on plain radiography. The enrolled patients underwent MRI with a 0.4T permanent magnetic unit in a single institution over a 9-month period. The indications of MRI were chronic knee disorder of non-specific cause. Patients with minor trauma were also included. Consecutive 1,091 knees of 1,075 patients were assessed for the degree of synovial fat deposition on MRI and the severity of degenerative joint disorder on plain radiography. The degenerative joint disorder was graded by radiographic features obtained within one month from MRI using Kellgrene-Lawrence (K-L) scores. MRI features of synovial fat deposition were classified as none, mild and severe. Synovial fat deposition was identified in 30 knees of 29 patients (2.7%) (11 men and 18 women; aged from 25 to 86 years, one patient with bilateral lesions): one female patient with osteoarthritis secondary to rheumatoid arthritis and 28 patients with degenerative joint disorder. The K-L grade was 4 in the case of rheumatoid arthritis. There was a moderate positive correlation between the K-L grade and fat deposition grade (correlation coefficient: 0.59, p < 0.001). Thus, synovial fat deposition was noted in the advanced degenerative joint disorder. We propose that fat deposition represents a nonspecific secondary phenomenon of degenerative joint disorder.
Benign lipomatous lesions may occur focally in a joint or a tendon sheath, or they may be diffuse with villous proliferation of the synovium. The first type, synovial lipoma, is a true neoplasm and its development is thought to be unrelated to any other joint pathology, reflecting a characteristic neoplastic nature. The second type, synovial fat deposition or “lipoma arborescens” is a rare articular disorder consisting of villous synovial proliferation that most commonly occurs in the knee joints (Feller et al. 1994). Its cause is unknown, but it has been known as a somewhat non-specific phenomenon that is most commonly observed in the elderly. Hallel et al. (1988) suggested that the lesion be called villous lipomatous proliferation of the synovial membrane, because the designation of lipoma arborescens implied a tumor (Hallel et al. 1988; Murphey et al. 2004). Myhre-Jensen (1981) reported two cases of lipoma arborescens that is thought 0.3% of the lipomas in those days. With the advent of magnetic resonance imaging (MRI), the qualitative analysis of synovium became possible, although its clinical features have not been well defined.
The objective of this study is to explore the relationship between the degree of synovial fat deposition and the severity of degenerative joint disorder (also known as osteoarthritis). In this study, we carefully distinguished synovial fat deposition from extrasynovial fat deposition that is considered to represent normal findings; namely, we used two orthogonal planes, sagittal and coronal images to exclude extrasynovial fat deposition that is usually prominent laterally. We thus conclude that the synovial fat deposition is associated with chronic knee disorder typically secondary to degenerative joint disorder.
This study was approved by the Institutional Review Board of Iwate Medical University School of Medicine, and the requirement for informed consent was waived for this retrospective analysis with no influence on the clinical outcome. We reviewed MRI of the knee in 1,237 joints in patients aged 20 years and older (Fig. 1). Indications of MRI were chronic knee pain of non-specified cause. Patients with minor trauma, i.e., suspected trauma-related disorder without history of major trauma representing well-documented fracture, dislocation, or injury of the major knee ligaments and tendons, were also included since it was a common chronic joint disorder related to trauma or degenerative joint disorder. All MRI data were obtained during a 9-month period at Towada-East Clinic in Towada, Aomori, Japan. We excluded 146 joints with no plain radiography of the knee, including at least anteroposterior and lateral views, obtained within 1 month from MRI. We also excluded acute or subacute major trauma with displaced or comminuted fractures with soft tissue changes (7 joints), the status post intraarticular surgical procedure (4 joints), and MRI obtained more than twice during the study period (10 joints). In total, 1,091 consecutive joints of 1,075 patients were included, and synovial fat deposition was assessed. The ages of the patients ranged from 25 to 86 years (median 64.5 years); 412 were men and 679 were women (Fig. 1).
Plain radiography obtained within 1 month of MRI was evaluated for the presence of degenerative joint disorder by means of Kellgrene-Lawrence (K-L) grading (grades 0-4). MRI included coronal and sagittal T1-weighted (TR 340 ms, TE 19 ms) and coronal and sagittal T2-weighted (TR 3,500 ms, TE 90 ms) spin-echo magnetic resonance sequences of the knee obtained by a 0.4T permanent magnet unit (APERTO, Hitachi, Tokyo). Both plain radiography and MRI were evaluated by one of the authors with more than 30 years of experience. Magnetic resonance images were evaluated for synovial fat deposition and classified as grade 0 (no synovial fat), grade 1 (mild synovial fat deposition with no joint expansion) (Fig. 2), or grade 2 (severe synovial fat deposition with joint expansion) (Fig. 3). Such synovial proliferation with fat deposition was mainly seen in the suprapatellar pouch, but the posterior aspect of the synovial tissue was also affected in diffuse synovial proliferation and such involvement of the popliteal region was recorded. Lobulated fat on the lateral aspect of the suprapatellar region, representing extrasynovial fat, was distinguished from synovial fat deposition by two orthogonal planes, sagittal and coronal images.
We assessed the correlation between K-L grade on plain radiography and fat deposition grade on MRI using Statcel 4 software (OMS publishing Inc., Saitama, Japan) and Microsoft Excel 2010 (Microsoft, Chicago). Spearman’s rank correlation was used to evaluate the association between the severity of K-L grade and synovial fat deposition (Fig. 1).

Flow diagram of patient inclusion and exclusion, and the relation between K-L grade and synovial fat deposition in the knee joint.
This study includes 1,237 knee joints evaluated by means of MRI. The indication of MRI is chronic knee pain of non-specified cause, and Kellgrene-Lawrence (K-L) grading on plain radiography and synovial fat deposition grade on MRI are evaluated. And the correlation between synovial fat deposition and osteoarthritic grade was assessed among 1,091 knees.
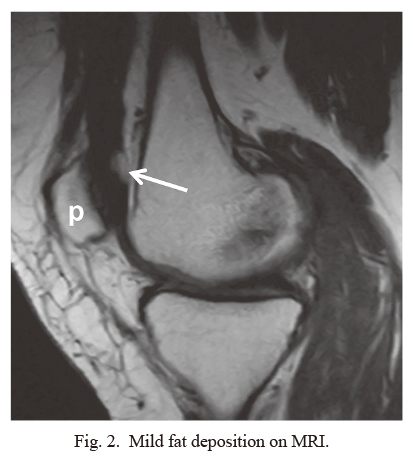
Mild fat deposition on MRI.
Mild synovial fat deposition without joint swelling (grade I lesion; 65-year-old woman). Sagittal T1-weighted image reveals fat nodules in the posterior wall of the suprapatellar pouch (arrow).
p, patella.

Severe fat deposition on MRI.
Severe synovial fat deposition with joint swelling (grade II; 57-year-old man). Sagittal T1-weighted imaging reveals fat deposition in the suprapatellar pouch and the posterior aspect of the knee joint (arrows). The suprapatellar pouch is expanded by the synovial proliferation with fat deposition. T1-weighted image also shows the osteophytes originated from femur and tibia.
Arrowheads indicate fatty marrow in the ossification of degenerated articular cartilage and asterisks (*) indicate fatty marrow of the osteophyte.
p, patella.
The number of the subjects is summarized in Fig. 1. Among 1,091 joints of 1,075 patients, K-L grading was grade 0 in 540 joints, grade 1 in 216 joints, grade 2 in 143 joints, grade 3 in 118 joints, and grade 4 in 74 joints. There was no significant sex difference in the prevalence of synovial fat deposition: 2.7% (11/412 joints) in men vs. 2.8% (19/679 joints) in women. Histological correlation was not obtained in any case since conservative treatment was selected.
MRI synovial fat grading was grade 0 (no fat) in 1,061 cases, grade 1 (mild fat deposition) in 16 joints, and grade 2 (severe fat deposition) in 14 joints (Fig. 4). Among the patients with fat deposition in 30 joints of 29 patients; 11 were men and 18 were women. Their ages ranged from 25 to 86 years (median 64.5 years). In one woman 79-year-old, fat deposition was bilateral.
The indications of MRI studies in joints with synovial fat deposition were degenerative joint disorder in 29 joints, and non-specific arthritis in one joint. The synovial fat deposition grade in this patient with arthritis of non-specific cause was grade 2. In one woman at the age of 25, K-L grade was 3 and fat deposition grade was 2, we could not find any underlying cause of the premature degenerative disorder, suggestive of primary degenerative disorder. One patient revealed history of rheumatoid arthritis representing secondary degenerative disorder (Fig. 5). This fat deposition grade was 2 in this patient. There were no trauma findings in 25 knees of the 30 knees. In the reminder of 5 knees, there was subcutaneous edema at the prepatellar region in 4 knees, and old healed fracture of the patella in one knee.
There was a moderate positive correlation between K-L grade and synovial fat deposition grade (r = 0.59, p < 0.001) (see Fig. 1). The patients with synovial fat deposition were most likely to suffer from either primary or secondary degenerative joint disorder, probably related to minor trauma. The fat deposition was evident in the suprapatellar pouch in all the subjects, as shown in Figs. 2 and 3. The posterior aspect of the knee joint was involved in 6 knees, representing more diffuse synovial process (Fig. 3).

Age and sex distribution of synovial fat deposition.
The ordinate indicates number of knees with synovial fat deposition (total 30 knees of 29 patients), including a 79-year-old woman with bilateral fat deposition.

Synovial fat deposition in a patient with rheumatoid arthritis.
Fatty degeneration associated with synovial proliferation in chronic phase of rheumatoid arthritis (85-year-old woman). Sagittal T1-weighted imaging reveals fat deposition in the regions of synovial proliferation in the suprapatellar pouch and the posterior aspect of the knee joint.
p, patella.
Synovial fat deposition, lipoma arborescens, was believed to be a non-neoplastic synovial lesion. It was thought to be a reactive synovial change, and some authors prefered the term “villous lipomatous proliferation of the synovial membrane” (Hallel et al. 1988; Ryu et al. 1996). Case studies and case series including a small number of cases have been reported (Doyle et al. 2002; Howe and Wemger 2013).
In cases of lipoma arborescens, the lesion was usually monoarticular, but in 20% of cases it was polyarticular (Arzimanoglu 1957). Although occurrence in the knee accounted for approximately 20% of cases, particularly in the suprapatellar pouch, any joints including the shoulders, elbows, hips, and ankles may have been affected (Soler et al. 1998; Nisolle et al. 1999; Bejia et al. 2005; Pandey and Alkhulaifi 2006; Babar et al. 2008). Bursae may also be involved. When the suprapatellar pouch was isolated by a complete suprapatellar plica, the isolated bursa may be prone to synovitis, including synovial chondromatosis, pigmented villonodular synovitis, and lipoma arborescens (Bejia et al. 2005).
MRI characteristics of fat deposition included intra-articular masses containing fat lobules surrounded by fluid (Coventry et al. 1966; Armstrong and Watt 1989; Feller et al. 1994; Kransdorf and Murphey 1997; Vilanova et al. 2003). A large amount of joint effusion was usually associated, and the amount of effusion may significantly affect imaging features. MRI showed villous lipomatous deposition with signal intensity of fat on T1-weighted and T2-weighted images. The fat deposition and unique frond-like architecture of lipoma arborescens often permitted a specific diagnosis based solely on imaging findings (Ryu et al. 1996; Vilanova et al. 2003). Chemical shift MRI artifact may have been associated at the interface between the lesion and the effusion. Diffuse synovial thickening with a characteristic fat signal on MRI was suggestive of lipoma arborescens. Intravenous administration of gadolinium-based contrast material may have contributed to the depiction of vascular synovium (Coventry et al. 1966; Reiser and Naegele 1993; Kransdorf and Murphey 1997; Ragab et al. 2007; Chae et al. 2009).
The etiology of lipoma arborescens is not known. It is believed to be non-neoplastic and represents a synovial reaction to inflammatory or traumatic stimuli (Narvaez et al. 2001). Some cases may develop de novo, while the others may be associated with synovitis secondary to osteoarthritis, rheumatoid arthritis, or trauma; namely, this phenomenon may be reactive or inflammatory (Kransdorf and Murphey 1997). Although such synovial proliferation is a typical feature of rheumatoid arthritis, the most commonly associated condition is considered to be the degenerative joint disorder, osteoarthritis (Hallel et al. 1988; Armstrong and Watt 1989; Feller et al. 1994; Soler et al. 1998; Nisolle et al. 1999; Murphey et al. 2004). In the present study, we found a significant correlation between the severity of osteoarthritis and the degree of fat deposition.
On the other hand, some investigators speculated that lipoma arborescens may contribute to the development of osteoarthritis (Hallel et al. 1988; Ryu et al. 1996). One retrospective review suggested that primary lipoma arborescens of the knee may induce development of early osteoarthritis if prompt synovectomy was not performed (Natera et al. 2015). Although the severity of osteoarthritis seemed to be correlated with disease duration, aspects of the accompanying degenerative processes remained unclear with regard to cause and effect relationships. Specifically, it was not known if osteoarthritis exacerbated fat deposition or if fat deposition exacerbated osteoarthritis. The lesion was considered totally curable, but underlying persistent disease may have aggravated inflammatory processes and caused recurrent disease (Kamaci et al. 2015). Correlation with fat metabolism is also not well elucidated, and it may be worth investigated in the future research.
This study was a retrospective review of cases seen at a single institution and thus may not have accurately reflected the wider incidence of synovial fat deposition. The definitive reason for the apparent high prevalence of synovial fat deposition in the population investigated was not known. The study also had some limitations, including a lack of surgical correlation because most of the patients were of relatively older age and undergoing conservative treatment for their degenerative joint disorders. However, MRI findings of knee lesions were proved to be related based on the previous case series and reports (Armstrong and Watt 1989; Feller et al. 1994; Ryu et al. 1996; Soler et al. 1998; Howe and Wemger 2013). The quality of the magnetic resonance images used was also limited because they were generated by a permanent magnet unit with medium field strength. However, we believe that the resolution of MRI was still high enough to assess gross morphological changes that we dealt with. Intra-observer and inter-observer variabilities were not assessed. Still, the large number of cases and the observer with adequate experience added some validity to our observations. We believed the overall observations made in the study were still valid to conclude the relationship between synovial fat deposition and degenerative joint disorder.
In conclusion, synovial fat deposition may be a non-specific phenomenon secondary to degenerative joint disorder. Moreover, the degree of synovial fat deposition and the severity of degenerative joint disorder appears to be moderately correlated.
The authors declare no conflict of interest.