2019 Volume 248 Issue 3 Pages 169-179
2019 Volume 248 Issue 3 Pages 169-179
Extensive use of Wi-Fi has contributed to radiofrequency electromagnetic radiation (RF-EMR) pollution in environment. Various studies have been conducted to evaluate the effect of RF-EMR emitted by Wi-Fi transmitter on male reproduction health. However, there are conflicting findings between studies. Thus, this review aims to elucidate the possible effects of 2.45 GHz Wi-Fi exposure on both animal and human male reproductive system. A computerized database search performed through MEDLINE via Ovid and PUBMED with the following set of keywords: ‘Wi-Fi or WiFi or wireless fidelity or Wi-Fi router or WiFi router or electromagnetic or radiofrequency radiation’ AND ‘sperm or spermatozoa or spermatogenesis or semen or seminal plasma or testes or testis or testosterone or male reproduction’ had returned 526 articles. Only 17 studies conformed to pre-set inclusion criterion. Additional records identified through Google Scholar and reviewed article further revealed six eligible articles. A total of 23 articles were used for data extraction, including 15 studies on rats, three studies on mice, and five studies on human health. Sperm count, motility and DNA integrity were the most affected parameters when exposed to RF-EMR emitted by Wi-Fi transmitter. Unfortunately, sperm viability and morphology were inconclusive. Structural and/or physiological analyses of the testes showed degenerative changes, reduced testosterone level, increased apoptotic cells, and DNA damage. These effects were mainly due to the elevation of testicular temperature and oxidative stress activity. In conclusion, exposure towards 2.45 GHz RF-EMR emitted by Wi-Fi transmitter is hazardous on the male reproductive system.
Since several decades ago, the world had witnessed a rapid evolution in communication technology. Wireless fidelity (Wi-Fi) has emerged as the preferred route of internet communication and connectivity. Concurrently, Wi-Fi signal operates in an unlicensed spectrum range of 2.45 to 5 GHz (Zhang et al. 2015) which minimizes its operation cost. For this reason, Wi-Fi has become a daily necessity and is widely used in various devices. Although it tremendously transforms human life for the better, the extensive use of Wi-Fi has led to the proliferation of radiofrequency electromagnetic radiation (RF-EMR) in public spaces (Teixeira and Hasan 2016). This phenomenon consequently has raised public concern regarding the potential health effects of Wi-Fi on human.
The RF-EMR emitted from Wi-Fi transmitter involves whole body exposure (Wu et al. 2010; Banaceur et al. 2013) while mobile phone involves localized RF-EMR exposure (Ozorak et al. 2013; Grell et al. 2016; Jamaludin et al. 2017). RF-EMR is classified as non-ionizing radiation and theoretically is unable to induce ionization of cellular atoms and molecules. Therefore, the putative damaging effects of Wi-Fi on biological tissue could be attributable to the thermal mechanism (Coulton et al. 2004; Foster and Colombi 2017). However, recent studies had expanded this hypothesis to further encompass non-thermal effects (Kibona 2013; Adams et al. 2014). This latter effect is suspected to play a major role in causing cell damage via the oxidative stress pathway (Nazıroğlu et al. 2013; Tök et al. 2014; Yakymenko et al. 2016).
The measurement of the rate energy absorbed in the presence of an electromagnetic field over a volume of tissue is represented as specific absorption rate (SAR) and is commonly expressed in Watts per kilogram (W/kg) (Hochwald et al. 2014). According to the Federal Communications Commission (FCC), the whole body safe exposure to this form of energy should never exceed 0.08 W/kg or 1.6 W/kg for any body tissue (IEEE, The Institute of Electrical and Electronics Engineers 1991). Despite this recommendation, the World Health Organization (WHO) has recommended a much higher SAR limit which is 4 W/kg (Wu et al. 2010). Wi-Fi transmitter that emitting SAR below the aforementioned threshold is considered safe for use by the public in an uncontrolled environment (IEEE 1991).
Studies have found that testes are the most sensitive organ to RF-EMR emitted by Wi-Fi devices (Dasdag et al. 2015; Othman et al. 2017). The testes abnormality is noticed through significant changes to sperm count, viability, motility, morphology and percentage of sperm with severe DNA damage (Avendano et al. 2012; Shokri et al. 2015) when exposed to 2.45 GHz Wi-Fi frequency (Saygin et al. 2016). Interestingly, some studies have reported that only sperm count and motility were affected while other sperm parameters remained normal (Mahmoudi et al. 2015). Therefore, the effects of Wi-Fi on the male reproductive system remained elusive. This systematic review aims to evaluate the effects of Wi-Fi on various aspects of the male reproductive system and to determine the source of discrepancies between previous studies.
A computerized literature search was conducted on the original research articles reporting the effects of Wi-Fi exposure on the male reproductive system. The literature research was conducted through MEDLINE via Ovid and PUBMED databases with the following keywords: ‘Wi-Fi or WiFi or wireless fidelity or Wi-Fi router or WiFi router or electromagnetic or radiofrequency radiation’ AND ‘sperm or spermatozoa or spermatogenesis or semen or seminal plasma or testes or testis or testosterone or male reproduction’. Articles published between 1946 and November 2018 were included in the search. In order to search for additional literature that might have been missed during the database search, additional records were identified through Google Scholar using similar set of keywords and from the reference list of review article retrieved from the initial search (Kesari et al. 2018).
Study inclusion and exclusion criteriaThe eligible articles were reviewed independently by two authors (FHF and NHI) based on the following criteria: only full-length original articles published in English were included; reported the effects of Wi-Fi on sperm quality which include sperm count, motility, viability, morphology and/or DNA damage status in human or in rodent; reported the changes of testes histology; pro- and antioxidant status of the testes and/or male reproductive hormone due to Wi-Fi exposure; only studies which used the frequency of 2.45 GHz Wi-Fi radiation from Wi-Fi devices or generated from a specialized chamber were considered; radiation from mobile phones is excluded because similar topics were previously reviewed.
Data extraction and managementSelection of the study involved two steps. In the first step, the titles and abstracts of the articles were screened. The studies that did not meet the inclusion criteria were excluded. In the second step, the full text of the selected articles was retrieved and filtered based on the same inclusion and exclusion criteria. Discrepancies of opinions regarding the eligibility of an article between the two reviewers were resolved by consulting two authors, S.F.I. and K.O.
The sample size, strain of animal, age of the human and animal involved, duration of exposure and exposure setting were extracted. Besides, inclusion and exclusion criteria for human semen sample, movement restriction in the animal study as well as SAR and/or power density value applied in the study were also recorded.
The initial literature search retrieved 526 unique articles, of which 191 articles were from MEDLINE and 335 articles from PubMed. Another 191 articles were removed due to duplication. Subsequently, 315 articles were excluded after reviewing the titles and abstracts. Full papers were obtained for the remaining 20 articles and a thorough reviewing process was conducted (Fig. 1). Three articles were further excluded as the frequency of the RF-EMR generator applied in the study was not mentioned. On the other hand, six additional articles were retrieved from Google Scholar and one was cited by a review article (Kesari et al. 2018). One article was excluded because it was not written in English. In total, 23 eligible papers were reviewed for data extraction.

Flow chart of the literature search.
Animal study: Of the 23 eligible articles, 18 reported on the effect of 2.4 GHz Wi-Fi radiation rodents of which 15 studies used Wistar Albino and Sprague Dawley rats (Table 1) and another three used involved Swiss albino and BALB/c mice (Table 2).
The age of the animal used in the studies varied, ranging from prenatal age (Ozorak et al. 2013), weanlings (14 and 21 days for rats) (Simaiova et al. 2018), early adults, i.e. 6 to 8 weeks for mice (Atasoy et al. 2013; Saygin et al. 2016; Delavarifar et al. 2018; Jonwal et al. 2018) and 10 weeks for rats (Kesari and Behari 2010; Kumar et al. 2011). Other studies used adult mice and rats aged 12 to 24 weeks (Saygin et al. 2011; Shahin et al. 2014; Mahmoudi et al. 2015; Akdag et al. 2016; Bilgici et al. 2018).
The generator for the 2.45 GHz Wi-Fi radiation were derived from various sources which include horn antenna (Kesari and Behari 2010; Kumar et al. 2011; Shahin et al. 2014; Jonwal et al. 2018), monopole antenna (Saygin et al. 2016; Bilgici et al. 2018), half-wave dipole antenna (Saygin et al. 2011; Ozorak et al. 2013; Oksay et al. 2014; Akdag et al. 2016), purpose design chamber (Almasiova et al. 2014, 2018; Simaiova et al. 2018), Wi-Fi router (Mahmoudi et al. 2015; Delavarifar et al. 2018), Wi-Fi antenna (Dasdag et al. 2015; Shokri et al. 2015) and Wi-Fi gateway (Atasoy et al. 2013). The studies vary in terms of distance between samples and the generator and duration of exposure. The shortest duration was 2 h/day for 4 days while the longest was 24 h/day for 12 months. On the other hand, 2 m was the furthest distance applied. Some studies described the distance as ‘close contact’ but the actual distance for close contact was not specifically mentioned in the study. Despite the differences in the setting, all the studies reported SAR values below recommendation limits by US FCC and WHO.
Most of the studies defined control or sham group as the group that received no exposure of RF-EMR as the generator was switched off and only received cage restriction stress (Kesari and Behari 2010; Saygin et al. 2011, 2016; Kumar et al. 2011; Atasoy et al. 2013; Ozorak et al. 2013; Almasiova et al. 2014, 2018; Oksay et al. 2014; Shahin et al. 2014; Shokri et al. 2015; Akdag et al. 2016; Bilgici et al. 2018; Jonwal et al. 2018; Simaiova et al. 2018). On the other hand, the sham group in the study done by Mahmoudi et al. (2015) and Delavarifar et al. (2018) were exposed to non-energizing Wi-Fi router which refers to a switched on Wi-Fi router without any data exchange between the linked devices.
Most of the literature consistently demonstrated various degrees of degenerative changes on testes histomorphometry with a parallel appearance of apoptotic cells (Kesari and Behari 2010; Kumar et al. 2011; Saygin et al. 2011; Almasiova et al. 2014, 2018; Shahin et al. 2014; Dasdag et al. 2015; Shokri et al. 2015; Delavarifar et al. 2018; Jonwal et al. 2018; Simaiova et al. 2018) and more prominent DNA damage compared to other organs following RF-EMR exposure (Akdag et al. 2016). Moreover, oxidative stress developed in the testes after RF-EMR exposure as evidenced by increased ROS level, decreased enzymatic and non-enzymatic antioxidant levels and increased lipid and nucleic acid peroxidation products in the testes (Kesari and Behari 2010; Atasoy et al. 2013; Ozorak et al. 2013; Oksay et al. 2014; Shahin et al. 2014; Saygin et al. 2016; Almasiova et al. 2018; Simaiova et al. 2018).
The weight of the testes and accessory sex organs was not significantly affected by RF-EMR exposure (Mahmoudi et al. 2015; Shokri et al. 2015) but the weight of epididymis and seminal vesicle were significantly decreased (Dasdag et al. 2015; Shokri et al. 2015). The exposure also increased testes temperature but did not affect body temperature (Almasiova et al. 2018). In addition, three studies reported a significant decrease in testosterone level (Kumar et al. 2011; Shahin et al. 2014; Jonwal et al. 2018) while one study demonstrated a marginal decrease of testosterone level (Saygin et al. 2016) following RF-EMR exposure emitted by the Wi-Fi transmitter.
Evaluation on the sperm quality showed that the decrease of sperm count, motility, viability and normal morphology occurred following the RF-EMR exposure (Kesari and Behari 2010; Shahin et al. 2014; Dasdag et al. 2015; Shokri et al. 2015). However, Delavarifar et al. (2018) reported an increase in sperm count. Furthermore, a study by Mahmoudi et al. (2015) demonstrated that sperm count and motility were decreased following the exposure but sperm morphology and sperm DNA were not affected. Their findings on the sperm morphology were not similar with the other works of literature but it was noted that it was the only study that had evaluated the effect of 2.45 GHz radiation on the sperm DNA (Mahmoudi et al. 2015).
Human study: Five articles reported the effects of RF-EMR exposure on human subjects, whereby four were experimental studies (Oni et al. 2011; Avendano et al. 2012; Kamali et al. 2017; Ding et al. 2018b) and one was a retrospective cohort study (Ding et al. 2018a). In the three of the experimental studies, semen ejaculates were placed a few centimeters away from a laptop, which was actively connected to Wi-Fi (Oni et al. 2011; Avendano et al. 2012; Kamali et al. 2017; Ding et al. 2018b) while one study used a Wi-Fi modem (Kamali et al. 2017). The closest distance was 3 to 5 cm while 60 cm was the farthest distance. The length of exposure ranged from 45 minutes to 4 hours. Two studies have clearly stated the characteristic of the samples subjected to the exposure. They consisted of normozoospermia, teratozoospermia and low semen volume samples (Avendano et al. 2012; Ding et al. 2018b). Meanwhile, three studies were distinctly characterized chronic diseases, presence of infection and azoospermia as the exclusion criteria for the semen samples and were excluded from the study (Kamali et al. 2017; Ding et al. 2018a, b). One study, however, failed to state the inclusion and exclusion criteria of the semen samples (Oni et al. 2011). Similar to the animal studies, all the SAR value reported in human studies conform to the recommended limits set by the US FCC and WHO.
In these human studies, sperm motility was significantly affected by the exposure (Oni et al. 2011). Increase in DNA fragmentation of the sperm was also observed (Avendano et al. 2012; Ding et al. 2018a, b). On the other hand, changes in sperm count and sperm viability were inconsistent between studies. Only one study reported a lack of change in sperm morphology after the RF-EMR exposure (Oni et al. 2011). In addition, two studies demonstrated increased ROS level and nucleic acid damage marker and decreased antioxidant enzyme in the semen, indicating that oxidative stress might increase with the RF-EMR exposure (Ding et al. 2018a, b). The data for the human studies is depicted in Table 3.

The effect of 2.45 GHz Wi-Fi RF-EMR on male rat reproductive system.
8-OHdG, 8-hydroxy-2′-deoxyguanosine; ALH, amplitude of lateral head displacement; BCF, beat cross frequency; CAT, catalase; Cu-Zn-SOD, copper-zinc-superoxide dismutase; CGRP, calcitonin gene-related peptide; CRP, C-reactive protein; DAP, distance of average path; DCL, curvilinear distance; DSL, distance straight line; GPx, glutathione peroxidase; GSH, glutathione; GSH-Px, phospholipid hydroperoxide glutathione peroxidase; IL, interleukin; LIN, linearity; MDA, malondialdehyde; Mn-SOD, manganase-superoxide dismutase; MOT, motility; PGE2, prostaglandin E2; PRO, progressive; ROS, reactive oxygen species; SOD, superoxide dismutase; STR, straightness; TAS, total antioxidant status; TOS, total oxidant status; VAP, average path velocity; VCL, curvilinear velocity; VEGF, vascular endothelial growth factor; VSL, straight line velocity; XO, xanthine oxidase.

The effect of 2.45 GHz Wi-Fi RF-EMR on male mice reproductive system.
3β HSD, 3β-hydroxysteroid dehydrogenase; CAT, catalase; Cu-Zn-SOD, copper-zinc-superoxide dismutase; GPx, glutathione peroxidase; MDA, malondialdehyde; Mn-SOD, manganase-superoxide dismutase; ROS, reactive oxygen species; SOD, superoxide dismutase.
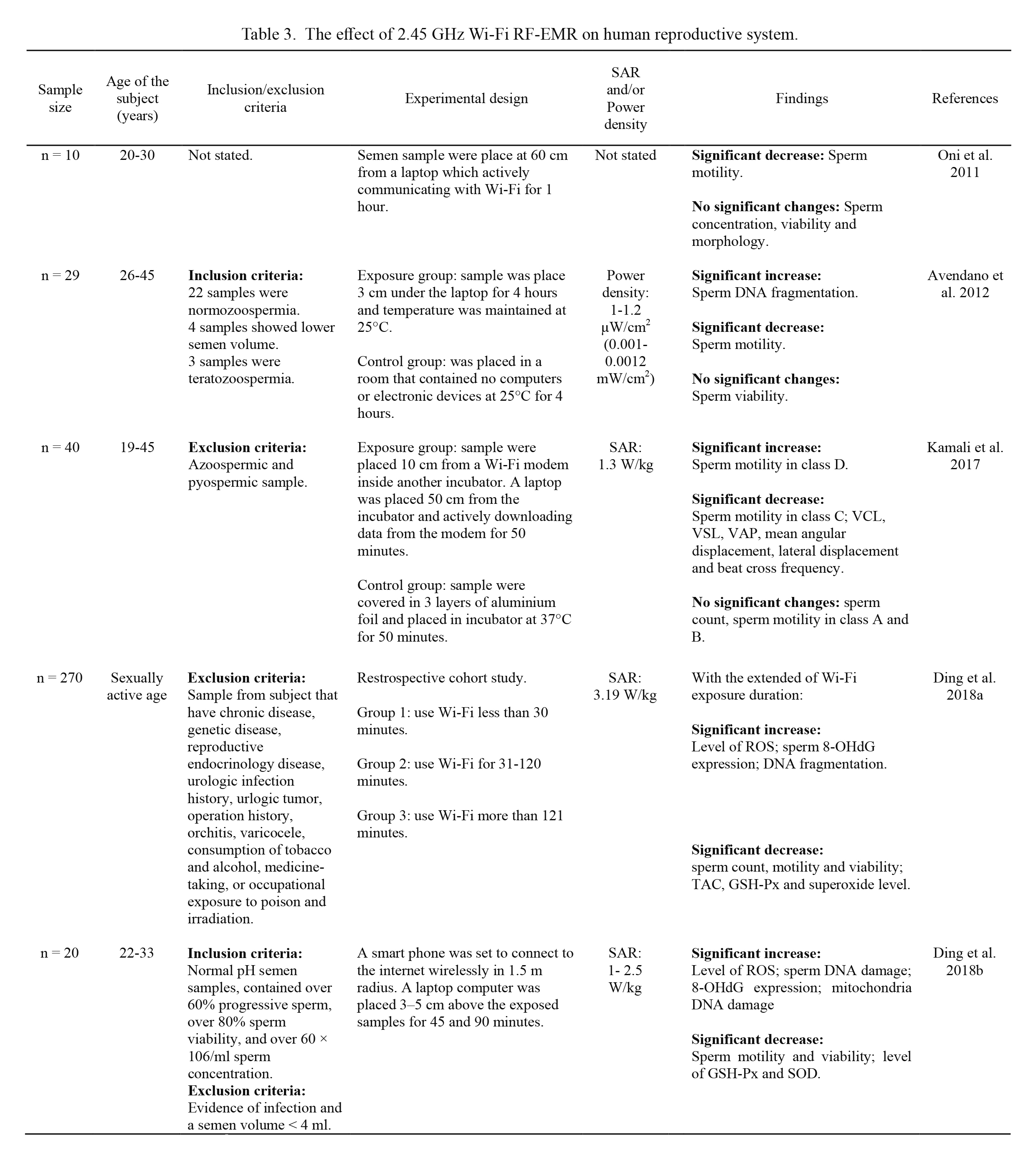
The effect of 2.45 GHz Wi-Fi RF-EMR on human reproductive system.
8-OHdG, 8-hydroxy-2′-deoxyguanosine; GSH-Px, phospholipid hydroperoxide glutathione peroxidase; ROS, reactive oxygen species; SOD, superoxide dismutase; TAC, total antioxidant capacity; VAP, average path velocity; VCL, curvilinear velocity; VSL, straight line velocity.
To date, Wi-Fi has become an essential component in the internet of things. While consumers are aware that Wi-Fi transmitters emit RF-EMR, controversy regarding the possible detrimental health effect of RF-EMR emitted from Wi-Fi transmitters endures. The findings of the RF-EMR exposure emitted by the Wi-Fi transmitter on the male reproductive health based on the reviewed studies are elaborate as below:
Effect of the exposure on male reproductive organ and sperm parametersThe exposure to 2.45 GHz RF-EMR radiation emitted from Wi-Fi transmitter caused a marked reduction in the weight of epididymis and seminal vesicle without affecting the weight of the testes in rats. Interestingly, the weight of cauda epididymis is positively related to sperm count (Mao et al. 2018), sperm maturation and reservoir (Sullivan and Mieusset 2016). Therefore, a decreased epididymal weight would reflect a reduction of sperm count. This assumption is further confirmed by the finding of reduced sperm count in in vivo studies (Kesari and Behari 2010; Shahin et al. 2014; Mahmoudi et al. 2015; Shokri et al. 2015; Saygin et al. 2016).
While most studies reported a decrease in sperm count, Delavarifar et al. (2018) reported a marginally significant increase in sperm count in control group compared to sham group. The oligospermic rat which received exposure at 150 cm from the RF-EMR generator showed an increase in sperm count as well though it was not statistically significant. This is an interesting finding requires further study. Based on findings by Delavarifar et al. (2018), there are two important research details that require attention; 1) Power density: the power density applied in the study is the lowest compared to other studies in this review. However, power density provides insufficient information on the biological aftermath compared to SAR (Lai 2005). SAR applied by Delavarifar et al. (2018) was not the lowest. Shahin et al. (2014) and Dasdag et al. (2015) had applied lower SAR at 0.00488 W/kg and 0.018 W/kg respectively and both demonstrated negative association of RF-EMR emitted from 2.45 GHz Wi-Fi transmitters on male reproduction (Shahin et al. 2014; Dasdag et al. 2015). 2) Duration of exposure: Delavarifar et al. (2018) had exposed the animals to RF-EMR for a duration of 2 h/day for four consecutive days while Shahin et al. (2014) and Dasdag et al. (2015) had longer exposure, i.e. for 24 h/day for 12 months and 2 h/day for 30 days respectively. Despite the differences in SAR, the cumulative exposure in the study of Delavarifar et al. (2018) could still be lower than the other studies due to the shorter exposure duration.
The evaluation of sperm counts in in vitro study using human ejaculated semen may not be an appropriate measure of reproductive health as the ejaculated sperm count could no longer be altered. Under normal physiology, sperm count is dependent on the spermatogenesis which takes place in the testes. The retrospective cohort study may reflect the effect of the RF-EMR exposure better because it involves a direct association of the Wi-Fi usage on the testes, in which spermatogenesis occurs (Ding et al. 2018a). In experimental studies involving manipulation of the ejaculated semen, however, sperm motility and sperm DNA were the most sensitive parameters apart from sperm count. This is parallel with findings found in the animal study. Other sperm parameters which are sperm morphology and viability were found to be inconsistent between studies, both in vivo and in vitro.
The effect of the exposure on the testes microenvironmentThe negative effect of RF-EMR exposure emitted by Wi-Fi transmitter on the sperm parameters is a reflection of impaired spermatogenesis which in turn, is a result of negative histomorphometry changes and inflammation of the testes and apoptosis of testicular cells.
Histopathological evaluation on the testes had demonstrated various degenerative features, including irregular shape and a decrease in diameter of seminiferous tubule, thinning of tunica albuginea layer with dilated and congested blood vessel both in tunica albuginea and in the interstitial space. Ample spaces between the Sertoli cells and spermatogonia and the detachment of spermatogonia from the tunica propria had creates peripheral spaces. These peripheral spaces caused disconnection of Sertoli and spermatogonia interaction. Subsequently, this will cause a decrease in spermatogonia proliferation, leading to spermatid density depletion in the seminiferous tubule and therefore, reduced sperm count (Saygin et al. 2016).
Most of the studies reviewed also demonstrated that Leydig cells were affected as evidenced by a reduced number of cells (Saygin et al. 2011) and abnormal irregular appearance (Shahin et al. 2014; Simaiova et al. 2018). However, Almasiova et al. (2018) reported contradicting result in which the Leydig cells remained intact. Yet, all of the studies demonstrated a decrease in testosterone level regardless of Leydig cell number (Kumar et al. 2011; Shahin et al. 2014; Saygin et al. 2016; Jonwal et al. 2018). Since testosterone is a very important hormone for spermatogenesis (Ramaswamy and Weinbauer 2014) as well as for the maintenance of structural and physiological function of seminiferous tubules (Walker 2010), decreased levels of this hormone may further exaggerate spermatogenesis impairment following the exposure. Furthermore it was also noted that, 3β-hydroxysteroid dehydrogenase (3β-HSD) activity was also decreased (Shahin et al. 2014). As this steroidogenic enzyme is responsible to activate steroid hormones including testosterone (McVey and Cooke 2003), the depletion of 3β-HSD activity may further amplify the decrease in testosterone level.
Inflammation may also significantly impact the microenvironment of the testes. It is evident that prostaglandin E2 (PGE2) and calcitonin gene-related peptide (CGRP) activities are responsible for testicular inflammation following RF-EMR exposure (Saygin et al. 2016). However, inflammation marked by interleukin 6 (IL-6), IL-10 and IL-32 levels showed no significant changes in the testicular tissue (Bilgici et al. 2018). Despite this, the presence of testicular apoptotic cells and the expression of caspase-3, caspase-8 and Bax-gene highlighted the possible involvement of low-grade inflammation (Kumar et al. 2011; Saygin et al. 2011; Shokri et al. 2015; Simaiova et al. 2018).
Pathophysiological mechanism associated with RF-EMR exposureInitial assumption of RF-EMR pathological pathway is that non-ionizing radiation emitted from the Wi-Fi transmitter would only cause damage through thermal effects (Almasiova et al. 2018). However, based on the findings of this review, it is evident that the non-thermal effect also plays a vital role in creating damage to the male reproductive organs. The increase in lipid peroxidation (Ozorak et al. 2013; Oksay et al. 2014; Shahin et al. 2014) and 8-hydroxy-2′-deoxyguanosine (8-OHdG) activity, a marker of nucleic acid damage, in the testes (Atasoy et al. 2013) and sperm (Ding et al. 2018a, b) hinted the involvement of the non-thermal effect. In addition, oxidative and nitrosative stress, as well as total oxidant status (Wiesner et al. 2008), were reported to show an increment following exposure (Shahin et al. 2014; Saygin et al. 2016). This result is congruent with a decrease in enzymatic antioxidant (SOD, CAT, XO, GPx, GPH, GPH-Px) and non-enzymatic anti-oxidant (vitamin A and E) (Kesari and Behari 2010; Atasoy et al. 2013; Oksay et al. 2014; Shahin et al. 2014; Saygin et al. 2016; Jonwal et al. 2018) as well as increase in SOD positive cells and immunoreactivity of i-NOS in spermatogonia and Leydig cells (Shahin et al. 2014; Almasiova et al. 2018; Simaiova et al. 2018). Human studies also showed similar findings (Ding et al. 2018a, b). Therefore, oxidative stress in male reproductive organs may be elevated following the exposure to RF-EMR emitted from Wi-Fi transmitters (Fig. 2).

Mechanisms of RF-EMR exposure emitted from 2.45 GHz Wi-Fi transmitter action on the testes.
3β HSD, 3β-hydroxysteroid dehydrogenase; 8-OHdG, 8-hydroxy-2′-deoxyguanosine; CAT, catalase; CGRP, calcitonin gene-related peptide; GPx, glutathione peroxidase; GSH, glutathione; GSH-Px, phospholipid hydroperoxide glutathione peroxidase; MDA, malondialdehyde; PGE2, prostaglandin E2; ROS, reactive oxygen species; SOD, superoxide dismutase; TAS, total antioxidant status; TOS, total oxidant status; XO, xanthine oxidase.
The experimental settings evaluated the effect of the 2.45 GHz Wi-Fi transmitters on the male reproductive system could affect the result of the studies. These settings include the type of antenna, the distance between the source of radiation and the animals/samples, the exposure duration (short and long-term exposure) and the age of the animals/subjects. Imitation of real human exposure remains challenging. For instance, distance from the Wi-Fi transmitter and the duration of exposure might vary throughout the day as the users were performing their daily activities. On the other hand, binge Wi-Fi users may spend most of the time close to the transmitters but received inconsistent intensity which could be interfered by multiple signals from the surrounding. The actual human exposure occurs in repetitive pattern and in a long-term duration (Lai 2005). Even though there is a putative negative association between Wi-Fi and health, the evolvement of the technology will continue. With the knowledge that oxidative stress plays an important role in mediating the effects of RF-EMR exposure on the male reproductive system, it is recommended to maintain the antioxidant status quo for fertility perseverance in men.
Direction of future researchThe Wi-Fi technology is evolving at a fast pace. Thus, it is important for the researchers to validate its health effects in time. Although 2.45 GHz Wi-Fi frequency is prevalent currently, the market has introduced a double frequency Wi-Fi which emits 2.45 GHz and 5 GHz radiation simultaneously. Alternative to Wi-Fi, Light Fidelity (Li-Fi) (Saini 2012) which claimed to be ‘greener’ as it uses common LED light bulbs (Lumoindong et al. 2018) yet provides 100 times faster speed than current Wi-Fi (up to 224 Gb/s) (Chakraborty et al. 2017) has been proposed. Health safety of these newer technologies should be determined to avoid jeopardizing user’s health.
We acknowledge the financial support from National University of Malaysia (UKM) Geran Galakan Penyelidikan (GGP-2017-001).
The authors declare no conflict of interest.