2019 年 249 巻 3 号 p. 147-154
2019 年 249 巻 3 号 p. 147-154
Osteoporosis is characterized by bone loss and skeletal fragility and is likely to occur in postmenopausal women. Distal radius fracture is a type of fragility fractures associated with osteoporosis. Bone mineral density (BMD) refers to the amount of mineral in bone tissue and is an indicator of osteoporosis. This study aimed to investigate the relationship between the severity of distal radius comminution and the BMD of the healthy contralateral forearm and femur in postmenopausal women. Of 165 women who sustained low-energy trauma from falls on flat ground, forearm and femoral neck BMDs were measured in 155 and 163 participants, respectively. Evaluation of distal radius comminution was performed by computed tomography, and the severity is classified based on the degree of articular surface comminution and on the presence of metaphyseal comminution. We thus evaluated 165 cases of articular surface comminution (extra-articular, 43 cases; intra-articular simple, 91 cases; and intra-articular multifragment, 31 cases) and metaphysis comminution (metaphyseal simple, 58 cases; metaphyseal monocortical comminution on either the palmar or dorsal side, 82 cases; and metaphyseal bicortical comminution on the palmar and dorsal sides, 25 cases). There was no significant association between intra-articular comminution and BMD of the forearm and femur. By contrast, the participants with metaphyseal bicortical comminution showed lower BMD of the forearm and femur compared with other types of metaphysis comminution (p < 0.05). In conclusion, postmenopausal women who developed bicortical comminuted fractures of the distal radius tend to have lower femoral BMD, which may predispose them to future hip fractures.
Osteoporosis is a skeletal disorder characterized by compromised bone strength that predisposes patients to an increased risk of fractures (Kanis 1984). Postmenopausal osteoporosis leads to an increased risk of fragility fractures, such as femoral neck fractures, humeral neck fractures, vertebral fractures, and distal radius fractures. A distal radius fracture is a classic fragility fracture that is typically caused by a fall onto an outstretched hand, and often occurs as an early fracture in osteoporosis (Mallmin and Ljunghall 1994; Sontag and Krege 2010). Bone mineral density (BMD) refers to the amount of mineral contained in bone tissue and is measured by dual-energy x-ray absorptiometry. It is indicative of the severity of osteoporosis; indeed, osteoporosis with low BMD is a risk factor for distal radius fractures (Hegeman et al. 2004; Itoh et al. 2004; Hung et al. 2005; Bahari et al. 2007; Harness et al. 2012; Xu et al. 2017). Distal radius fractures accompanying osteoporosis may precede future secondary fractures, such as femoral and vertebral fractures (Cuddihy et al. 1999; Bozkurt et al. 2018). Thus, the prevention and treatment of osteoporosis are important for the prevention of fractures. However, if a distal radius fracture occurs in a patient with low BMD, this may result in even more severe fragility fractures (Lill et al. 2003; Sakai et al. 2008; Clayton et al. 2009). According to the AO Foundation and Orthopedic Trauma Association (AO/OTA) (Müller et al. 1990), severity is classified based on the degree of articular surface comminution and the presence or absence of metaphyseal comminution. To date, no reports have investigated the relationship between articular surface and metaphysis comminution in the distal radius and BMD of the forearm and femur in postmenopausal women. Therefore, we investigated whether there was a correlation between BMD and the degree of articular surface and metaphyseal comminution. In addition, BMD was also measured in the contralateral healthy forearm and right femoral neck. We hypothesized that, both on the articular surfaces and in the metaphysis, BMD would be significantly lower in cases of severe comminution. If our hypothesis was proven to be true, high BMD would not only prevent bone fractures but would also reduce the severity of distal radius fractures. Furthermore, this would suggest that, in patients with lower femoral neck BMD, the prevention of secondary femoral fractures is more important in cases of severe comminution (compared to cases with no comminution).
The study protocol was approved by Ethical committee of Seirei Hamamatsu General Hospital (approval number: 2071). The methods were carried out in accordance with the relevant guidelines and regulations, and informed consent was obtained from all participants.
Of the distal radius fracture patients that visited our hospital from 2011 to 2017, we targeted postmenopausal women older than 50 years. We recruited patients who had sustained low-energy trauma from falls on flat ground and excluded those with high-energy trauma from falls and traffic accidents. Evaluation of comminution was performed by computed tomography at the time of injury, and articular surface comminution and metaphysis comminution were evaluated separately. First, to investigate whether articular surface comminution is related to the BMDs of forearm and femur, we classified all subjects into the following three groups; 1) the extra-articular fracture (Ea) group; 2) the articular simple (As) group, who had intra-articular simple fractures with only a single fracture line; and 3) the articular multifragmentary (Am) group, who had intra-articular comminution fractures with multiple fracture lines (Fig. 1). Second. to investigate the relationship of metaphyseal comminution with the BMDs of forearm and femur, we performed another classification of all subjects into three groups; 1) the metaphyseal simple (Ms) group, who had no comminution; 2) the metaphyseal monocortical comminution (Mm) group, who had comminution on either the palmar or dorsal side; and 3) the metaphyseal bicortical comminution (Mb) group, who had comminution on both the palmar and dorsal sides (Fig. 2).
BMD of the distal third of the contralateral healthy forearm and the right femoral neck was measured using dual-energy x-ray absorptiometry (Hologic Discovery; Marlborough, MA, USA). In total, 165 cases were investigated. The patients’ mean age was 69.8 ± 0.73 years (range, 50-89 years), mean height was 153.7 ± 0.48 cm (range, 137-170 cm), mean weight was 52.0 ± 0.82 kg (range, 31-75 kg), and mean body mass index (BMI) was 22.0 ± 0.31 kg/m2 (range, 14.0-37.5 kg/m2). Three patients had rheumatoid arthritis and 16 had diabetes mellitus; no patients had renal failure. Three patients had a history of vertebral fractures, and one patient had a history of proximal femoral fracture; no patients had history of humeral neck fractures. Patients received the following medical therapies for osteoporosis: bisphosphonate (n = 5), vitamin D (n = 6), calcium (n = 2), and vitamin K and calcitonin (n = 1). In the classification of articular surface comminution, there were 43 cases in the Ea group, 91 cases in the As group, and 31 cases in the Am group. In the classification of metaphyseal comminution, there were 58 cases in the Ms group, 82 cases in the Mm group, and 25 cases in the Mb group. Due to patient disagreement, 10 of the 165 patients underwent femoral BMD measurements only and three underwent forearm BMD measurements only. Therefore, we examined 155 cases of forearm BMD and 162 cases of femoral BMD (Fig. 3). Among the 155 cases with forearm BMD measurements, the patients’ mean age was 69.7 ± 0.75 years (range, 50-89 years); mean height was 153.9 ± 0.49 cm (range, 137-170 cm); mean weight was 51.7 ± 0.82 kg (range, 31-106 kg); and mean BMI was 21.8 ± 0.30 kg/m2 (range 14.0-37.1 kg/m2). Among the 162 cases with femoral BMD measurements, the patients’ mean age was 69.8 ± 0.74 years (range, 50-89 years); mean height was 153.6 ± 0.48 cm (range, 137-170 cm); mean weight was 52.0 ± 0.83 kg (range 31-106 kg); and mean BMI was 22.0 ± 0.32 (range, 14.0-37.5) (Table 1). In these groups, we analyzed whether fracture type was associated with BMD in the forearm or femoral neck. We then investigated, in all 165 cases, the relationship between BMI and intra-articular and metaphyseal comminution. We also investigated the correlation between forearm and femoral BMD in the 152 patients with both forearm and femoral BMD measurements.
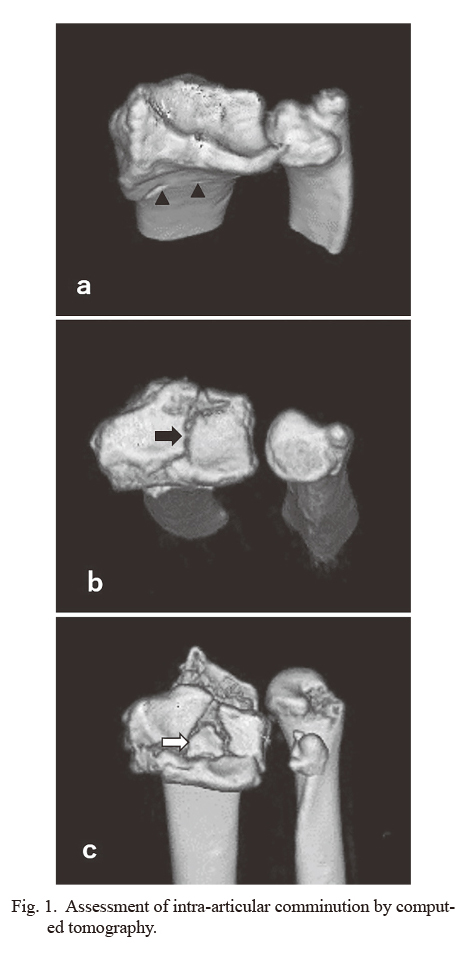
Assessment of intra-articular comminution by computed tomography.
(a) Extra-articular (Ea), (b) articular simple (As), and (c) articular multifragmentary (Am) groups. The black arrowheads indicate the extra-articular fracture line. The black arrow indicates the intra-articular single fracture line. The white arrow indicates the intra-articular third fragment.

Assessment of metaphyseal comminution by computed tomography.
(a) Metaphyseal simple (Ms), (b) metaphyseal monocortical comminution (Mm), and (c) metaphyseal bicortical comminution (Mb) groups. Right image is volar aspect and left image is dorsal aspect in each panel. The black arrows indicate the metaphyseal simple fracture line. The white arrows indicate metaphyseal comminuted fragments.
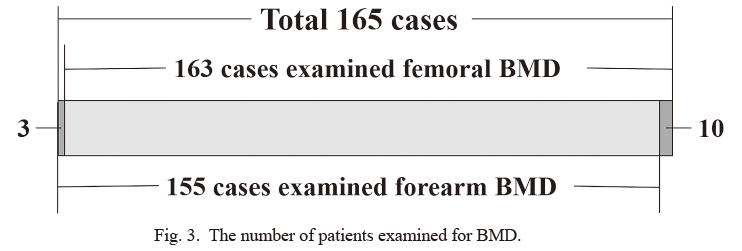
The number of patients examined for BMD.
Ten patients received femoral BMD measurements only, and three patients received forearm BMD measurements only.

Age, height, weight, and BMI of the target cases.
BMI, body mass index; BMD, bone mineral density.
Results are expressed as mean ± standard deviation. Differences in average BMD between the groups were tested using the Tukey-Kramer method, and p < 0.05 was considered significantly different. The correlation coefficient between forearm and femoral BMD was calculated using Pearson correlations. The software used for statistical analysis was SPSS version 24 (IBM Corp., Armonk, NY, USA).
Among the articular comminution groups, there were 41 cases in the Ea group, 84 cases in the As group, and 30 cases in the Am group. Mean forearm BMD was 0.401 ± 0.011 (range, 0.240-0.605), 0.431 ± 0.008 (range, 0.279-0.605), and 0.405 ± 0.012 (range, 0.263-0.512) g/cm2 in the Ea, As, and Am groups, respectively. No significant differences were observed between the groups (Ea-As, p = 0.078; As-Am, p = 0.194; Ea-Am, p = 0.980). Among the metaphyseal comminution groups, there were 55 cases in the Ms group, 78 cases in the Mm group, and 22 cases in the Mb group. Mean forearm BMD was 0.435 ± 0.011 (range, 0.254-0.605), 0.419 ± 0.008 (range, 0.240-0.594), and 0.375 ± 0.012 (range, 0.263-0.462) g/cm2 in the Ms, Mm, and Mb groups, respectively. The Mb group showed significantly lower values compared with the other groups, but no significant difference was observed between the Ms and Mm groups (Ms-Mm, p = 0.404; Mm-Mb, p = 0.033; Ms-Mb, p = 0.003) (Table 2, Fig. 4).
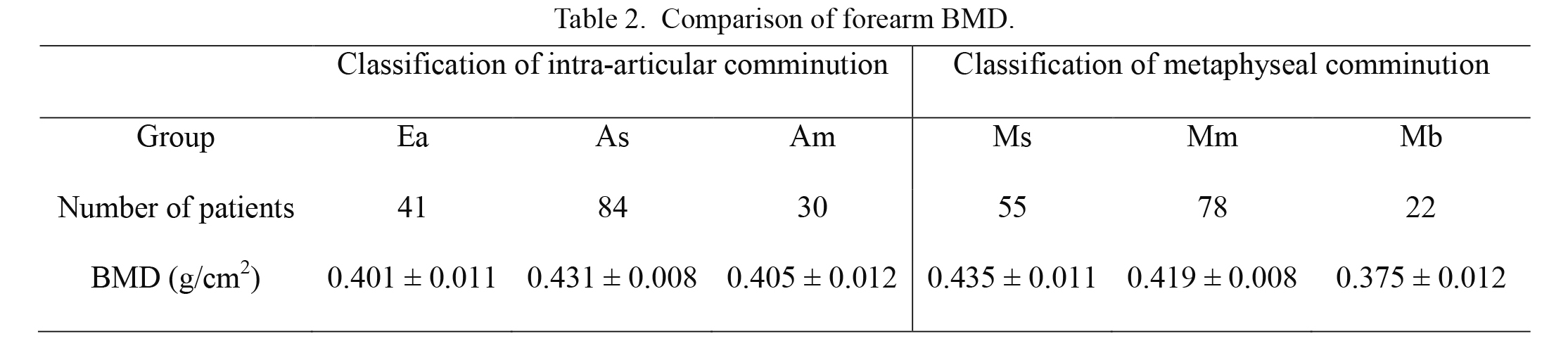
Comparison of forearm BMD.
Am, articular multifragmentary; As, articular simple; BMD, bone mineral density; Ea, extra-articular; Mb, metaphyseal bicortical comminution; Mm, metaphyseal monocortical comminution; Ms, metaphyseal simple.

Correlation of forearm BMD with distal radial comminution.
Forearm BMD and articular comminution. (b) Forearm BMD and metaphyseal comminution.
*Significant difference (p < 0.05).
**Significant difference (p < 0.01).
Among the articular comminution groups, there were 42 cases in the Ea group, 89 cases in the As group, and 31 cases in the Am group. Mean femoral neck BMD was 0.530 ± 0.019 (range, 0.276-0.959), 0.562 ± 0.010 (range, 0.272-0.885), and 0.553 ± 0.020 (0.358-0.766) g/cm2 in the Ea, As, and Am groups, respectively. No significant differences were observed between the groups (Ea-As, p = 0.244; As-Am, p = 0.915; Ea-Am, p = 0.629). Among the metaphyseal comminution groups, there were 56 cases in the Ms group, 81 cases in the Mm group, and 25 cases in the Mb group. Mean femoral neck BMD was 0.573 ± 0.016 (range, 0.276-0.959), 0.554 ± 0.010 (range, 0.358-0.766), and 0.497 ± 0.019 (range, 0.272-0.671) g/cm2 in the Ms, Mm, and Mb groups, respectively. The Mb group showed significantly lower values than the other groups, but no significant difference was observed between the Ms and Mm groups (Ms-Mm, p = 0.537; Mm-Mb, p = 0.039; Ms-Mb, p = 0.006) (Table 3, Fig. 5).

Comparison of femoral neck BMD.
Am, articular multifragmentary; As, articular simple; BMD, bone mineral density; Ea, extra-articular; Mb, metaphyseal bicortical comminution; Mm, metaphyseal monocortical comminution; Ms, metaphyseal simple.
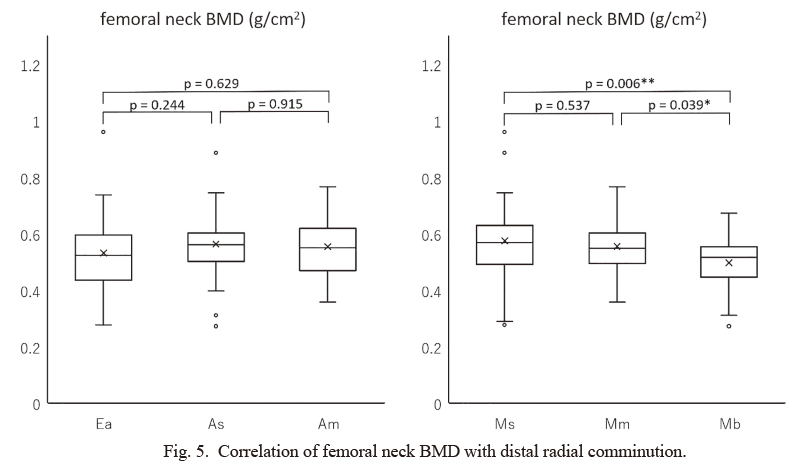
Correlation of femoral neck BMD with distal radial comminution.
(a) Femoral neck BMD and articular comminution. (b) Femoral neck BMD and metaphyseal comminution.
*Significant difference (p < 0.05).
**Significant difference (p < 0.01).
Among the classification of intra-articular comminution, there were 43 cases in the Ea group, 91 cases in the As group, and 31 cases in the Am group. Mean BMI was 22.0 ± 0.64 (14.0-35.1), 21.8 ± 0.42 (14.7-37.5), and 22.3 ± 0.68 (15.2-31.2) kg/m2 in the Ea, As, and Am groups, respectively. No significant differences were detected between the three groups (Ea-As, p = 0.968; As-Am, p = 0.824; Ea-Am, p = 0.940). Among the classification of metaphyseal comminution, there were 58 cases in the Ms group, 82 cases in the Mm group, and 25 cases in the Mb group. Mean BMI was 22.1 ± 0.59 (16.9-37.5), 21.8 ± 0.41 (14.0-32.0), and 22.0 ± 0.80 (14.7-29.3) kg/m2 in the Ms, Mm, and Mb groups, respectively, and no significant differences between the groups were observed (Ms-Mm, p = 0.892; Mm-Mb, p = 0.990; Ms-Mb, p = 0.979) (Table 4).
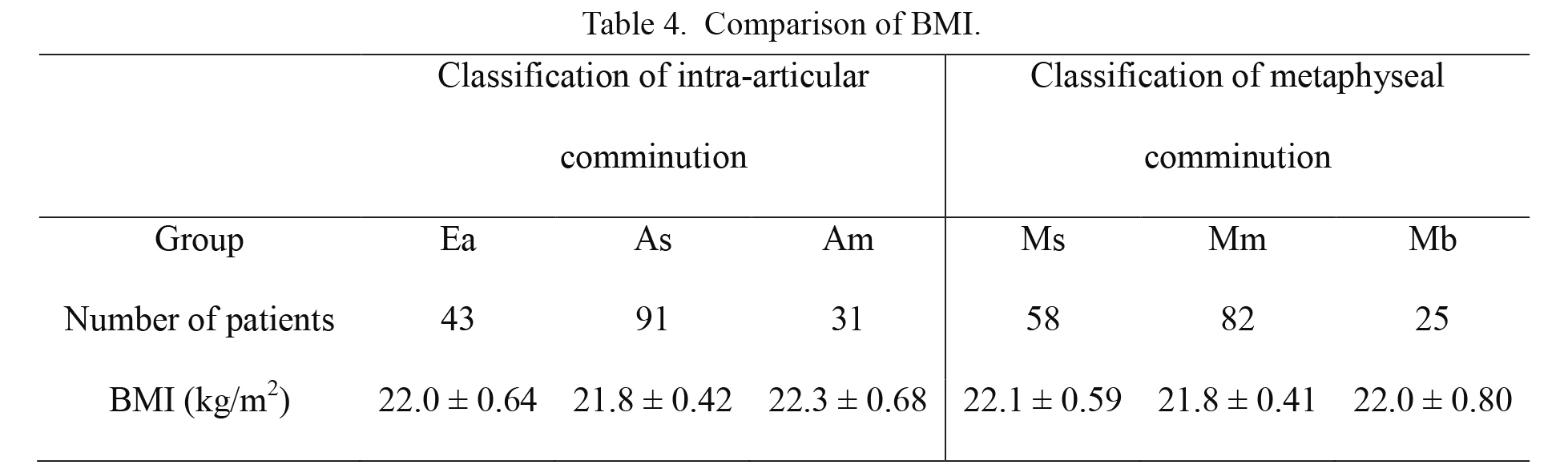
Comparison of BMI.
Am, articular multifragmentary; As, articular simple; BMI, body mass index; Ea, extra-articular; Mb, metaphyseal bicortical comminution; Mm, metaphyseal monocortical comminution; Ms, metaphyseal simple.
In the 152 cases with both forearm and femoral neck BMD measurements, the BMD of the forearm and the femoral neck showed a significant positive correlation (r = 0.666) (Fig. 6).
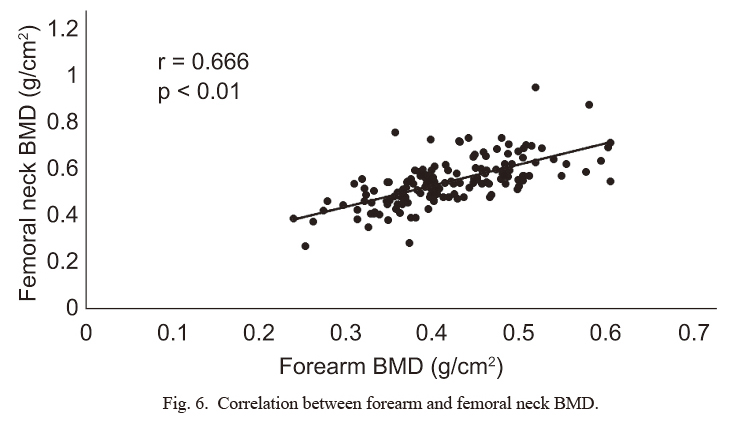
Correlation between forearm and femoral neck BMD.
One hundred fifty-two cases with both forearm and femoral neck BMD measurements.
In the current study, there was no association between articular surface comminution and BMD of the forearm and femoral neck. We also found that in the metaphysis, forearm and femoral neck BMD were significantly lower in cases with bicortical comminution. We did not find any association between intra-articular comminution and BMI, or between metaphyseal comminution and BMI. We also found a strong correlation between forearm and femoral neck BMD.
Previous reports have described the relationship between the severity of distal radius fractures and BMD. However, no reports have investigated the relationship between metaphyseal comminution of the distal radius and BMD of the forearm and proximal femur. Sakai et al. (2008) reported that the degree of deformity of the distal radius fracture, palmar tilt, radial inclination, and ulnar variance were related to lumbar spine BMD. In a cadaver study, Lill et al. (2003) reported a correlation between AO classification, Cooney classification (Cooney 1993), and forearm BMD. Clayton et al. (2009) reported that hip joint BMD correlates with early instability of a distal radius fracture, carpal malalignment, and the occurrence of nonunion. While these reports described the relationship between distal radius fractures and BMD of the hip or spine, they did not discuss metaphyseal comminution of the distal radius. In the present study, we did not find any association between articular surface comminution and BMD. However, we found that in the metaphysis, BMD was significantly lower in cases of comminution on both the palmar and dorsal sides of the hand. As there is a high degree of metaphyseal comminution in cases with low BMD, it is conceivable that the visible displacement on plain X-rays is also increased. Furthermore, since, it is thought that deformity likely occurs after reduction, it can be concluded that these findings are consistent with those of previous studies (Sakai et al. 2008; Clayton et al. 2009; Lill et al. 2003).
The results of the present study did not confirm the influence of BMI on fracture comminution. Greater body weight tends to increase the severity of comminution due to the stronger forces applied to the bones. One report indicated that BMI affects the severity of distal radius fractures (Xu et al. 2017), but another study reported that there was no correlation between fracture type according to AO classifications and BMI (Acosta-Olivo et al. 2017).
In fragility fractures (such as femoral neck, vertebral, humeral neck, and distal radius fractures), distal radius fractures tend to occur as the initial fracture (Sontag and Krege 2010). Although the incidence of femoral neck and vertebral fractures increases rapidly with age, the incidence of distal radius fractures increases more gradually with age. Concerning the osteoporotic fractures, Sakuma et al. (2008, 2014) reported that the incidence of age-related distal radius fractures is different from the incidence of other osteoporotic fractures. In cases of distal radius fractures, the patient should be examined for osteoporosis and the risk of secondary fractures should be taken into consideration. Treatment for osteoporosis should be given once a diagnosis is confirmed. Based on the results of the present study, it is highly likely that in cases of metaphyseal comminution on both the palmar and dorsal sides, the femoral neck also has lower BMD. Webber et al. (2015) examined the association between the thickness of the cortical bone distal to the radius and femoral BMD. The authors found that the thinner the cortex, the lower the femoral BMD. Furthermore, Shin et al. (2016) reported that hip joint BMD influenced the risk of distal radius fracture. The results of the present study confirmed a strong correlation between forearm and femoral neck BMD. Iba et al. (2018) reported that in patients with femoral neck and distal radius fractures, orthopedic surgeons did not properly intervene and treat the patients’ osteoporosis after the fracture. Bougioukli et al. (2019) also described inappropriate treatment of osteoporosis after fragility fractures. Distal radius fractures provide an important opportunity during which to identify osteoporosis, which should not be missed. Cuddihy et al. (1999) reported that forearm fractures are predictive of osteoporotic fractures, and Bozkurt et al. (2018) stated that vertebral and distal radius fractures are precursors to femoral neck fractures. A diagnosis of osteoporosis following a distal radius fracture is also essential towards preventing femoral neck fractures, which can occur as a secondary fracture.
Johnell et al. (2005) reported that femoral neck BMD is a strong predictor of hip fractures, and in the present study, we showed that patients with distal radius fractures with metaphyseal bicortical comminution had low femoral neck BMD. Thus, such patients may be more likely to suffer from secondary hip fractures. Orthopedic surgeons should treat these patients as osteoporotic to prevent potential future hip fractures.
A limitation of this study is the small number of cases; hence, it will be necessary to increase the sample size in further investigations. Additionally, we should have measured grip strength of the contralateral healthy hand in all cases, as it may have affected the BMD of the forearm and femur. Moreover, healthy controls were not investigated, and it was not possible to confirm the presence or absence of an actual secondary fracture following distal radius fractures. Future studies should conduct long-term follow ups to assess the occurrence of secondary fractures in patients with distal radius fractures.
We would like to thank all the doctors and staff who contributed to this study. We especially express our gratitude to Drs. A. Suzuki, M. Mukoda, and J. Tsuchiya for their help with data collection.
All authors contributed greatly to design of study, collection and/or interpretation of data, drafting and/or critical revision of the manuscript. T.K., N.E., and N.K. designed the study. T.K. collected data and wrote the first draft of the manuscript. N.E., and N.K. contributed to data collection and interpretation. T.K., N.E., and N.K. critically revised the manuscript.
The authors declare no conflict of interest.