2019 年 249 巻 3 号 p. 155-161
2019 年 249 巻 3 号 p. 155-161
Patent ductus arteriosus (PDA) is a common problem among preterm infants. The standard of care for PDA has been to attempt to close the PDA by pharmacological treatment or surgical ligation. Recently, conservative approach for PDA (i.e., infants receive no treatment for PDA unless it is necessary for rescue) is gaining interest. However, when PDA is persisted under the conservative approach, there is a concern about the neurodevelopmental problems caused by decreased cerebral oxygenation. Our objective was to examine the risk of neurodevelopmental impairment in preterm infants, when PDA remained persistently open under conservative approach for PDA. We retrospectively analyzed data from the medical charts in 72 included infants (gestational age < 29 weeks, birth weight < 1,250 g). Under our conservative approach for PDA, we divided infants by their ductal patency: a closed ductus group (ductus closure within 14 days after birth, n = 52) and a persistent patent ductus arteriosus group (ductus closure after 14 days, n = 20). We compared the clinical parameters and neurodevelopmental outcomes assessed with the Kaufman Assessment Battery for Children (K-ABC) at 5 years of corrected age in two groups. Among the children who completed the K-ABC test, there were no significant differences in neurodevelopmental scores between a closed ductus group (n = 44) and a persistent patent ductus arteriosus group (n = 17). A conservative approach for PDA, even in the case of prolonged PDA, does not increase the risk of neurodevelopmental impairment at 5 years of corrected age in preterm infants.
Patent ductus arteriosus (PDA) is a common problem in preterm infants. In infants exposed to hemodynamically significant PDA, the risks of pulmonary congestion, congestive heart failure, and reduced systemic blood flow are increased (Clyman 2006). Many studies have demonstrated that PDA is associated with significant morbidities, such as intraventricular hemorrhage, chronic lung disease, necrotizing enterocolitis, retinopathy of prematurity, and/or neurodevelopmental impairment (Evans and Kluckow 1996; Dollberg et al. 2005; Chorne et al. 2007; Noori et al. 2009).
Intravenous cyclooxygenase (COX) inhibitor is now widely used as a first-line therapy for hemodynamically significant PDA in very low birth weight (VLBW) infants. However, very premature babies frequently fail to achieve PDA closure by COX inhibitor administration (Koch et al. 2006). When the ductus arteriosus (DA) fails to close after COX inhibitor treatment, there is little information regarding whether neonatologists should use a repeated COX inhibitor administration, or surgical approach for DA closure and which of these may be advantageous (Bose and Laughon 2007). Surgical DA ligation is usually considered when medical treatment has failed or is contraindicated, but some studies have shown that surgical ligation may contribute to increased mortality and morbidity (Madan et al. 2009; Mirea et al. 2012; Bourgoin et al. 2016). Recently conservative approach for PDA has been gaining interest (Jhaveri et al. 2010; Wickremasinghe et al. 2012; Clyman et al. 2019). Conservative approach generally means infants does not receive any initial treatments to close PDA, pharmacologic agents are used only for rescue infants when PDA becomes hemodynamically significant, and do not undergo surgical ligation until systemic complications developed or COX inhibitor contraindicated (for example; inotrope-dependent hypotension, acute renal failure, feeding intolerance). However, other studies have suggested that persistent PDA compromises the perfusion and oxygenation of the preterm brain and negatively affects neurodevelopmental outcomes (Lemmers et al. 2008). Furthermore, there is a paucity of information on the long-term outcomes achieved in patients with persistent PDA. Although it had reported that cerebral oxygen saturation and extraction were not affected by hemodynamically significant PDA in preterm infants within 2 weeks after birth (van der Laan et al. 2016), we often experience PDA persistent more than 2 weeks. And the neurodevelopmental effect of longer persistent PDA is unknown. Our management for PDA has been relatively conservative approach, which avoid ligation as long as possible, while maintaining the blood flow of the brain using COX inhibitor when PDA becomes hemodynamically significant.
The purpose of this study was to examine the risk of neurodevelopmental impairment in preterm infants, when PDA remained persistently open under conservative approach for PDA.
This study was approved by the ethics committee of Japanese Red Cross Sendai Hospital (No 2018-148). The study involved all VLBW infants who were born before gestational age (GA) of 29 weeks with a birth weight of < 1,250 g and admitted to the neonatal intensive care unit (NICU) of the Japanese Red Cross Sendai Hospital from January 2010 to March 2013 (n = 99). All data were extracted retrospectively from medical records. The exclusion criteria were (1) death in the NICU, (2) chromosomal aberrations or multiple malformations, (3) lost to follow up. Fig. 1 depicts the study population.
The patients were divided into two groups: closed ductus and persistent patent ductus arteriosus. The closed ductus group comprised patients whose ductus closed either spontaneously or in response to indomethacin or surgical ligations within the 14 days after birth. The persistent patent ductus arteriosus group comprised patients whose ductus was open for more than 14 days after birth. The groups divided 14 days after birth based upon van der Laan’s study (2016) that reported that cerebral oxygen saturation was not affected by hemodynamically significant PDA in preterm infants within 2weeks after birth. At 5 years of corrected age, a neuropsychological assessment was performed by trained psychologists. In enrolled infants (n = 72): the closed ductus group (n = 52), the persistent patent ductus arteriosus group (n = 20), GA, birth weight, administration of antenatal steroid, sex, Apgar scores, the rates of singleton, small for gestational age (SGA), and the occurrence of respiratory distress syndrome (RDS), intraventricular hemorrhage, periventricular leukomalacia (PVL), necrotizing enterocolitis, retinopathy of prematurity with laser coagulation, chronic lung disease with home oxygen therapy, exposure to indomethacin, surgical ligation, neurodevelopmental impairment, duration of persistent PDA and neurodevelopmental assessment scores were compared between the two groups.
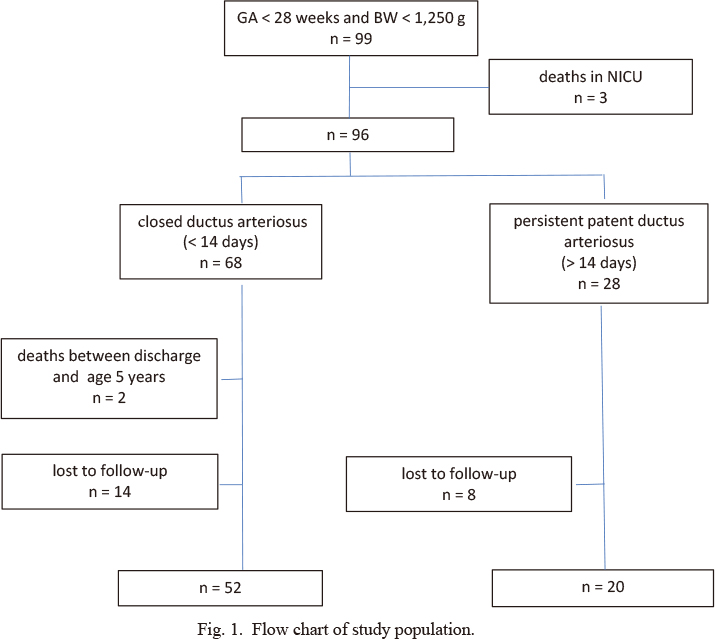
Flow chart of study population.
GA, gestational age; BW, birth weight.
Our management of PDA has historically been relatively conservative approach; that is, we control DA flow by indomethacin treatment in the presence of the DA shunt, and surgical ligation is avoided as long as possible. As protecting the brain is the important priority in the management of preterm infants, we use indomethacin when PDA becomes hemodynamically significant. No infants received prophylactic treatment with indomethacin. The conservative approach comprised fluid restriction, diuretics, or mechanical ventilation adjustment to manage the PDA shunt. DAs were ligated only when one or more of the following were observed: 1) persistent hypotension requiring inotropic support to maintain brain perfusion (the presence of interrupted diastolic flow in the anterior cerebral artery), 2) feeding intolerance, and 3) contraindication to indomethacin treatment. Treatment decisions for PDA are made by attending neonatologists.
The diagnosis of a hemodynamically significant PDA is based on clinical indices (continuous systolic heart murmur, tachycardia, widened pulse pressure) and confirmed by echocardiographic investigation (ductus diameter > 1.5 mm, left atrium-to-aortic root (LA/Ao) ratio > 1.5, left pulmonary artery end diastolic flow velocity > 0.2 m/second, and the presence of diastolic reversal of flow in the renal artery (El Hajjar et al. 2005)). An ultrasonographic device (Philips CX50) with a S12-4 probe is used for the blood flow diagnosis. When infants develop a hemodynamically significant PDA, they receive treatment with indomethacin. The initial dose of indomethacin is 0.1 mg/kg in infants treated within 48 hours of birth and 0.1-0.2 mg/kg in infants treated from 2 days after birth. In all cases, indomethacin was administered intravenously for 1-4 hour and maximum of 3 times in one course. Infants who continued to have hemodynamically significant PDA after a first course of indomethacin and had no contraindications to additional treatment were given a second or more course of indomethacin for rescue at more than 48-hour intervals. We had used only indomethacin as a COX inhibitor because ibuprofen (another COX inhibitor) was first available in Japan in 2018.
Neurodevelopmental AssessmentAt 5 years of corrected age, a neuropsychological assessment (Kaufman Assessment Battery for Children [K-ABC]) was performed by trained psychologists. The K-ABC is a method for evaluating intelligence and achievement designed for children aged 2.5 to 12.5 years old (Kaufman et al. 1987) This multisubtest battery is composed of 5 scales: mental processing composite, sequential processing, simultaneous processing, achievement processing, and nonverbal. The mental processing composite scale can be interpreted as being similar to an intelligence quotient (IQ), which is age-standardized to a mean of 100. It is divided into sequential processing and simultaneous processing scales. The sequential processing scale measures short-term memory and consists of subtests that measure problem-solving skills with the emphasis is on following a sequence or order. The simultaneous processing scale examines problem-solving skills that involve several processes at once. The achievement scales provide an estimate of previous learning by using subtests that measure acquired knowledge and the application of skills. The nonverbal scales serve as a good estimate of intellectual potential in children who have problems in the areas of receptive or expressive language or who have language disorders.
DefinitionsGA was determined by early ultrasound scanning. SGA was defined as a weight and height below the 10th percentile for gestational age. RDS was defined according to clinical symptoms of respiratory distress in the first 24 hours of life and a need for surfactant administration. Intraventricular hemorrhage was defined as grade III or higher severe hemorrhage according to the classification (Papile et al. 1978). PVL was diagnosed based on magnetic resonance imaging according to the reported definition (Baker et al. 1988; Maalouf et al. 1999). Necrotizing enterocolitis was defined as Bell’s classification II or greater (Bell et al. 1978). Chronic lung disease was defined as the supplemental oxygen requirement at 36 weeks GA. Duration of persistent PDA is until the postnatal day when the closure of the DA was finally confirmed by echocardiography. In three patients with small PDA at discharge, the durations of patency of PDA were considered as the postnatal age at discharge. Neurodevelopmental impairment was defined as having either cerebral palsy, visual impairment, hearing impairment, or a K-ABC mental processing composite score of < 70.
Statistical AnalysisContinuous variables are represented by the median values and interquartile ranges (IQR), and categorical variables are represented as the number of cases (%). Data distribution was determined with the Shapiro-Wilk test. Differences between the groups were evaluated by the Mann-Whitney U test for continuous data and the χ2 test or Fisher exact test for categorical data. For statistical analysis, SPSS version 24.0 (IBM SPSS Statistics, IBM Corporation) was used, and a P value < 0.05 was considered significant.
A total of 99 infants with a GA < 29 weeks and a birth weight < 1,250 g were admitted. We excluded 3 infants who died of neonatal asphyxia, sepsis and gastrointestinal perforation during initial hospitalization. There were 68 patients in the closed ductus group and 28 patients in the persistent patent ductus arteriosus group. Two infants died in the closed ductus group, and 14 infants in the closed ductus group and 8 infants in the persistent patent ductus arteriosus group were lost to follow-up between discharge and an adjusted age of 5 years of corrected age. The data of the remaining 72 infants were assessed in this study: the closed ductus group (n = 52), the persistent patent ductus arteriosus group (n = 20) (Fig. 1). As summarized in Table 1, the perinatal characteristics and management of PDA of the preterm infants were not significantly different between those who were followed and assessed at 5 years of corrected age (n = 72) and those who were not assessed because followed in another referral clinic, lost to follow-up, or died between discharge and age 5 years (n = 24). Among the 96 infants, seven infants of the followed-up group and six infants of not followed-up group showed spontaneous closure of the DA without indomethacin administration.
We were thus able to follow up the 72 infants (Table 2). Among the 52 infants of the closed ductus group, 45 infants received indomethacin administration, while seven infants showed spontaneous closure of the DA. Antenatal steroid use, sex, Apgar scores, the rates of singleton, SGA, and the occurrence of RDS, intraventricular hemorrhage, PVL, necrotizing enterocolitis, retinopathy of prematurity with laser coagulation, chronic lung disease with home oxygen therapy were not significantly different between the two groups. GA (median [IQR]: 26.3 [2.3] vs. 25.6 [4.0]; P = 0.044) and Birth weight (861 [267] vs. 690 [443]); P = 0.014) was lower, surgical ligation rates were higher (3.8% vs. 25.0%; P = 0.015), and duration of persistent PDA were longer (median [range]:3.0 [1-13] vs. 50.5 [17-165]; P = 0.000) in the persistent patent ductus arteriosus group than in the closed ductus group.
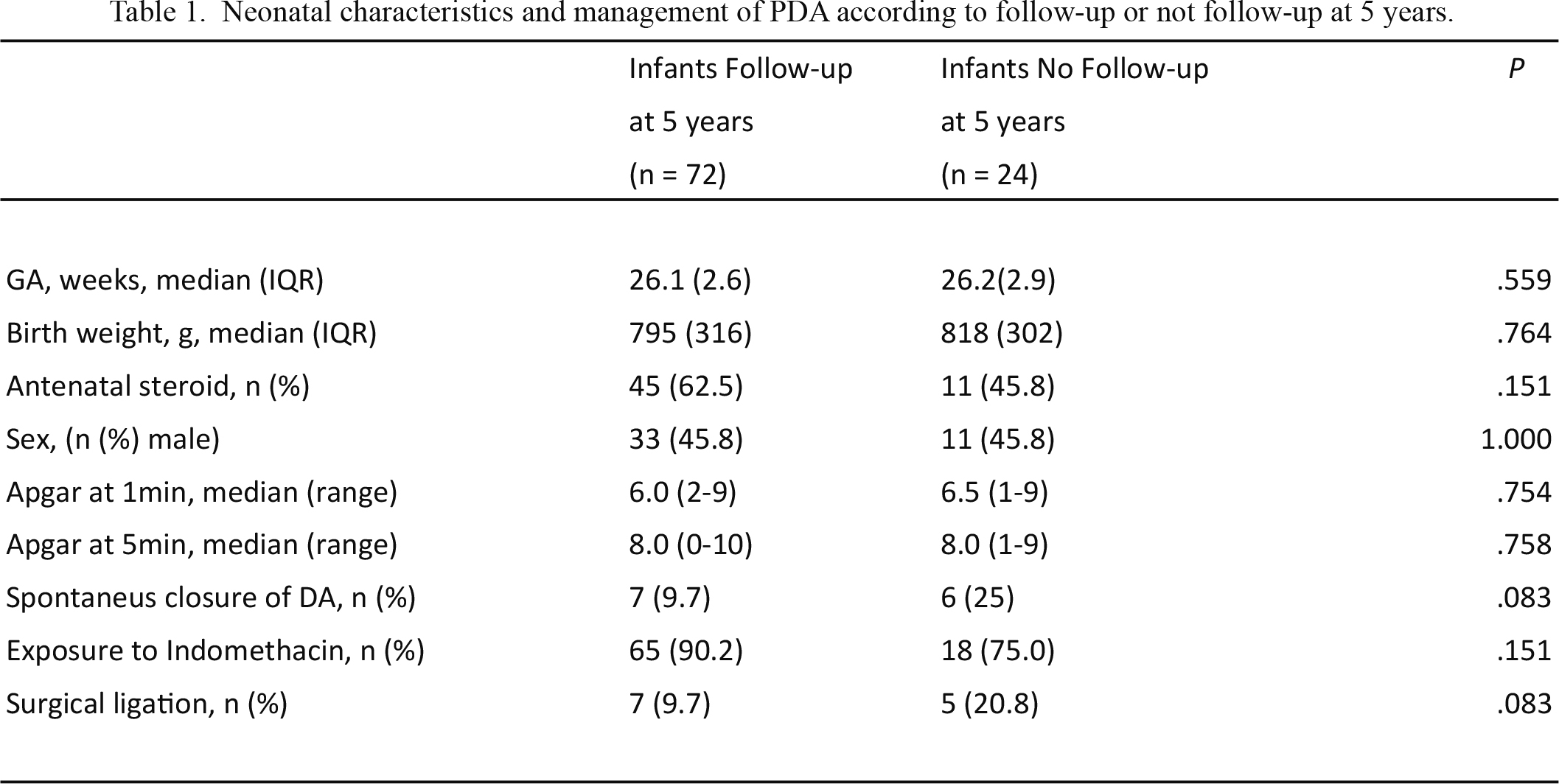
Neonatal characteristics and management of PDA according to follow-up or not follow-up at 5 years.
Values were statistically analyzed using tha Mann-whitney U test or χ2 test.
GA, gestational age; IQR, interquartile range; DA, ductus arteriosus.

Neonatal characteristics and neurodevelopmental impairment at 5 years corrected age according to the persistency of PDA.
Values were statistically analyzed using tha Mann-whitney U test or χ2 test.
GA, gestational age; IQR, interquartile range; SGA, small for gestational age; RDS, respiratory distress syndrome; IVH, intraventricular hemorrage; PVL, periventricular leukomalacia; NEC, necrotizing enterocolitis; ROP, retinopat of prematurity; HOT, home oxygen therapy; NDI, neurodevelopmental impairment.
In this study, eight children (15.4%) in the closed ductus group and three children (15.0%) in the persistent patent ductus arteriosus group did not complete the K-ABC test because of severe neurodevelopmental impairment. Eventually, we were able to perform the K-ABC test for 44 children in the closed ductus group and 17 children in the persistent patent ductus arteriosus group. One child among 17 children in the persistent patent ductus arteriosus group was determined neurodevelopmental impairment because the K-ABC score was less than 70. We did not find significant differences in K-ABC sores at 5 years of corrected age between the two groups: mental processing composite (median [IQR] 98 [18] vs. 92 [19]; P = 0.147), sequential processing (100 [16] vs. 92 [32], P = 0.240), simultaneous processing (101 [18] vs. 89 [18]; P = 0.050), achievement processing (94 [27] vs. 99 [33]); P = 0.612), and nonverbal abilities (98 [15] vs. 88 [16]; P = 0.100) (Fig. 2).
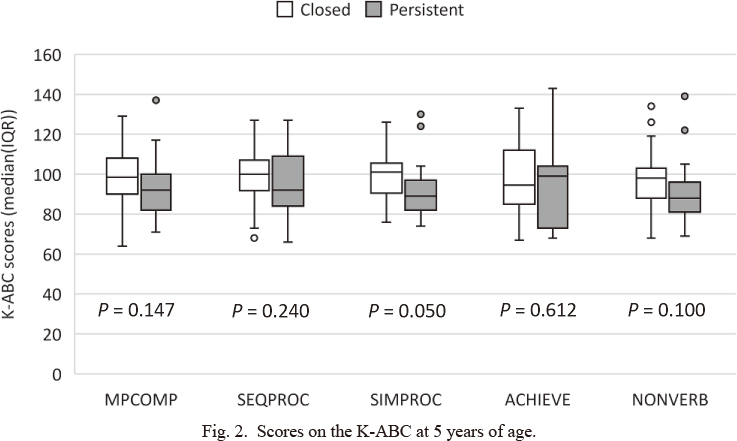
Scores on the K-ABC at 5 years of age.
Shown are the scores on the K-ABC at 5 years of corrected age in the closed ductus group (n = 44) and persistent patent ductus arteriosus group (n = 17).
Values for the different subtests are shown as median and interquartile range. Values were statistically analyzed using the Mann-Whitney U test.
MPCOMP, mental processing composite; SEQPROC, sequential processing; SIMPROC, simultaneous processing; ACHIEVE, achievement scales; NONVERB, nonverbal abilities.
In this study, under our conservative management of PDA, we found no significant differences in K-ABC scores at 5 years of corrected age between the closed ductus group (DA closed within 14 days after birth) and the persistent patent ductus arteriosus group (DA persisted for more than 14 days after birth). Some studies have reported that conservative management of PDA did not increase the risk of mortality, chronic lung disease, retinopathy of prematurity, intraventricular hemorrhage, necrotizing enterocolitis, or neurodevelopmental impairment in preterm infants (Jhaveri et al. 2010; Wickremasinghe et al. 2012; Clyman et al. 2019). This is the first study that examined more long-term neurodevelopmental outcomes after the conservative management of PDA in preterm infants. The results of our study suggest that conservative management for PDA even if exposed to more prolonged PDA did not affect the neurodevelopmental outcomes of 5-year corrected age in preterm infants.
The main reason for applying a conservative approach is that spontaneous permanent DA closure occurs in > 34% of extremely low birth weight (ELBW) neonates (Koch et al. 2006). In addition, Laan reported that cerebral and renal oxygen saturation and extraction were not affected by hemodynamically significant PDA in preterm infants treated within 2 weeks after birth (van der Laan et al. 2016). Moreover, large cohort studies have reported an association between surgical DA ligation and poor neurodevelopmental outcomes in preterm infants (Madan et al. 2009; Mirea et al. 2012; Bourgoin et al. 2016). We found that 9.7% (7/72) of the subjects in this study demonstrated spontaneous DA closure, while a lower late than was achieved in the previous study. In addition, a significant number of the infants had spontaneous or medical closure of their DA and did not undergo DA ligation, although 25% of the infants in the persistent patent ductus arteriosus group underwent surgical ligation eventually.
On the other hand, when choosing a conservative approach, we consider the negative effects in preterm infants with more prolonged PDA exposure. Previous observational studies have shown that prolongd PDA is related to increased mortality and morbidity in very preterm infants (Chorne et al. 2007; Lemmers et al. 2008). Vida et al. (2009) reported that surgical ligation should be performed after the failure of medical treatments. Lemmer et al. (2008) suggested that persistent PDA compromises the perfusion and oxygenation of the preterm brain and negatively affects neurodevelopmental outcomes. However, in this study, even though infants with persistent patent ductus arteriosus were exposed to PDA shunts for longer durations, their rates of morbidities (intraventricular hemorrhage, PVL, necrotizing enterocolitis, retinopathy of prematurity, and chronic lung disease with home oxygen therapy) and neurodevelopmental outcomes did not change.
Furthermore, the timing of surgical ligation may be important. Sung et al. (2014) showed that delayed ligation (after more than 2 weeks after birth) decreased the risk for mortality or morbidities in extremely preterm infants born at 23-25 weeks of gestation. In our results, although surgical ligation rates were significantly higher in the persistent patent ductus arteriosus group (3.8% vs 25.0%), the neurodevelopmental outcomes did not change. We speculate that late surgical ligation appears to be more advantageous than early ligation during the immature period. Conservative management of PDA could avoid unnecessary surgical ligation and allow the infant’s maturity to increase until the optimal timing for surgical ligation is reached.
The limitations of the study are its retrospective nature, the small number of included infants, and its single-center design. We could not completely match infants with closed ductus to those with persistent patent ductus arteriosus; the infants in the persistent patent ductus arteriosus group had lower GA and birth weights than were recorded in the closed ductus group. However, the neurodevelopmental outcomes associated with persistent patent ductus arteriosus were not significantly different from those associated with closed ductus despite the lower GA and birth weights of the infants in the former group. It is, therefore, unlikely that the results of the present study were influenced by bias related to GA and birth weights.
In conclusion, under our conservative management of PDA, we did not find an association between persistent PDA and neurodevelopmental outcomes at 5 years of corrected age. These results indicate that a conservative approach for PDA, even in the case of prolonged PDA, does not increase the risk of long-term neurodevelopmental impairment.
The authors declare no conflict of interest.