2019 年 249 巻 3 号 p. 185-192
2019 年 249 巻 3 号 p. 185-192
Knowledge of branching patterns of external carotid artery (ECA) is essential for planning and execution of head and neck surgeries. Digital subtraction angiography (DSA) images of 532 ECAs from 302 consecutive patients were retrospectively evaluated. We classify the branch variants of ECA into three types, simply based on the number of branches arising close together. Type A, Type B, and Type C variants are defined as two, three, and four or more branches of ECAs arising at a common point from the proximal ECA, respectively. In this classification, the distal ECA was counted as one branch. Of 532 ECAs, Type A was found in 344 ECAs (64.6%) of 237 patients (78.5%), Type B in 134 ECAs (25.2%) of 110 patients (36.4%), and Type C in 54 ECAs (10.2%) of 49 patients (16.2%). The distance from the common carotid artery (CCA) bifurcation to the first branch of ECA with Type C was 14.7 ± 6.6 mm; its distance is shorter compared with Type A (21.8 ± 15.6 mm) and Type B (20.6 ± 8.9 mm) (P < 0.05). The position of CCA bifurcation with Type C was detected at the third-fourth junction cervical vertebral level or higher in 52 of 54 ECAs (96.3%), significantly higher than those of the other types (P < 0.05). In conclusion, Type C ECA has aggregated vessels with short distance from CCA and high position of CCA bifurcation. Type C ECA is not uncommon; thus, special consideration should be paid to avoid complications during surgeries.
Knowledge of the branching pattern of ECA is important for head and neck surgeries or performing selective intra-arterial chemotherapy for head and neck cancer (Yonenaga et al. 2011). Interventional radiologists, neurosurgeons, vascular, craniofacial, and neck surgeons should be aware of branch variants of ECA to obtain the correct interpretation of radiological images, for planning safe surgical approaches, and to execute surgeries including carotid endarterectomy (CEA) and carotid artery stenting (CAS) as a representative example of neuroendovascular surgeries.
The external carotid artery (ECA) has eight named branches distributed to the head and necks. It gives off the superior thyroid artery, lingual artery (LA), facial artery (FA), occipital artery (OA), and ascending pharyngeal artery (APA) in the carotid triangle (Standring 2005). After these branches, the ECA branches off into the posterior auricular artery (PAA), maxillary artery (MA), and superficial temporal artery. Some common trunks, such as thyrolingual, linguofacial, thyrolinguofacial, occipitoascending pharyngeal, and occipitoauricular trunks, were also identified (Zümre et al. 2005; Tanaka et al. 2010; Devadas et al. 2018).
Variants of the branching pattern of ECA have been discussed in the literature (Gluncic et al. 2001; Standring 2005; Tanaka et al. 2010; Thwin et al. 2010; T et al. 2010; Kishve et al. 2011; Rao 2011; Yonenaga et al. 2011; Cappabianca et al. 2012; Cvetko 2014; Ogeng’o et al. 2015; Kawai 2016). However, the classification for branch variants of ECA is not unified because the previous analyses were performed using small number of cases (Gluncic et al. 2001; T et al. 2010; Thwin et al. 2010; Kishve et al. 2011; Rao 2011), or focused only on data of interest (Standring 2005; Tanaka et al. 2010; Yonenaga et al. 2011; Ogeng’o et al. 2015).
The widespread four-type classification of ECA is as follows: type I, separate origin of the superior thyroid artery, LA, and FA; type II, the LA and FA originate together from a common trunk (linguofacial trunk); type III, the superior thyroid artery and LA originate together from a common trunk (thyrolingual trunk); and type IV, the superior thyroid artery, LA, and FA originate together from a common thyrolinguofacial trunk (Standring 2005). This classification focused only on the front branch of ECA.
Ogeng’o et al. (2015) took particular note of the branch patterns of ECA based on the number of branches arising close together from a common point of the ECA, as the trifurcation, quadrifurcation, and pentafurcation of ECA. In the trifurcation, the ECA after the origin of superior thyroid artery trifurcated into the linguofacial trunk, APA, and distal ECA. In the quadrifurcation, the ECA branched into the LA, FA, APA, and distal ECA. In the pentafurcation, ECA branched into the superior thyroid artery, LA, FA, and APA arose within close proximity from a common short stem. In addition to these branch variants, they defined the typical branch pattern as the artery having a long stem from which the superior thyroid artery, LA, FA, and APA arose while the ECA ended by bifurcating into the MA and superior temporal artery. The bifurcation was defined as the ECA after giving the superior thyroid artery branched into a linguofacial trunk and distal ECA. Ogeng’o et al. (2015) analyzed 224 ECAs from 112 cadavers, the largest number of ECA samples used for examining the branch patterns. However, they did not describe the data whether the OA was involved in the formation of quadrifurcation and pentafurcation or not. In contrast, several case reports mentioned that the OA was involved in the quadrifurcation branch variant of ECA (Gluncic et al. 2001; T et al. 2010; Thwin et al. 2010; Kishve et al. 2011).
The present study, using angiographic images, classified the branch variants of ECA into three types simply based on the number of branches arising close together from a common stem of proximal ECA. In this classification, the distal ECA was counted as one branch. Type A, B, and C variant was defined as two, three, and four or more branches of ECAs arising at a common point from the proximal ECA, respectively. We also analyzed several characteristics of each variant, including its frequency, the distance from the common carotid artery (CCA) bifurcation to the first branch of ECA, and the correlation between the position of CCA bifurcation and the cervical vertebral level.
In this report, we would like to advocate the simple classification of ECA for the daily usage.
This study evaluated digital subtraction angiography (DSA) images of 532 ECAs from 302 consecutive patients aged from 15 to 94 years treated at Kitasato University Hospital from January 2014 to March 2016. Their clinical characteristics are summarized in Table 1. This is a retrospective study; thus, the bilateral external carotid artery angiography was performed for 230 patients, not for all the patients.
All DSA procedures were performed in the angiographic suite (syngo X Workplace VB21c; Siemens Healthcare GmbH, Erlangen, Germany). Arterial catheterization was performed through the radial artery or femoral artery to the CCA. After placement of the angiographic catheter, flush angiography from the CCA was performed to evaluate the CCA bifurcation, neck internal carotid artery (ICA) stenosis, and the branching variation of the ECA. Selective angiograms were obtained using a 4-Fr modified Simmons catheter® (Medikit, Tokyo, Japan). Iodine contrast medium was used for all procedures. Other procedures were performed according to the indications for angiographic intervention or treatment.
Images were obtained from at least two different angles (frontal and lateral views). Three-dimensional (3D) reconstruction images using rotational DSA (3D DSA) was performed for some cases. Their branching variations were evaluated by a qualified neuroendovascular surgeon and two other qualified neurosurgeons. All branches from the ECA of our interest were superior to the level of CCA bifurcation in the carotid triangle, specifically the LA, FA, OA, APA, thyrolingual, linguofacial, thyrolinguofacial, and occipitoascending pharyngeal trunks. In this study, the superior thyroid artery branching only from the ECA was included. We evaluated the number of branches arising close together from a common point of the ECA. The distal ECA was counted as one branch. All the common trunks were regarded as one branch. The APA could sometimes not be recognized on DSA; in such cases, APA was not counted as one branch. Branch variants of the ECA were divided into three types: Type A, all individual branches arising separately from the proximal ECA (the number of branches arising from the proximal ECA is two); Type B, three branches of ECAs arising close together at a common point from the proximal ECA; and Type C, four or more branches of ECAs arising close together at a common point from the proximal ECA.
The distances from the CCA bifurcation to the first branch of ECA and the correlation between the position of CCA bifurcation and the cervical vertebral level were analyzed from DSA images.
This study was approved by the institutional ethics committee of Kitasato University Hospital (B19-097, September, 12, 2019). Patient consent was neither required nor sought because this was retrospective observational study. Instead, we provided a means to opt out from this study on the internet to the patients.

Clinical characteristics of the cases.
We compared distance from the CCA bifurcation to the first branch of ECA, among three type classification. Analysis of covariance following Dunnett’s post-hoc analysis was applied. Next, we investigated the association between prevalence of the three type variants and CCA bifurcation level using univariate logistic regression model. CCA bifurcation level were divided into three groups, higher third cervical vertebral level (C3); C3 or third-fourth junction cervical vertebra (C3/4); and fourth cervical vertebra (C4) or lower. Two-sided P < 0.05 was regarded as statistical significance. Statistical software Stata13.1 (StataCorp) and R-3.6.1 (R Foundation for Statistical Computing) were used for analysis.
Branching variations of the ECA are classified into the following three types (Fig. 1), based on the DSA findings of 532 ECAs from 302 patients, including 230 patients with both-side carotid angiograms. The same branch variant was observed on the right and left sides in 136 patients (59.1%).
Type A: The number of branches arising from the proximal ECA is two (Fig. 1). Type A was found in 344 vessels (64.6%; right, 175; left, 169) of 237 patients (78.5%). Among 230 patients with both-side carotid angiograms, bilateral Type A was found in 107 patients (46.5%); Type A and Type B, 58 patients (25.2%); and Type A and Type C, 24 patients (10.4%).
Type B: The number of branches arising from the proximal ECA is three (Fig. 1). Type B was found in 134 vessels (25.2%; right, 61; left, 73) of 110 patients (36.4%). Bilateral Type B was found in 24 patients (10.4%); and Type B and Type C, 12 patients (5.2%).
Type C: The number of branches arising from the proximal ECA is four or more (Fig. 1). Type C was found in 54 vessels (10.2%; right, 24; left, 30) of 49 patients (16.2%). The representative images of Type C are shown in Fig. 2. Bilateral symmetrical Type C branch variants were present in 5 patients (2.2%) out of 230 patients with both-side carotid angiograms.
Both-side carotid angiograms were available for 41 patients with Type C. Among these 41 patients, bilateral symmetrical Type C was found in 5 patients (12.2%); Type C and Type A, 24 patients (58.5%); and Type C and Type B, 12 patients (29.3%).
The compositions of branches involved in Type C were divided into the twelve patterns (Table 2). The top three branching patterns were as follows: LA, FA, OA, and distal ECA, 13 cases (24.0%); linguofacial trunk, OA, APA, and distal ECA, 13 cases (24.0%); and LA, FA, OA, APA, and distal ECA, 6 cases (11.1%; Fig. 3).
The distance from the CCA bifurcation to the first branch of ECA was 21.8 ± 15.6 mm in Type A and 20.6 ± 8.9 mm in Type B. By contrast, the distance in Type C was 14.7 ± 6.6 mm, and significantly shorter than those of the other types (Dunnett’s post-hoc test between Type A and Type C; P = 0.002 and between Type B and Type C; P = 0.032).
When the most common C3 or C3/4 level bifurcation group was regarded as reference group, Type C was significantly uncommon in the group with C4 level or lower CCA bifurcation (Odds Ratio [95% confidence interval]: 0.06 [0.015 to 0.24], P < 0.001) (Fig. 4). The position of CCA bifurcation with Type C was detected at the C3/4 level or higher in 52 of 54 ECAs (96.3%) (Table 3).

Illustrations of our three types classification for branch variant of the external carotid artery (ECA) with incidences.
Branch variants of the ECA were divided into three types: Type A, all individual branches arising separately from the proximal ECA (the number of branches arising from the proximal ECA is two, including distal ECA); Type B, three branches of ECAs arising close together at a common point from the proximal ECA (white arrow head); and Type C, four or more branches of ECAs arising close together at a common point from the proximal ECA (black arrow head). The black double-headed arrows indicate the common carotid artery bifurcation level of cervical vertebra. Note the higher position of the bifurcation level in Type C.
APA, ascending pharyngeal artery; CCA, common carotid artery; ECA, external carotid artery; FA, facial artery; ICA, internal carotid artery; LA, lingual artery; OA, occipital artery.

Lateral views of digital subtraction angiograms (DSAs) showing representative 10 cases of Type C.
The distances from the common carotid artery (CCA) bifurcation to the first branch of ECA were indicated below the each DSA. The average length from CCA bifurcation to the first branch of the ECA was 14.7 ± 6.6 mm (n = 54 vessels).
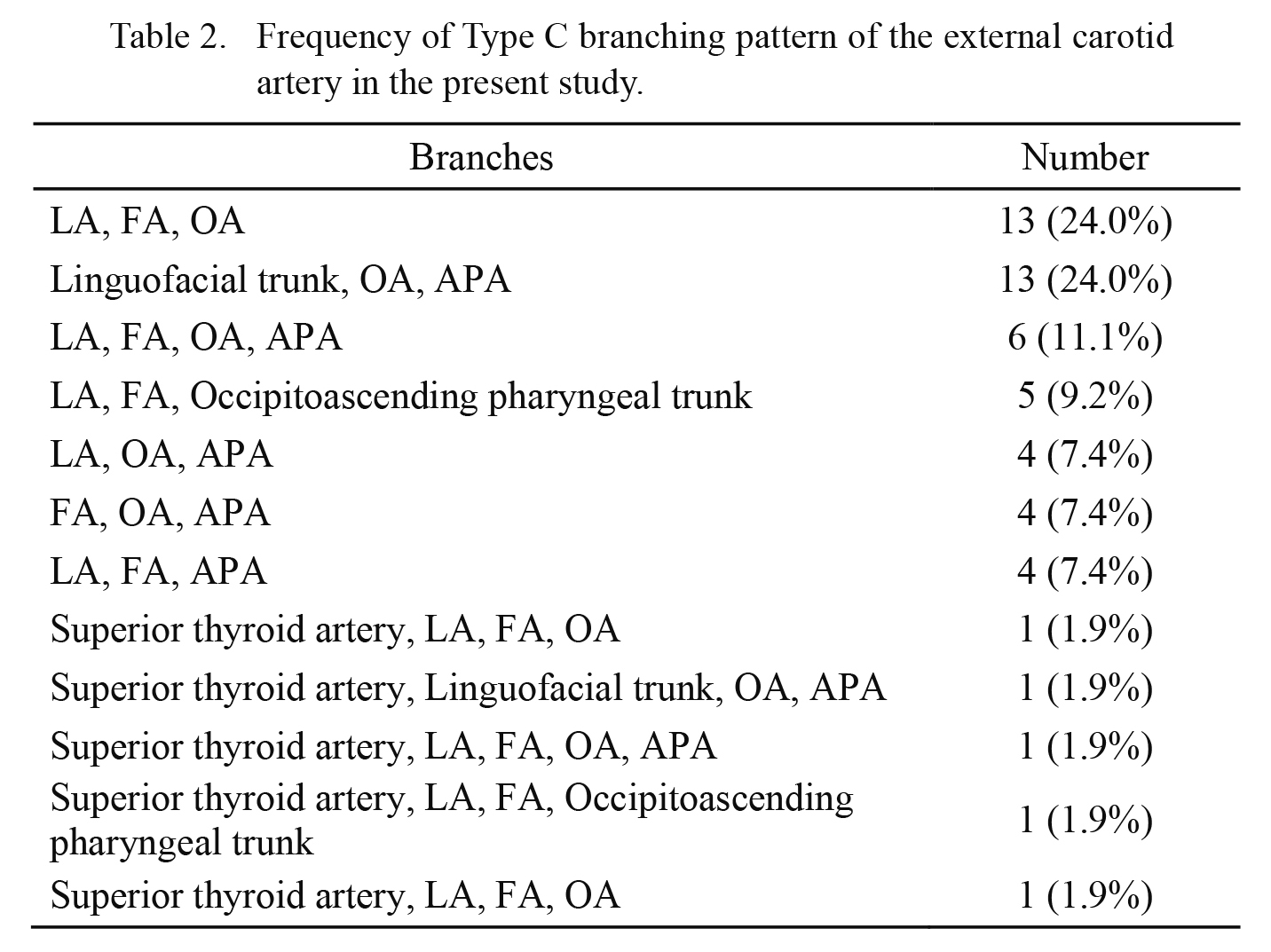
Frequency of Type C branching pattern of the external carotid artery in the present study.
LA, lingual artery; FA, facial artery; OA, occipital artery; APA, ascending pharyngeal artery.

Representative angiographic finding of external carotid artery (ECA) with Type C.
Shown are digital subtraction angiogram (DSA) and 3-dimensional (3D) reconstruction images, obtained with rotational DSA (3D DSA). Lateral views of left common carotid artery DSA (A) and 3D DSA (B, magnified view; C, overall view), depicting left internal carotid artery stenosis and Type C branching pattern of ECA. Branches from the proximal external carotid artery (ECA) are five as follows, the lingual artery, facial artery, ascending pharyngeal artery, occipital artery, and distal ECA.
APA, ascending pharyngeal artery; CCA, common carotid artery; ECA, external carotid artery; FA, facial artery; ICA, internal carotid artery; LA, lingual artery; MA, maxillary artery; OA, occipital artery.

The common carotid artery (CCA) bifurcation level of cervical vertebra in each external carotid artery (ECA) branch variant of the three-type classification.
The group name of “Higher than C3” includes the CCA bifurcation level of second cervical vertebra and second-third junction cervical vertebra. “C3 or C3/4” includes the bifurcation level of third cervical vertebra and third-fourth junction cervical vertebra. “Lower than C4” includes the bifurcation level of fourth cervical vertebra, fourth-fifth junction cervical vertebra, and fifth cervical vertebra. There were no cases with the CCA bifurcation level of higher than first-second junction cervical vertebra and lower than fifth-sixth junction cervical vertebra. CCA bifurcation level with Type C lower than C4 was lower than those of the other variants (※P < 0.05). The ordinate (%value) indicates the frequency of CCA bifurcation level in each type.
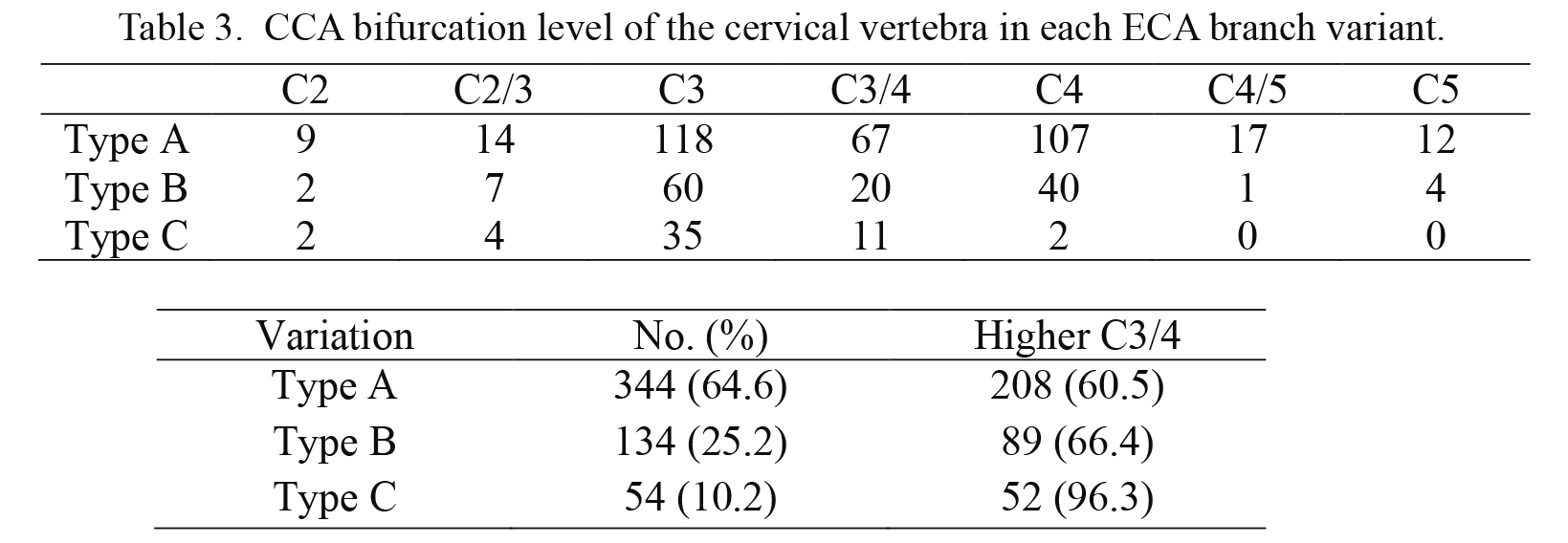
CCA bifurcation level of the cervical vertebra in each ECA branch variant.
C2, second cervical vertebra; C2/3, second-third junction cervical vertebra; C3, third cervical vertebra; C3/4, third cervical vertebra and third-fourth junction cervical vertebra; C4, fourth cervical vertebra; C4/5, fourth-fifth junction cervical vertebra; C5, fifth cervical vertebra.
The present study proposes the three-type classification for branch variants of ECA, simply based on the number of branches arising close together at a common point from the proximal ECA. Type A is that all individual branches arise separately from the proximal ECA. The number of branches arising from the proximal ECA is two, including the distal ECA. Type B is that three branches arise close together including the distal ECA. Type C is defined as four or more branches arising close together including the distal ECA.
In the first place, we determined the incidence of the branch variants of ECA using DSA results from a large consecutive series. In the results, the frequency of Type A, B, and C was 64.6%, 25.2% and 10.2%, respectively. A cadaveric study using a black Kenyan population showed that the typical pattern of branching, bifurcation, trifurcation, quadrifurcation, and pentafurcation, was observed in 41.1%, 17.9%, 26.8%, 8.9%, and 5.3% of cases, respectively (Ogeng’o et al. 2015). In comparison with their study, our type A includes the typical branch pattern and the bifurcation of them. Our type B is the same as the trifurcation. Our type C includes the quadrifurcation and pentafurcation; thus, the frequency of each type of our classification was similar to the results of Ogeng’o et al. (2015).
Next, we focused on Type C. Previous reports on cadavers concerning this characteristic branch variant of the ECA are summarized in Table 4 (Gluncic et al. 2001; Thwin et al. 2010; T et al. 2010; Kishve et al. 2011; Rao 2011; Ogeng’o et al. 2015). We can recognize that various branches and trunks were involved in the composition of this branch variant of the ECA. Five of these six papers were case reports analyzing a human cadaver (Gluncic et al. 2001; Thwin et al. 2010; T et al. 2010; Kishve et al. 2011; Rao 2011). Gluncic et al. (2001) reported a case with a quadrifurcation into the superior thyroid artery, LA, OA, and distal ECA. Each of Thwin et al. (2010) and T et al. (2010) reported the ECA after the origin of superior thyroid artery quadrifurcated into the LA, FA, OA, and distal ECA. Rao (2011) reported a case in which all eight branches arose close together from a common point just above the origin of the ECA. Like these previous case reports, various branches and trunks were involved in our Type C (Table 4). To classify the branch patterns of ECA based on these diverse variations is so complicated and impractical. For the daily usage, our three-type classification for branch variants of ECA, simply based on the number of branches arising close together at a common point from the proximal ECA, must be convenient.
Interestingly, Kishve et al. (2011) reported a case with simultaneous Type C branching on both sides. This was the only case of bilateral Type C branching of ECA, so far. In our study, the 5 cases of bilateral Type C variant of the ECA had 2.2% probability in 230 patients with the data of both side carotid angiograms. The fact that 12.2% of cases with Type C had the contralateral Type C ECA branching pattern is worthy for remark.
In the second place, our study demonstrated that the distance from the CCA bifurcation to the first branch of ECA was mean 14.7 ± 6.6 mm in our cases of Type C. This length is statistically shorter than those of the other variations (P < 0.05). Previously, Ogeng’o et al. (2015) pointed out that the pentafurcation showed the early division within the carotid triangle in 12 out of 224 cadavers (5.3%). However, the precise distance from the CCA bifurcation to the first branch of ECA has not been reported yet. This short distance of proximal ECA in Type C should be recognized during head and neck surgery or neuroendovascular therapy.
In the third place, we analyzed the correlation between the ECA branch variations and the position of the CCA bifurcation. The CCA usually bifurcates at the level of the upper border of the thyroid cartilage into the ECA and ICA (Standring 2005). Zümre et al. (2005) did a study of the bifurcation levels of the CCA and origin variations of the branches of the ECA in 20 human fetuses. In their analyses, the bifurcation level of the CCA was determined to be 55% at the C3 level, 35% at the C4 level, 10% at the C5 level on the right side and 60% at the C3 level, 40% at the C4 level on the left side. Thus, the CCA usually bifurcates at the level of the C3 level. Recently, a higher level of origin was noted in 20 of 80 cadavers (25%) (Devadas et al. 2018). They concluded that the higher level of the carotid bifurcation exhibited a great degree of anatomical variability. Our study showed that 96.3% of CCA bifurcation level with Type C was at C3/4 or higher. The rate in CCA bifurcation level with Type C lower than C4 was significantly lower than those of the other variations (P < 0.05). These results are consistent with the previous reports of the quadrifurcation that analyzed cadavers (Gluncic et al. 2001; Thwin et al. 2010; T et al. 2010; Kishve et al. 2011). The CCA was bifurcated at the level between C2 and C3 in the case of Gluncic et al. (2001), and Thwin et al. (2010) reported that the CCA bifurcation level was as high as C2, corresponding to the hyoid bone. Kishve et al. (2011) also reported the association of high carotid bifurcation at 1 cm above the greater cornu of hyoid bone and bilateral three branches, including linguofacial trunk, OA, APA, and the distal ECA, arising close together from a common point just above the origin of the ECA. Thus, the higher position of CCA bifurcation is associated with the variant, equivalent to Type C. The development of ECA is a complicated process of angiogenesis and remodeling which includes annexation and regression of vessels (Mustafa et al. 2016). The variation in this developmental process results in long CCA with aggregated ECA branches; thus, high CCA bifurcation must be one unique feature of Type C.
There are several limitations. First, this is the most extensive study for evaluation of branch patterns of ECA, but it is retrospective. We could not perform complete bilateral external carotid artery angiograms for all 302 consecutive patients. Thus, our data might have some bias. Second, we could not discuss the ethnic differences of variations in branching of ECA, because our materials were not the healthy volunteers, but the patients suffering from a disease, Third, most of the branch variation of ECA was evaluated by images obtained from two different angles (frontal and lateral views), resulting the APA could not be visualized in some cases. At this point, our angiographical evaluation is inferior to the data obtained by cadaver dissection. However, even in the angiographical evaluation, 3D DSA can demonstrate the precise stereoscopic anatomy of ECA with the APA (Fig. 3).
In conclusion, using 3D DSA, we propose the three-type classification for branch variants of ECA, simply based on the number of branches arising close together at a common point from the proximal ECA. Our classification with angiographic images is more practical in clinical usage. Indeed, we are able to show that about 16.2% of analyzed subjects carry the Type C branching pattern (10.2% of the ECA). Importantly, the Type C branching pattern is characterized by the short distance from the CCA bifurcation to the first branch of ECA and by the higher cervical vertebral position of its CCA bifurcation. This unique Type C with aggregated ECA branches needs to be paid attention to avoid complication during surgeries.
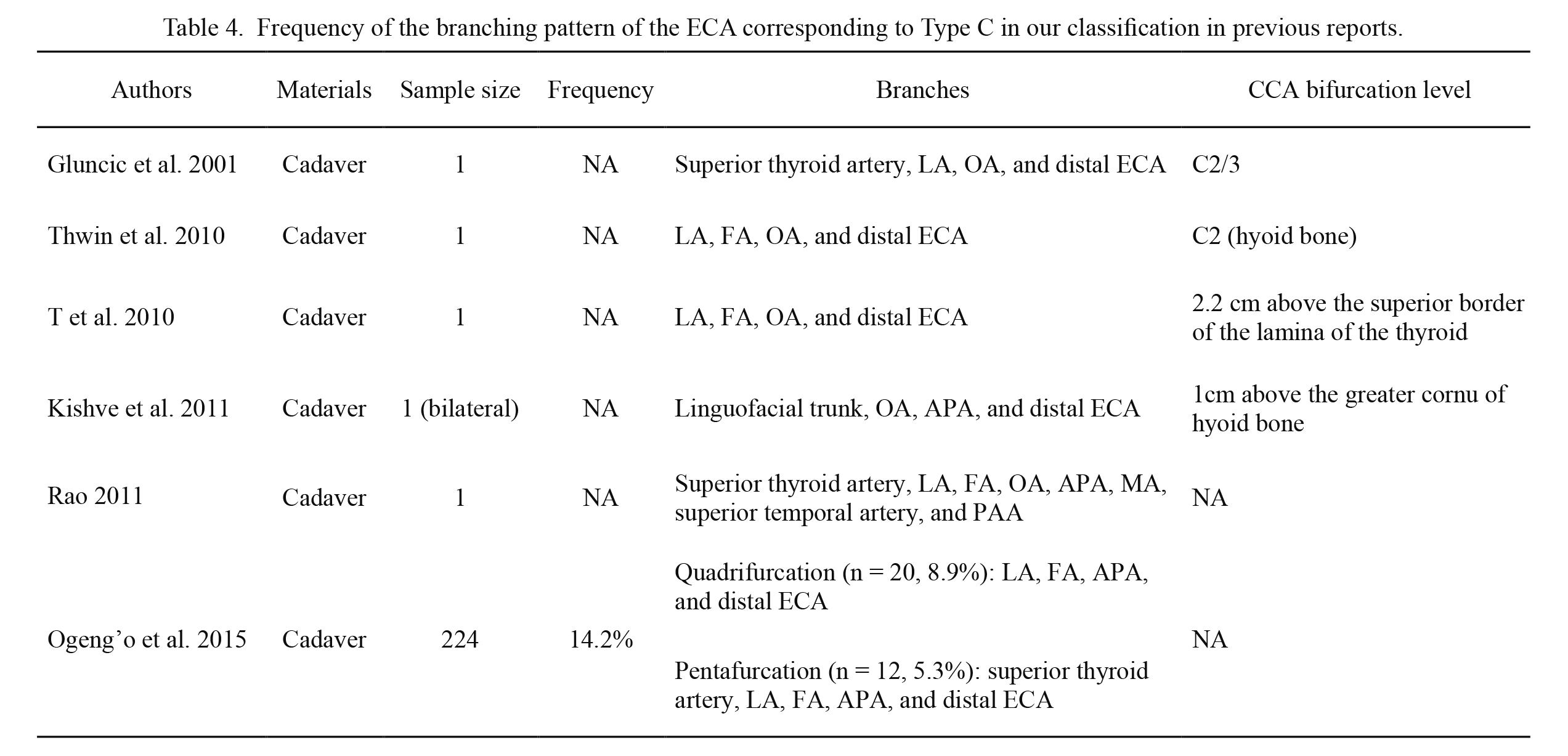
Frequency of the branching pattern of the ECA corresponding to Type C in our classification in previous reports.
NA, not applicable, LA, lingual artery; OA, occipital artery; ECA, external carotid artery; FA, facial artery; APA, ascending pharyngeal artery; MA, maxillary artery; PAA , posterior auricular artery.
The authors declare no conflict of interest.