2020 Volume 251 Issue 2 Pages 135-145
2020 Volume 251 Issue 2 Pages 135-145
The high rates of mortality and hospitalization among elderly asthmatics, as well as their increasing healthcare costs have become an important public health issue. It would be worthwhile to assess whether inhaled corticosteroid (ICS) can resolve these problems. To explore ICS prescription rates for elderly asthmatics and the factors influencing them and to investigate their association with hospitalization and healthcare costs, we analyzed data from the National Health Insurance Claims Database for the same time frame (December 1 to February 28) across three different periods (2011-2012; 2014-2015; and 2017-2018), from which we identified 6,619, 5,619, and 6,880 elderly individuals, respectively. The prescription rates of ICS increased (52.8%, 65.5% and 68.8%, in the first, second and third survey period, respectively) and inversely the hospital admission rates declined (3.7%, 3.2% and 2.5%, in the first, second and third survey period, respectively). The total healthcare costs per month were significantly lower for patients who received ICS-containing regimens than for those who did not. A multivariate analysis revealed that increasing age, rural residence, receiving a prescription from a clinic, hospital admission, and prescription of asthma medications other than ICS were associated with non-prescription of ICS, whereas cross-boundary treatment increased the ICS-prescription rate. Our study suggests that increases in the prescription rate of ICS are associated with reduced hospital admission rates and lower medical costs in the real-world. ICS prescription rates in rural areas and at clinics, which remain low, need to be increased.
Asthma is the most common chronic respiratory disease worldwide. In recent decades, both asthma prevalence and incidence have been increasing among individuals ≥ aged 65 years or older (GBD 2015 Chronic Respiratory Disease Collaborators 2017). High rates of mortality and hospitalization among elderly asthmatics have become an important public health issue (Moorman et al. 2012). Approximately 50% of those who die of asthma in the United States are elderly (Stupka and deShazo 2009), and 1,728 people lost their lives to asthma in Japan in 2013, of which 90% were people ≥ aged 65 years or older (Ichinose et al. 2017). Inhaled corticosteroid (ICS) is reported to help reduce the risk of re-hospitalization and all-cause mortality in elderly asthmatics (Sin and Tu 2001); the Japanese guidelines for adult asthma recommend ICS as the first choice for the treatment of elderly patients (Ichinose et al. 2017). However, previous studies have demonstrated that elderly asthmatics are treated with ICS less frequently than younger patients (Navaratnam et al 2008) and that most elderly asthmatics admitted to emergency departments for asthma symptoms were not using ICS (Banerji et al 2006). Because there is little information on the real-world management of geriatric asthma in Japan, it is important to determine the rate at which ICS is prescribed for elderly asthmatics, to investigate their association with hospitalization, and to identify factors influencing the non-prescription of ICS.
Another pressing social issue is the tendency for older people to incur relatively high medical costs (Plaza et al. 2000). In elderly asthmatics with several comorbidities, exacerbation of asthma symptoms is frequent, leading to increased need for medication, outpatient hospital visits, and hospital admissions (Banerji et al. 2006; Dunn et al. 2018); this also increases the costs of asthma to the patient and society. The costs of asthma vary from country to country, and detailed data on these costs in Japan are limited (Miyamoto et al. 1999; Morishima et al. 2013; Inoue et al. 2019).
In recent years, clinical and epidemiologic studies using electronic databases have become feasible, and a few Japanese studies on subjects with asthma have been published (Atsuta et al. 2018; Tomita et al. 2019; Inoue et al. 2019; Nagase et al. 2020). The use of claims data has the advantage of providing information on the treatment provided by both non-specialist doctors and specialists in medical institutions, which is free of selection bias (Dilokthornsakul et al. 2019). Furthermore, the integration of claims data with drug claims data allows not only the investigation of the status of treatment but also interregional comparisons of medical costs (Jacob et al. 2016; Libutzki et al. 2019). These data comprise an important foundation for improving disease management and can be useful in formulating future healthcare policies. In particular, because of the very large number of elderly individuals enrolled, the National Health Insurance (NHI) Database can be an extremely useful tool for the assessment of the health management status of older people (Iihara et al. 2019; Tamaki et al. 2019).
In this study, we analyzed the NHI Claims Database to explore ICS prescription rates among elderly asthmatics and to investigate their association with hospitalization and healthcare costs; we also analyzed factors influencing the non-prescription of ICS.
We analyzed the NHI receipt data for medical fees and drug prescriptions in all of the municipalities in Oita Prefecture, which is located in the southern area of Japan. We were allowed access to three months of data, which was provided by the NHI Federation. We analyzed data from three periods: December 1, 2011 to February 28, 2012 (first survey period), December 1, 2014 to February 28, 2015 (second survey period), and December 1, 2017 to February 28, 2018 (third survey period). All of the claims for each individual were linked before anonymizing the data. The variables extracted from the dataset included the following: demographics (i.e., age, sex, home address, address of the medical institution where the individuals were treated, and history of hospital admission), codes for asthma (J45 and J46) based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), the mean value of total medical costs per month, and the prescription codes of asthma-related drugs. When the medical institution that provided the treatment and the patient’s home were located in different municipalities, this was defined as a cross-boundary treatment.
This study was approved by the ethics committee of Oita University Hospital (approval no. 1252). Written consent was obtained from each municipality for the use and analysis of its health insurance claims data.
Extraction of data on asthma patientsPatients whose health insurance claims were marked with any of the ICD-10 asthma diagnosis codes (J45 or J46) and who had been prescribed asthma medications (ICS, combination of ICS/long-acting beta-2 agonists [LABA], theophylline, beta-2 agonists, leukotriene receptor antagonists [LTRA], or omalizumab) at least once during the survey period were coded as asthma patients during each of the three-month survey periods. From this group, those who were 65 years of age or older were included in the analysis population as elderly asthmatics.
The prescription rate of each drug was calculated as the proportion of patients who received a prescription at least once in the three-month period. The prescriptions of either an ICS or ICS/LABA were defined as ICS-containing regimens. In addition, we measured the separate prescription rates of ICS and ICS/LABA in the second and third survey periods. The beta-2 agonists identified in this study included short-acting beta-2 agonists, as well as oral beta-2 agonists and tulobuterol patches.
Definitions of geographical areas and medical institutionsThe statistics on the total population and those 65 years of age or older in Oita Prefecture and its constituent municipalities were obtained from the Oita Prefectural Government website (http://www.pref.oita.jp/site/toukei/index-cpe.html). The number of people enrolled in the NHI each year was obtained from the Oita NHI Organization website (http://www.pref.oita.jp/site/toukei/index-cpe.html). To assess the differences between geographical areas, Oita City, where the prefectural government offices are located, was defined as urban, and all other areas were defined as rural, including isolated areas, such as remote islands and mountainous areas. For the purpose of this analysis, medical institutions with nineteen or fewer beds were defined as clinics, and those with twenty or more beds were defined as hospitals.
Statistical analysesThe percentages of individuals at each value of the categorical variables were compared using the χ2 test and Fisher’s exact probability test. Trends from one survey period to another were compared using the Cochran-Armitage trend test. The median and interquartile ranges of total healthcare costs per month were computed for different groups of patients in the study. Continuous variables were compared between groups using the Mann-Whitney U-test. Univariate logistic regression models of ICS non-prescription were estimated to identify significant predictors; the explanatory variables included patient demographics and asthma treatment drugs. Using multiple logistic regression analysis, risk adjustment was conducted for the factors with strong associations. The software program Stat Flex version 6 (Artech Co. Ltd., Osaka, Japan) was used for all statistical analyses, except for the Cochran–Armitage trend test, which was performed using the R 3.5.3 software program (R Foundation for Statistical Computing, Vienna, Austria). A p value of less than 0.05 was regarded as statistically significant.
Fig. 1 shows patient disposition. In the first survey period, 11,834 individuals were identified as asthmatics. Of these, 6,619 patients were identified as elderly asthmatics. The number of elderly asthmatics was 5,619 in the second survey period and 6,880 in the third survey period.
Detailed data on the total population and elderly population in Oita Prefecture are presented in Table 1. In brief, the total population was declining, while the elderly population was increasing. The percentage of the population that was elderly increased over time in both urban and rural areas. Accordingly, the number of NHI subscribers ≥ aged 65 years or older increased across the three periods. The enrollment rates of elderly individuals were high, at 89.3%, 87.1%, and 85.7% in the first, second, and third survey periods, respectively.
Table 2 shows the characteristics of the elderly asthma patients identified. When the patients were divided by age groups of five-year increments, the histogram formed a curve with a single peak, with those 75-79 years old as the largest group. The proportion of females increased over time. The proportion of patients who lived in rural areas decreased significantly (63.9%, 60.6% and 56.6%, in the first, second and third survey periods, respectively, p < 0.01). Furthermore, the proportion of patients who received prescriptions at rural medical institutions declined significantly (60.7%, 57.2% and 51.3%, in the first, second and third survey periods, respectively, p < 0.01). Patients who received cross-boundary treatment accounted for around 13% of the total, and this proportion did not change significantly across the three periods. In the first survey period, 58.6% of patients were prescribed medications at clinics, and this proportion increased significantly, rising to 60.6% in the second survey period and then 63.2% in the third period (p < 0.01). The proportion of patients admitted to a hospital declined significantly from 3.7% in the first survey period to 3.2% in the second survey period and 2.5% in the third survey period (p < 0.01).

Patient disposition. Abbreviations: NHI, National Health Insurance.

Changes in the total population, the population over 65 years, and the number of National Health Insurance subscribers in Oita Prefecture.
‡: Significant increase by the Cochran-Armitage trend test (p < 0.01).
§: Significant decrease by the Cochran-Armitage trend test (p < 0.01).

Background of the extracted elderly asthmatic patients within three months separated by three years.
‡: Significant increase by the Cochran-Armitage trend test (p < 0.01).
§: Significant decrease by the Cochran-Armitage trend test (p < 0.01).
Table 3 shows the prescription rates of asthma drugs. The prescription rates of ICS-containing regimens increased significantly (52.8%, 65.5% and 68.8%, in the first, second and third survey periods, respectively, p < 0.01). When we analyzed these changes separately, the difference between the prescription rate of ICS/LABA in the second survey period (50.6%) and the third survey period (57.0%) was statistically significant (p < 0.0001), whereas the prescription rate for ICS alone declined significantly from 16.5% to 12.3% (p < 0.0001). The prescription rates of ICS-containing regimens both in clinics and in hospitals increased significantly (p < 0.01). However, the prescription rates in clinics were significantly lower than those in hospitals during the first (48.2% vs. 59.3%, p < 0.0001), second (61.4% vs. 71.9%, p < 0.0001), and third (65.6% vs. 74.3%, p < 0.0001) survey periods. Throughout the three survey periods, the prescription rates of theophylline and beta-2 agonists declined, but the prescription rate of LTRAs exhibited a statistically significant increase (p < 0.01). Omalizumab was prescribed at a low rate of 0.1%, which did not change over the three periods.
Fig. 2 shows the prescription rates of asthma medications for all asthmatics extracted from the claims database separately for every 5 years of age. When we compared the ICS prescription rates between those aged 65 or older and those aged 20 to 64 years, the rate was significantly lower for older adults than for younger adults in the first (52.8% vs. 60.5%, p < 0.0001), second (65.5% vs. 72.0%, p < 0.0001), and third (68.8% vs. 72.4%, p = 0.0008) survey periods. Subsequently, we focused our study on individuals aged 65 years or older. Fig. 3 shows the prescription rates of the different types of drugs by age group among elderly asthmatics. Although the prescription rates of ICS and ICS/LABA increased across the three periods, they decreased significantly with advancing age within each survey period. In contrast, the prescription rates of theophylline and beta-2 agonists significantly increased with advancing age (p < 0.01). The theophylline prescription rate tended to decrease across the three periods in all age groups. The LTRA prescription rate increased significantly with advancing age only in the third survey period (p < 0.01).

Prescription of asthma medicine.
ICS, inhaled corticosteroid; LABA, long-acting beta-2 agonist; LTRA, leukotriene receptor antagonist; N.A., not available.
*p < 0.001, in comparison to the second survey period by the chi-square test.
**p < 0.001, in comparison between clinics and hospitals by the chi-square test.
‡: Significant increase by the Cochran-Armitage trend test (p < 0.01).
§: Significant decrease by the Cochran-Armitage trend test (p < 0.01).

Changes in the prescription rates of asthma medication by age for all asthmatics extracted every three years.
First survey period (■), Second survey period (▲) and Third survey period (○).
ICS, inhaled corticosteroid; LABA, long-acting beta-2 agonist; LTRA, leukotriene receptor antagonist.

Trends in the prescription rates of asthma medication by age among elderly asthmatics.
First survey period (■), Second survey period (▲) and Third survey period (○).
ICS, inhaled corticosteroid; LABA, long-acting beta-2 agonist; LTRA, leukotriene receptor antagonist.
†: Significant increase by the Cochran-Armitage trend test in all survey periods (p < 0.01).
‡: Significant increase by the Cochran-Armitage trend test in the third survey period (p < 0.05).
§: Significant decrease by the Cochran-Armitage trend test in all survey periods (p < 0.01).
As shown in Table 4, the prescription rates of ICS-containing regimens were significantly lower at medical institutions located in rural areas than those in urban areas (49.1% vs. 58.4%, p < 0.0001, 63.2% vs. 69.2%, p < 0.0001, and 66.4% vs. 71.5%, p < 0.0001, in the first, second, and third survey periods, respectively). The theophylline prescription rate was significantly higher at rural medical institutions than at urban medical institutions (48.8% vs. 38.8%, p < 0.0001) in the first survey period, but it showed no significant differences between institutions in the second survey and third survey periods. The beta-2 agonist prescription rate was significantly higher at rural medical institutions than at urban medical institutions during all three survey periods. Compared with the urban areas, the rural areas had significantly lower prescription rates of LTRAs in the third survey period and of omalizumab in the first survey period. The hospital admission rates in the rural areas were significantly higher than those in the urban areas in all three survey periods (4.5% vs. 2.3%, p < 0.0001, 4.3% vs. 1.5%, p < 0.0001, and 3.5% vs. 1.2%, p < 0.0001, in the first, second, and third survey periods, respectively). The rates of the prescription at clinics in urban areas were significantly higher than those in rural areas in all three survey periods (66.8% vs. 53.7%, p < 0.0001, 70.7% vs. 54.2%, p < 0.0001, and 73.1% vs. 56.5%, p < 0.0001, in the first, second, and third survey periods, respectively).

Comparison between urban and rural areas in the prescription rate of asthma medicine, the hospital admission rate within the survey periods separated by three years.
ICS, inhaled corticosteroid; LABA, long-acting beta-2 agonist; LTRA, leukotriene receptor antagonist; N.A., not available.
*p < 0.05, **p < 0.001, ***p < 0.0001, compared between urban area and rural area by the chi-square test.
†p < 0.05, calculated using Fisher’s exact probability test.
Fig. 4 shows the association between the prescription of asthma drugs and total monthly healthcare costs. In the first survey period, the median total medical cost was significantly lower for patients prescribed the ICS-containing regimens than for patients who were not prescribed them (median, $120.50; range, $52.46-$254.69 vs. median, $156.45; range, $75.11-$349.05, p < 0.00001); similar trends were observed in the second and third survey periods. The total medical costs declined across the three periods for both patients prescribed ICS-containing regimens and those not prescribed ICS. In contrast, the total medical costs were significantly higher among patients prescribed theophylline, beta-2 agonists, or LTRAs than in patients who were not prescribed those medications. This finding was reproduced in all three survey periods.

The association between anti-asthma drug prescription and total medical expenses per month. A box is drawn around the interquartile range, and the midline of the box represents the median; the 2.5th to 97.5th percentile range is indicated by lines. Medical costs were converted from Japanese Yen to US dollars as a fixed rate of 110 JPY/USD.
ICS, inhaled corticosteroid; LABA, long-acting beta-2 agonist; LTRA, leukotriene receptor antagonist; USD, United States dollar.
*: Medical expenses are higher than no drug prescription (p < 0.01).
**: Medical expenses are higher than no drug prescription (p < 0.001).
***: Medical expenses are higher than no drug prescription (p < 0.00001).
†: Medical expenses are lower than no drug prescription (p < 0.00001).
Considering an ICS-containing regimen as the standard treatment, we used the health insurance claims data from the third survey period to investigate the factors contributing to the non-prescription of ICS (Table 5). In the univariate logistic regression analyses, age, rural residence, receiving prescriptions at medical institutions in rural areas, receiving prescriptions from clinics, hospital admission, and prescription of theophylline, beta-2 agonists, or LTRAs were identified as factors associated with ICS non-prescription. There were no marked differences in the prescription of ICS between male and female. Next, we estimated a multivariate logistic regression model using as predictors the factors identified as significant by the univariate analysis. A five-year increase in age, living in a rural area, receiving a prescription from a clinic, being admitted to a hospital, and receiving theophylline, beta-2 agonist, or LTRA prescription were significant predictors for ICS non-prescription. In contrast, cross-boundary treatment was a factor that reduced the likelihood of ICS non-prescription. All of these findings were reproduced in the investigations of the first and second survey periods.
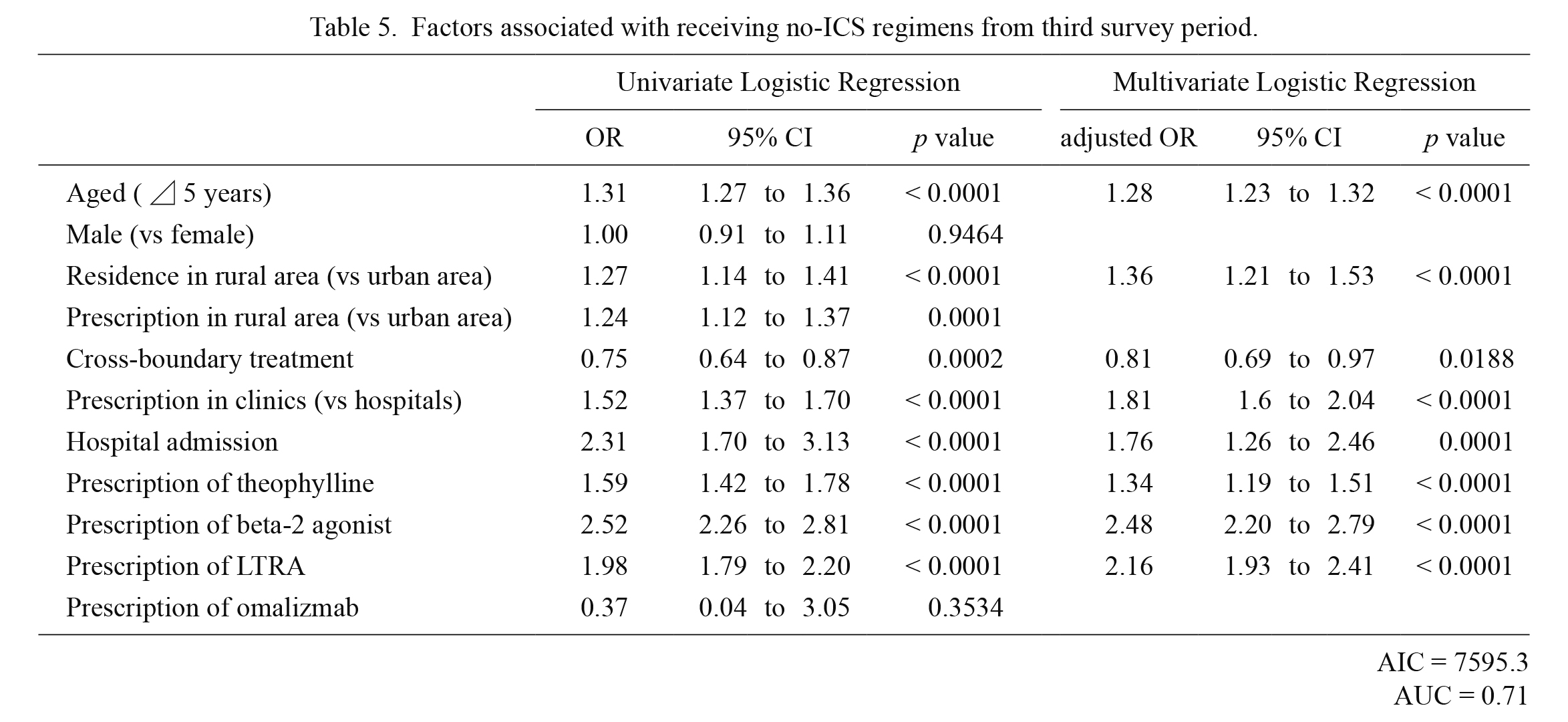
Factors associated with receiving no-ICS regimens from third survey period.
ICS, inhaled corticosteroid; LTRA, leukotriene receptor antagonist; OR, odds ratio; CI, confidence interval; AIC, Akaike’s information criterion; AUC, area under the curve.
We analyzed data from the NHI, which covers approximately 90% of the population aged 65 or older in the study area. This is the first study to clarify the treatment status of elderly asthmatics in the real world. The ICS prescription rate among elderly asthmatics increased across the three periods while the hospital admission rates declined. The monthly healthcare costs were significantly lower for patients who received ICS-containing regimens than for those who did not, while the prescription of theophylline, beta-2 agonists, or LTRAs was associated with increased healthcare costs. We identified increasing age, rural residence, receiving a prescription from a clinic, hospital admission, and prescription of asthma medications other than ICS as factors being associated with non-prescription of ICS; cross-boundary treatment increased the ICS-prescription rate.
An ICS-based regimen is the standard treatment for asthma, and this remains true for elderly asthmatics (Tsai et al. 2012; Ichinose et al. 2017; Global Initiative for Asthma 2019). However, ICS prescription rates among all age groups vary considerably across countries, from 25.4% in South Korea (Choi et al. 2018) to 60.9% in Australia (Reddel et al. 2017), 76.6% in Canada (To et al. 2015), and 80.0% in the United Kingdom (Bloom et al. 2019). In Japan, the rate is 69% according to an analysis of the Japan Medical Data Center (JMDC) Claim Database, which contain the health insurance records of office workers and their families (Atsuta et al. 2018). In this study, the prescription rate of ICS among elderly asthmatics increased over time, reaching 68.8% in the third survey period, which was consistent with the report on Japan using JMDC data (Atsuta et al. 2018). However, when compared with younger adults, elderly asthmatics received ICS prescriptions less frequently and the prescription rates decreased with advancing age. This implies that clinicians may be hesitant to prescribe inhaled medications to older patients due to potential problems, including decreased pulmonary function, irreversible airway obstruction, incorrect inhalation techniques, and poor inhalation adherence (Kim et al. 2009; Gibson et al. 2010; Jones et al. 2011; Koya et al. 2018). In addition, age-related conditions, such as cognitive decline, numerous comorbidities, and polypharmacy, contribute to the difficulty in managing asthma in older patients (Hanania et al. 2011; Tsai et al. 2012).
This survey showed low ICS prescription rates in clinics. It also revealed that a relatively high proportion of elderly asthmatics were treated in hospitals. This differed from findings in Western countries and South Korea, where most asthmatics are treated in clinics (Levy et al. 2004; Kim et al. 2013). Across the three periods, the percentage of patients prescribed medications in clinics was increasing, while the ICS prescription rates in clinics remained lower than those in hospitals. These results suggest that improvement in patient care can be made by clarifying the guidelines for clinic doctors and promoting the use of ICS.
Our findings indicate geographic differences in the treatment of elderly asthmatics. Oita Prefecture faces problems associated with a declining population that are common to all rural prefectures in Japan, where an uneven distribution of doctors serves an increasing number of people who are 65 or older. Our data showed the ICS prescription rate was markedly lower in rural areas than in urban areas; beta-2 agonists were more likely to be prescribed in these rural areas. These observations support the findings of previous studies indicating that the treatment status and risk of death in asthmatics depend on the area of residence (Baird and Wright 2006 ; Pritpal et al. 2011; Eftekhari et al. 2016). Interestingly, cross-boundary treatment increased ICS prescription rates, suggesting that cross-boundary treatment may enable elderly asthmatics to access specialist healthcare and receive the standard treatment for asthma.
This study showed that the hospital admission rates decreased across the three periods. In rural areas where ICS prescription rates were low, the hospital admission rates were high. A multivariate analysis showed that hospital admission was a factor associated with ICS non-prescription. Collectively, our data indicate that the widespread use of ICS may have directly or indirectly reduced hospital admission rates among elderly asthmatics, confirming previous findings that ICS therapy reduces the risk of hospitalization (Sin and Tu 2001; Tsai et al. 2012).
This study revealed that the widespread use of ICS/LABA contributed significantly to the increase in the ICS prescription rate. In general, the ICS/LABA combination is more effective than similar or higher doses of ICS alone (Ismaila et al. 2014). The Global Initiative for Asthma (GINA) guidelines recommend low-dose ICS for mild asthma and the addition of LABA if the asthma is not well-controlled (Global Initiative for Asthma 2019). Aside from whether it has a positive impact for elderly asthmatics, even patients with mild asthma are being treated with ICS/LABA rather than ICS alone.
Asthma is more costly to treat in older adults than in younger adults, because older adults have higher rates of hospital admission, longer hospital stays, more emergency department visits, and more prescribed medications (Banerji et al. 2006; Tsai et al. 2012; Altawalbeh, et al. 2018). We showed that prescriptions of ICS-containing regimens, including combination formulations, decreased the total healthcare costs in elderly asthmatics; in contrast, the opposite results were obtained with theophylline, beta-2 agonists, and LTRAs. Medical costs are an important issue to consider when providing continued asthma treatment (Laba et al. 2019). Our results may imply that medications used in the maintenance and prevention of asthma are costly, but asthma exacerbation events, such as hospitalizations and emergency department visits, are more costly. To our knowledge, this study is the first to reveal an association between asthma medications and healthcare costs in elderly asthmatics within a clinical setting.
Our study found that LTRAs were given to approximately half of the elderly asthmatics in the sample, and the prescription rate tended to increase over time. Furthermore, unlike ICS, the rate remained constant regardless of advancing age. These results are consistent with the finding that LTRAs are well-tolerated by elderly people (Sánchez and Buitrago 2018) and have comparable effects to ICS as a first-line controller therapy in terms of the asthma-related quality of life scores and exacerbation rates in the primary care setting (Price et al. 2011).
In our survey, theophylline was a factor affecting ICS non-prescription and the prescription rate of the drug increased with advancing age, indicating that theophylline is used as an alternative medication to ICS. Given that theophylline is considered a second-line asthma drug (Ichinose et al. 2017) and often causes side effects in older people (Barnes 2003), the decrease in theophylline prescriptions over time in this study can be considered favorable.
Several limitations associated with the present study warrant mention. First, the survey period was short. We requested one full year of data from all municipalities, but they allowed us only three months of data in order to protect personal information. Despite dissatisfaction with the study period, this approach appears worthwhile for analyzing most elderly asthmatics in the municipalities we studied. Second, the three months interval of the survey periods meant that asthma patients who were not visiting medical institutions or being prescribed asthma medication during that time period were omitted from the dataset; however, the aim of this study was not to estimate the prevalence of asthma. Third, we defined asthma based on a combination of the ICD-10 code and whether the patient had been prescribed an asthma drug at least once during the survey period. This method has been adopted in a number of other studies (Kim et al. 2013; Choi et al. 2018). Nagase et al. (2020) included patients who had been prescribed asthma medication multiple times within a one-year survey period. This approach may lead to a more stringent diagnosis of asthma, while a short-term survey such as the present study may exclude patients with long-term prescriptions (Nagase et al. 2020). Fourth, we showed that the prescription rate of ICS was lower for older adults than for younger adults. However, because the NHI coverage is only around 30% among younger adults, the NHI data may not be representative for this age group as a whole. Fifth, distinguishing whether the patients actually have asthma or chronic obstructive pulmonary disease is not straightforward. We cannot conclusively determine whether the individuals included in this study as asthma patients actually had COPD; this is not an issue associated with the claims database analysis but rather a limitation of diagnosing elderly asthma in the real world. Finally, because this was a cross-sectional study, we were unable to follow the same patients over time or to investigate long-term outcomes.
Our results indicate that there is still room for improvement to ensure that the standard guideline-recommended treatment is universally provided. Nationwide studies with longer survey periods should be conducted in the future.
We thank the Oita National Health Insurance Organization (https://oita-kokuhoren.or.jp/) and each municipality for providing us with the data from the health insurance claims. We would like to thank Editage (https://www.editage.com) for English language editing.
E.M. designed the study. T.I. and E.M. performed the analysis and wrote the manuscript. S.S., K.Y. and K.A. contributed to the critical revision of the manuscript. All authors read and approved the final manuscript.
The authors declare no conflict of interest.