2020 Volume 251 Issue 3 Pages 193-206
2020 Volume 251 Issue 3 Pages 193-206
Approximately 90% of low back pain (LBP) diagnoses are non-specific (NSLBP; i.e. with unknown cause). In NSLBP patients, the hamstrings, iliopsoas, piriformis, and tensor fasciae latae are overactive due to weak hip abductor, extensor, and core muscles. Core stability is essential for proper load balance within the pelvis, spine, and kinetic chain, and core stability exercise (CSE) is an exercise treatment regimen for LBP conditions. We investigated how core stability and hip muscle stretching exercises affected NSLBP patients’ physical function and activity. Patients were randomly allocated to three groups. The Stretch group (n = 24) performed exercises for hip muscle stretching for maximal motion; the Strengthen group (n = 22) performed exercises for hip muscle strengthening while maintaining the maximal isometric contraction. The Sham group (n = 20) received gentle palpation of the skin. Therapy was conducted thrice weekly for 6 weeks. Pain intensity, lower back instability, and hip muscle flexibility were measured to assess physical function. Disability level, balance ability, and quality of life were measured to assess physical activity. Data were collected prior to intervention and at 6-week follow-up. There were significant within-group changes for all measurements (P < 0.05). The Stretch and Strengthen groups had greater improvements in pain intensity, disability level, balance ability, and quality of life than the Sham group. Lower back instability and hip muscle flexibility had the greatest improvement in the Stretch group. In conclusion, CSE and hip muscle stretching are effective at improving physical function and activity in NSLBP patients.
Low back pain (LBP) is experienced by 80% of the population at least once during their lifetime (O’Sullivan 2000). Approximately 10% of LBP patients present specific LBP with etiologies such as lumbar spinal stenosis, spondylolisthesis, fracture of spine, inflammatory disease, or nerve root compression (Deyo et al. 1992). Meanwhile, 90% of LBP patients are diagnosed with non-specific LBP (NSLBP), in which the cause cannot be clinically identified (Koes et al. 2006).
Core stability exercise (CSE) is emphasized as a universal physiotherapy method for NSLBP (Liddle et al. 2004). CSE trains muscle activity patterns without unnecessarily overloading the tissue, and can help to stabilize the spine (Kavcic et al. 2004). Additional physiotherapy for NSLBP patients aims to treat the hip joint, especially for those patients with accompanying hip joint pain (Ben-Galim et al. 2007). The concept of hip-spine syndrome was introduced by Offierski and MacNab (1983) 30 years ago, and is frequently cited in the literature. This model assumes that there is a clear disability in two areas – the hip joint (usually hip joint arthritis) and the lower back (generally stenosis). The model hypothesizes that treatment of one area can improve pain and function in the untreated area. Although the hip joint and lower back have different functions, they actually perform a single action (Arokoski et al. 2004). Due to this relationship, musculoskeletal symptoms can be directly and indirectly affected by disability in adjacent joints (Sueki et al. 2013). Elderly patients with chronic LBP often present with hip joint pain and morning stiffness (Hicks et al. 2018), and athletes with LBP show restricted hip joint motion (Yang et al. 2018). LBP patients with hip joint osteoarthritis have reported reduced pain and improved function of the hip joint and lower back after total hip replacement surgery (Ben-Galim et al. 2007). Thus, previous studies have demonstrated an association between LBP and the hip joint.
There have been several studies comparing hip muscle strength between NSLBP patients and healthy adults. Studies have reported LBP patients show significantly lower hip abductor and extensor strength compared to healthy adults (Nourbakhsh and Arab 2002), and show weakening of the hip abductor (Tsai et al. 2010; Cooper et al. 2016), or weakening of the hip extensor (Cai and Kong 2015). Therefore, there is evidence that LBP patients experience more weakening of the hip muscles compared to healthy adults. There have been several studies that have implemented exercises for hip strengthening for LBP patients experiencing hip muscle weakness. Studies have shown that exercises for core stability and hip strengthening and motion can reduce LBP and improve LBP disability, lower back muscle strength, and balance ability; patient satisfaction has also been shown to improve when combining lumbar spine therapy and hip strengthening and joint mobility therapy (Jeong et al. 2015; Kendall et al. 2015; Bade et al. 2017). Recently, Bernet et al. (2018) reported a systematic review and meta-analysis on the effects of hip muscle intervention in LBP patients; however, the majority of studies reported hip muscle intervention as therapy for hip joint mobility and exercises to strengthen the muscles around the hip, whereas the effects of stretching the hip muscle on LBP and disability were not considered. Stretching is used prophylactically in healthy individuals or in cases of disability to prevent injury, and is often thought to improve performance (Behm et al. 2016). Health care professionals often use stretching as a means of increasing joint motion in the care for LBP patients (Han et al. 2016).
In order to maintain lumbar spine and pelvis stability, the stability of the sacroiliac joint is important, via activation of the multifidus, transversus abdominis, internal oblique, and gluteus maximus muscles (Hungerford et al. 2003). However, LBP patients experience a weakening of these muscles, leading to impaired stability of the sacroiliac joint (Nourbakhsh and Arab 2002; Hungerford et al. 2003). Hamstring activation is used to compensate for this disability, but this instigates a worsening cycle of LBP, where hamstring activation further delays activation of the multifidus, transversus abdominis, internal oblique, and gluteus maximus muscles (Hungerford et al. 2003; MassoudArab et al. 2011). Han et al. (2016) implemented CSE and hamstring stretching exercises for LBP patients and reported reduced pain and improved work ability. Fasuyi et al. (2017) reported that LBP patients show hamstring shortening, and that increasing the flexibility of the hamstrings reduces the extent of pelvic tilt. Pelvic tilt in LBP patients is also affected by the iliopsoas muscle (Lee et al. 2018b). Imamura et al. (2016) reported that the extent of LBP and disability are associated with the iliopsoas muscle, while Malai et al. (2015) reported that, in LBP patients with lumbar hyper lordosis, iliopsoas muscle stretching exercises resulted in decreased pain and lumbar lordosis angle, and increased transversus abdominis activation and flexibility of iliopsoas muscle. Kasunich (2003) proposed tensor fasciae latae tightness as a cause of LBP, and Bae et al. (2017) reported that tensor fasciae latae stretching exercises improves hip joint and pelvis motion, and helps to reduce LBP and disability. The piriformis muscle is a hip rotator, and the presence of LBP increases the size of the piriformis muscle (Leung et al. 2015), while LBP patients show restriction in hip joint rotation motion (Yang et al. 2018).
In summary, the causes of NSLBP include weakening of the hip abductor and extensor, and core muscles. The hamstring, iliopsoas, tensor fasciae latae, and piriformis muscles may be over-activated to compensate for weakening of the hip and core muscles. Many previous studies have demonstrated the effectiveness of CSE and hip muscle interventions in NSLBP patients. However, hip muscle intervention has only been implemented for the individual hip muscle, and there is little known about utilizing interventions for the overall hip musculature. The purpose of the present study was to examine the effects of CSE and hip muscle stretching exercises on physical function (i.e., pain, instability, hip muscle flexibility) of patients with NSLBP and on activity (i.e. disability, balance, quality of life [QOL]), and to investigate differences between hip muscle stretching and strengthening exercises.
This study was conducted at the Design Hospital in Jeonju, Jeollabuk-do between June and November 2019. The participants were patients diagnosed with NSLBP and were prescribed exercise therapy by an orthopedist. These patients had complaints of NSLBP for at least 3 months (Balthazard et al. 2012), and experienced a pain intensity of 3 or higher based on the visual analogue scale (VAS, 0-10 scale) (Seong et al. 2011). A total of 66 patients (34 men, 32 women) between the ages of 30-65 were ultimately included in the analysis.
The required sample size was calculated using G*power 3.1 (G-Power software 3.1.2; Franz Faul, University of Kiel, Kiel, Germany). The analysis of covariance was set at significance level (α) = 0.05, large effect size f = 0.4, and power = 0.8; this required a sample size of 64 patients to maintain an actual power of 0.80. To account for patients that would discontinue treatment (dropouts), we estimated that a total of 75 patients would be required.
The exclusion criteria adapted from a prior study (Krekoukias et al. 2017) included: (1) history of spinal surgery, (2) history of ankylosing spondylitis or rheumatoid arthritis, (3) history of spondylolisthesis or spondylolysis, (4) history of spinal or pelvic fracture, (5) history of spinal inflammation or tumor, (6) history of osteoporosis, (7) continuous use of pain medications, (8) history of stroke, (9) history of respiratory disease or heart disease, or (10) pregnancy. The withdrawal criteria were as follows: (1) lack of compliance (< 90% of sessions), or (2) participants did not want to complete the study.
The research team provided participants with detailed information about the research procedure and the safety of related experiments and treatment method, and obtained voluntary written consent from all participants. This study was approved by the Sahmyook University Institutional Review Board (IRB No. 2-7001793-AB-N-012019047HR), located in Seoul, South Korea. The research protocol was registered at http://clinicaltrials.gov (CRIS identifier KCT0004140).
ProcedureThe participants consisted of 75 NSLBP patients who had received a thorough explanation of the study requirements and voluntarily consented to participation. These participants were randomly divided into a Stretch group (n = 25) and Strengthen group (n = 25), and underwent CSE (30 min) and exercises for hip muscle stretching (15 min) or strengthening (15 min), respectively. The Sham group (n = 25) underwent CSE (30 min) and a sham treatment that entailed gentle palpation of the skin (15 min). Graphpad software was used for the randomization process (http://www.graphpad.com/quickcalcs/randomize1/). All NSLBP patients agreed to the group allocations. The NSLBP patients were blinded to which exercise group they were in until the end of the research. The procedure was performed by a principal investigator who was not involved with patient intervention and measurement. The randomization timetable was known only to the intervention administrators who treated the patients. The examiner assessing patients before intervention and after 6 weeks of intervention was also blinded to group allocation, and the patients were asked not to disclose this to the examiner.
The research team consisted of one principal investigator, one examiner, and six intervention administrators. The principal investigator checked whether participants were suitable for the study, and explained the study procedure and objectives. The examiner was blinded to group allocation and assessed the patients before intervention and after 6 weeks. Each group had two intervention administrators that were responsible for administering intervention only to the patients included within the group. Only the principal investigator had knowledge of the entire research flow, and the whole study was discussed with orthopedists and the chief of the rehabilitation center.
Outcomes were examined before the intervention and after 6 weeks; outcomes included: pain intensity, lower back instability, hip muscle flexibility (which included hamstring, iliopsoas, tensor fasciae latae, and piriformis muscles for this study), disability level, balance ability, and QOL.
Of the 75 participants, there were 9 dropouts in total, with 1 dropout from the Stretch group (unable to contact), 3 dropouts from Strengthen group (unable to contact), and 5 dropouts from the Sham group (unable to contact 4 and 1 had surgery). Thus, the main outcomes were investigated in 66 patients (Fig. 1). Table 1 summarizes the patients’ general characteristics.

Study flow diagram.
Stretch group: did exercises for core stability and hip muscle stretching, Strengthen group: did exercises for core stability and hip muscle strengthening, Sham group: did core stability exercises and received sham treatment (gentle palpation of the skin).

General characteristics of participants (n = 66).
SD, standard deviation; Stretch group, did exercises for core stability and hip muscle stretching; Strengthen group, did exercises for core stability and hip muscle strengthening; Sham group, did core stability exercises and had sham treatment; BMI, body mass index; R, right; L, left; VAS, visual analogue scale; PSLRT, passive straight leg raising test; TTT, toe-touch test; MTT, modified Thomas test; OT, Ober test; FAIRT, Flexion adduction internal rotation test; ODI, Oswestry disability index; RMDQ, Roland Morris disability questionnaires; OLST, one-leg standing test; SF-PCS, short form-physical component score; SF-MCS, short form-mental component score.
a) one-way ANOVA; b) covariate.
Measurement of pain intensity: The patients were instructed to indicate the subjective extent of their LBP along a 10-cm straight line, with tick marks. An overall score between 0 and 10 points was given, with ‘no pain’ defined as 0 points and ‘the most severe pain possible’ defined as 10 points. The VAS is an instrument with a very high test-retest reliability (intraclass correlation coefficient [ICC] = 0.99) and inter-rater reliability (ICC = 1.00) (Wagner et al. 2007).
Measurement of lower back instability: The passive straight leg raising test (PSLRT) was used to assess instability in the lower back. With the patient in a supine position, the examiner held the patient’s ankle and, with the knee extended, slowly moved the hip joint into maximal flexion, and then measured the angle of the hip using a digital inclinometer. The PSLRT is an instrument with high inter-rater reliability (ICC = 0.87-0.96) (Waddell et al. 1992).
Measurement of hip muscle flexibility: The toe-touch test (TTT) was used to measure hamstring muscle flexibility. The patient stood facing forward with both feet together. The patient then bent forward from the hip to touch their toes with their hands. Patients were asked to bend over as far as possible without bending their knees. The TTT is an instrument with high test-retest reproducibility (ICC = 0.89) (Ayala et al. 2012).
The modified Thomas test (MTT) was used to measure iliopsoas muscle flexibility. The patient sat on the edge of a table and lay down on their back. The patient pulled their knees towards their chest while keeping their lower back pressed against the table (to prevent compensation of motion by lower back extension). One foot was slowly lowered below the table. The examiner observed and felt the thigh to ensure that it was completely relaxed. In this state, a digital inclinometer was placed at the center of the lateral aspect of the thigh, and the motion of hip extension was measured. The MTT is an instrument with high inter-rater reliability (ICC = 0.89-0.92) (Clapis et al. 2008).
The Ober test (OT) was used to measure tensor fasciae latae muscle flexibility. The patient lay on their side with the leg that needed to be measured on top. To stabilize their posture, the patient flexed the hip and knee joints of the bottom leg. The examiner fixed the pelvis with one hand and, with the knee of the top leg in 90º flexion, moved the top leg through passive abduction and extension. From this position, the top leg was slowly lowered, and the motion was measured at the stopping point. The OT is an instrument with high inter-rater reliability (ICC = 0.90) (Reese and Bandy 2003).
The flexion adduction internal rotation test (FAIRT) was used to measure piriformis muscle flexibility. With the patient in a supine position, the hip joint in 60º flexion, and the knee joint in 90º flexion, the examiner moved the hip through passive adduction and internal rotation. The motion was measured using a goniometer at the point in the passive test where the patient experienced pain in the sciatic/gluteal area (Kean Chen and Nizar 2013).
Measurement of disability level: The Oswestry disability index (ODI) was used to assess the extent of disability caused by LBP. The ODI consisted of 10 questions on pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sexual activity, social life, and travel. Performance in each item was described in 6 stages, from 0 to 5 points (Fairbank 2014). A higher score on the ODI indicated more severe disability.
The Roland Morris disability questionnaire (RMDQ) was developed to assess physical function in relation to LBP. The RMDQ consists of 24 items, including walking, sitting, lying, dressing, sleeping, self-care, and daily living, and the range for the total score is 0-24 points. A higher score on the RMDQ indicates a more severe disability level (Roland and Morris 1983).
Measurement of balance ability: The one-leg standing test (OLST) was used to measure the static balance ability of the LBP patients. At the start of the OLST, the patient stood on two feet on firm, even ground, with their eyes closed and their arms spread. Upon the instruction, “Start,” the patient raised one leg 90º and the timer was started simultaneously. The time was measured until the foot touched the ground again. The OLST is an instrument with high inter-rater reliability (ICC = 0.88-1.0) (Tidstrand and Horneij 2009).
Measurement of QOL: The SF-36 is a short-form survey developed by Ware and Sherbourne (1992), and it was used to assess QOL for patients with LBP. This self-report questionnaire consisted of 36 questions in total, divided into 8 subdomains: physical function, physical role difficulty, pain, general health, energy, social function, emotional role difficulty, and mental health. Each item was scored, and each subdomain was converted to a score in the range of 0-100 points. A higher score indicated a higher health-related QOL.
InterventionCore stability exercise: All groups participated in CSE for 30 min, 3 times/week, for 6 weeks. For each exercise, isometric contraction was maintained for 7-8 s. Each exercise was reported 10 times, and there was a brief rest interval of 3 s between repetitions. Patients were provided a 1-min rest in between exercises (McGill 2015). Individual training intensity gradually increased with decreasing therapist’s assistance, and was determined based on the patient’s performance. During the repetition of each exercise, patients were instructed to contract their abdominal muscles, and to hold the contraction while maintaining a normal breathing pattern (Saleh et al. 2019). All exercise sessions were performed in individual exercise programs with the therapist, and recorded in a diary to facilitate adherence rates. Based on the exercise methods of Saleh et al. (2019), CSE consisted of abdominal hollowing, side bridge, supine extension bridge, straight leg rise from prone, alternate arm and leg raise from quadruped, and prone bridge. The methods for the CSE are described in Table 2.
Hip muscle stretching exercise: In addition to core stability exercises, Stretch group patients participated in hip muscle stretching exercises for 15 min, 3 times/week, for 6 weeks. All hip muscle stretching exercises were maintained for 30 s at the maximal motion, before returning to the original position and resting for 10 s. All exercises were repeated 3 times (Han et al. 2016). Patients were instructed to minimize tension in their body and to breath in during each movement. All exercise sessions were performed in individual exercise programs with the therapist, and recorded in a diary to facilitate adherence rates. The hip muscle stretching exercises consisted of hamstring stretch (Castellote-Caballero et al. 2014), iliopsoas stretch (Wakefield and Cottrell 2015), piriformis stretch (Gulledge et al. 2014), and tensor fasciae latae stretch (Umehara et al. 2015). The methods for the hip muscle stretching exercises are described in Table 3.
Hip muscle strengthening exercise: In addition to core stability exercises, Strengthen group patients participated in hip muscle strengthening exercises for 15 min, 3 times/week, for 6 weeks. All hip muscle strengthening exercises were maintained for 30 s at maximal isometric contraction, before returning to the original position and resting for 10 s. All exercises were repeated 3 times. Individual training intensity gradually increased with decreasing therapist’s assistance, and was determined based on the patient’s performance. All exercise sessions were performed in individual exercise programs with the therapist, and recorded in a diary to facilitate adherence rates. Hip muscle strengthening exercises consisted of side-lying hip abduction with internal rotation, prone heel squeeze (Philippon et al. 2011), quadruped hip extension (Boren et al. 2011), and standing gluteal squeeze (Contreras et al. 2015). The methods for the hip muscle strengthening exercises are described in Table 4.
Sham treatment: The Sham group participated in sham treatment for 15 min, 3 times/week, for 6 weeks. The therapist gently palpated the skin over the patient’s lumbosacral spine, and did not perform any other intervention. The patients were unaware that they were in the Sham group, and believed that they were receiving actual treatment at the time of the intervention (Krekoukias et al. 2017).
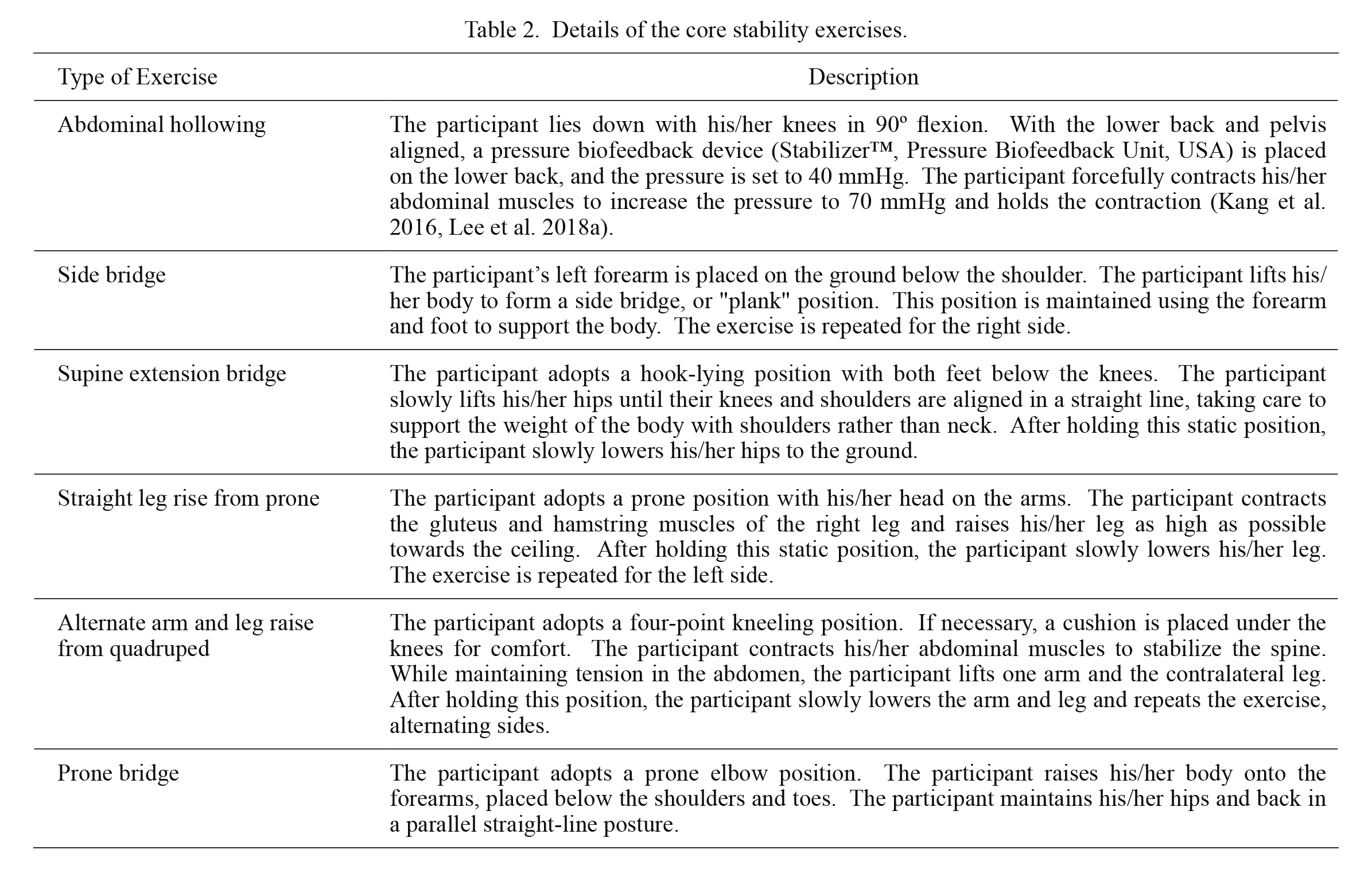
Details of the core stability exercises.
The trick movements or compensation of all exercises were focused and corrected by the chin-out position, throw-out abdominal position, or trunk hyperextension position.

Details of the hip muscle stretching exercises.
The trick movements or compensation of all exercises were focused and corrected by the chin-out position, throw-out abdominal position, or trunk hyperextension position.

Details of the hip muscle strengthening exercises.
The trick movements or compensation of all exercises were focused and corrected by the chin-out position, throw-out abdominal position, or trunk hyperextension position.
IBM SPSS Statistics version 23.0 software for Windows (IBM Corp, Armonk, New York, USA) was used for statistical processing in this study. The Shapiro-Wilk test was used for normality testing of the participants’ general characteristics. A one-way ANOVA was performed to test the homogeneity of the dependent variables between the three groups at baseline. Paired t-tests were performed to compare changes in physical function and activity within the groups between pre- and post-intervention. An analysis of covariance was performed to compare differences between groups. Bonferroni’s method was used for post-hoc testing. A statistical significance level of α = 0.05 was used for all tests.
Analysis of within-group changes showed that all groups had significant differences between pre- and post-intervention (P < 0.05) for: pain intensity, lower back instability, and hip muscle flexibility (Table 5). Additionally, there were significant differences between pre- and post-intervention for disability level, balance ability, and QOL, when changes within-group changes were analyzed (Table 6).
There were statistically significant differences in pain intensity, lower back instability, and in hip muscle flexibility between the groups (P < 0.05). Post-hoc Bonferroni testing confirmed that the Stretch group experienced a greater impact on lower back instability and hip muscle flexibility than the Strengthen and Sham groups and that both the Stretch and Strengthen groups experienced a greater impact on pain intensity than the Sham group (Table 7). There were statistically significant differences in the disability level, balance ability, and QOL between the groups (P < 0.05). Post-hoc Bonferroni testing confirmed that the Stretch and Strengthen groups experienced a greater impact on disability level, balance ability, and QOL than the Sham group (Table 8).

Comparison of baseline and 6-week exercise outcome measures of physical function within groups (n = 66).
SD, standard deviation; CI, confidence interval; Stretch group, did core stability and hip muscle stretching exercises; Strengthen group, did core stability and hip muscle strengthening exercises; Sham group, did core stability exercises and had sham treatment; VAS, visual analogue scale; PSLRT, passive straight leg raising test.
a)paired t-test; *P < 0.05.

Comparison of baseline and 6-week exercise outcome measures of physical activity within groups (n = 66).
SD, standard deviation; CI, confidence interval; Stretch group, did exercises for core stability and hip muscle stretching; Strengthen group, did exercises for core stability and hip muscle strengthening; Sham group, did core stability exercises and had sham treatment; ODI, Oswestry disability index; RMDQ, Roland Morris disability questionnaires; OLST, one-leg standing test; SF-PCS, short form-physical component score; SF-MCS, short form-mental component score.
a)paired t-test; *P < 0.05.

Change in outcome measures of physical function between groups (n = 66).
SD, standard deviation; Stretch group, did exercises for core stability and hip muscle stretching; Strengthen group, did exercises for core stability and hip muscle strengthening; Sham group, did core stability exercises and had sham treatment; VAS, visual analogue scale; PSLRT, passive straight leg raising test; FAIRT, Flexion adduction internal rotation test; A, Stretch group; B, Strengthen group; C, Sham group.
a)analysis of covariance; b)Bonferroni, *P < 0.05.

Change in outcome measures of physical activity between groups (n = 66).
SD, standard deviation; Stretch group, did exercises for core stability and hip muscle stretching; Strengthen group, did exercises for core stability and hip muscle strengthening; Sham group, did core stability exercises and had sham treatment; ODI, Oswestry disability index; RMDQ, Roland Morris disability questionnaires; OLST, one-leg standing test; SF-PCS, short form-physical component score; SF-MCS, short form-mental component score; A, Stretch group; B, Strengthen group; C, Sham group.
a)analysis of covariance; b)Bonferroni; *P < 0.05.
The overall objective of this study was (1) to determine whether hip muscle stretching intervention in conjunction with CSE would result in greater improvements in outcomes than sham treatment, and (2) to compare commonly used hip muscle strengthening exercises. We hypothesized that the addition of hip muscle stretching exercises would show improved outcomes for both physical function and activity after 6 weeks of intervention. We observed greater differences in the pain intensity, lower back instability, hip muscle flexibility, disability level, balance ability, and QOL scores after 6 weeks for the Stretch group than the Sham group. While for the Strengthen group, we observed greater differences in lower back instability and hip muscle flexibility than in the Sham group. To the best of our knowledge, this is the first randomized controlled trial to assess the effects of hip muscle stretching exercises on patients with NSLBP.
NSLBP is related to hip muscle strength and endurance (Nourbakhsh and Arab 2002), and hip muscle imbalance leads to LBP (Van Dillen et al. 2000). Hip extensor and abductor weakness have been reported to cause LBP in female athletes (Nadler et al. 2002). Thus, due to the importance of these muscles in LBP, exercises to strengthen the hip extensors and abductors have been highlighted as necessary (Bade et al. 2017).
Stretching exercises are one of the most important methods to restore and maintain normal flexibility, and are used to reduce muscle tension or pain and to increase joint motion (Schilling and Stone 2000). The hip muscle stretching exercises in this study aimed to stretch the hamstrings, iliopsoas, tensor fasciae latae, and piriformis muscles. Tension in these muscles inhibits contraction of the hip extensors and abductors in daily life activities, and can act as risk factors for LBP (Frank et al. 2009). Hamstring shortening causes LBP by increasing pelvic tilt (Fasuyi et al. 2017), while the iliopsoas affects activity of the transversus abdominis and, when shortened, causes LBP by inhibiting the transversus abdominis and hip extensor muscle activity (Malai et al. 2015). Hip extensor weakness causes tension in the piriformis, which leads to LBP and restricted hip joint rotation motion (Yang et al. 2018), while the tensor fasciae latae also restricts the motion of the hip joint and pelvis, and causes LBP (Bae et al. 2017). These findings support the need for the hip muscle stretching exercises proposed in this study.
Kim and Lee (2017) reported a significant decrease in LBP after 6 weeks of CSE using a rehabilitation concept in chronic LBP patients. Likewise, in the present study, we observed significant decreases in the pain intensity compared to baseline after 18 sessions in 6 weeks of CSE and hip muscle stretching exercises in the Stretch group (pain intensity difference 3.58 score), following CSE and hip muscle strengthening exercises in the Strengthen group (pain intensity difference 3.75 score), and for CSE only in the Sham group (pain intensity difference 2.93 score). The minimum clinically important difference (MCID) of the pain intensity (VAS) is 2.1 score (Parker et al. 2011). Based on these results, it is thought that CSE in all three groups activated abdominal and lower back muscles that had become weaker due to LBP (Selkow et al. 2017), resulting in a significant decrease in LBP in all groups. In the between-group comparison, Stretch and Strengthen groups showed significant differences compared to the Sham group. Bade et al. (2017) randomly divided 84 LBP patients into two groups: one group received pragmatic LBP intervention, including CSE, and hip joint mobility therapy and strengthening exercises, and the other group received pragmatic LBP intervention only. The authors reported a significant decrease in LBP in the group that also received hip joint mobility therapy and strengthening exercises (Bade et al. 2017). A previous report suggested that hip joint mobility therapy and strengthening exercises improved the strength of weakened muscles and relaxed tense muscles; this reduced anterior pelvic tilt, which in turn lessened the pressure on the spine and provided pain relief (Kang and Kim 2019), which supports the results of our study on hip muscle stretching and strengthening exercises.
Louw et al. (2017) reported a 5-degree improvement in PSLRT (lower back instability) in chronic LBP patients who underwent manual therapy. Likewise, in the present study, the Stretch (lower back instability difference 7.5 degrees), Strengthen (lower back instability difference 3.63 degrees), and Sham (lower back instability difference 3.3 degrees) groups all showed significant improvements in lower back instability post-intervention compared to pre-intervention. Control of rotation motion of the spine is an important variable for lower back stability. The transversus abdominis and multifidus contract synergistically to control the rotation motion of the spine, and it is thought that the CSE in this study affected this control process by activating transversus abdominis and multifidus, resulting in reduced instability of the lower back (Wilke et al. 1995). Moreover, the between-groups comparison showed a significant difference in the Stretch group compared with Strengthen and Sham groups. LBP patients generally show lower crossed syndrome, in which there is tightness of the back extensors and hip flexors and weakness of the abdominal muscles and the hip extensors (Frank et al. 2009). Hip joint motion and imbalances in muscle length and muscle strength are associated with chronic LBP (Van Dillen et al. 2000). Lower back instability is observed in 57% of chronic LBP patients (Alqarni et al. 2011). The hip muscle stretching exercises in this study are thought to have increased the length of shortened hip muscles, facilitating activation of the transversus abdominis, which plays a relatively important role in lower back stability, which resulted in greater improvements in lower back instability in the Stretch group that performed hip muscle stretching exercises.
Trampas et al. (2015) observed a significant improvement in balance ability in chronic NSLBP patients who underwent CSE and manual therapy. Park (2006) reported a 1.26 sec improvement in OLST (balance ability) in LBP patients who underwent Tai Chi exercise. Similarly, in the present study, there were significant improvements in balance ability after the intervention in both Stretch (balance ability difference 4.78 sec) and Strengthen (balance ability difference 3.99 sec) groups and in the Sham group (balance ability difference 1.27 sec). Yadav and Deshmukh (2013), reported that CSE is highly effective at improving dynamic balance in LBP patients, which is consistent with our results. Meanwhile, in the between-groups comparison, both Stretch and Strengthen groups showed significant differences compared to the Sham group. Humans use strategies involving the ankle and hip joints and foot support to maintain postural stability (Horak and Nashner 1986). Chronic LBP patients favor hip joint strategies over ankle strategies for maintaining postural stability (Nies and Sinnott 1991), and compared to younger adults, the elderly use hip joint strategies more frequently (Okada et al. 2001). In the present study, the Stretch group patients, who performed hip muscle stretching exercises, showed significant improvements in hip muscle flexibility following the intervention, and these increases in hip muscle flexibility are thought to have resulted in improved balance ability by affecting hip joint strategies. Meanwhile, the Strengthen group patients, who performed hip muscle strengthening exercises, are thought to have showed improved balance ability due to increased hip muscle strength. Jeong et al. (2015) randomly divided 40 chronic LBP patients into a group that performed CSE and hip muscle strengthening exercises, and another group that only performed CSE, and reported a significant increase in balance ability in the group that performed both CSE and hip muscle strengthening exercises, supporting our results for Strengthen group.
The Stretch (ODI difference 28.42, RMDQ difference 7.71), Strengthen (ODI difference 26.73, RMDQ difference 7.69), and Sham (ODI difference 21.5, RMDQ difference 5.58) groups all showed significant decreases in scores for disability level (ODI, RMDQ) following the intervention. The MCIDs are a score of 14.9 for ODI and a score of 5 for RMDQ (Parker et al. 2011; Yelland et al. 2011). In the between-groups comparison, Stretch and Strengthen groups showed significant differences compared to the Sham group. Saleh et al. (2019) administered CSE to lumbo-pelvic pain patients and reported a significant decrease in disability level; Bade et al. (2017) randomly divided LBP patients into a group that received pragmatic LBP intervention and hip exercises and a group that only received pragmatic LBP intervention, and reported significant decreases in disability level in the group that had also performed hip exercises. Based on these results, we may infer that repeated hip muscle stretching and strengthening resolves muscle length and muscle strength imbalances, leading to increased spine motion and reduced pain (Gawda et al. 2015), and this is thought to explain the significant improvements observed in disability level in the Stretch and Strengthen groups, who performed hip muscle stretching or strengthening exercises, compared to the Sham group.
Ulger et al. (2017) reported significant improvements in QOL (short form-physical component score [SF-PCS], short form-mental component score [SF-MCS]) after 18 sessions of CSE and manual therapy over 6 weeks in chronic LBP patients. Likewise, in the present study, the Stretch (SF-PCS difference 17.82 score, SF-MCS difference 14.45 score), Strengthen (SF-PCS difference 16.92 score, SF-MCS difference 12.87 score) groups, and Sham groups (SF-PCS difference 8.55 score, SF-MCS difference 8.03 score) showed significant improvements in QOL after the intervention. The MCIDs are a score of 8.8 for SF-PCS and 9.3 for SF-MCS (Parker et al. 2012). In the between-groups comparison, Stretch and Strengthen groups showed significant differences compared to the Sham group. These results suggest that CSE led to core muscle strengthening, improved spinal stability, and reduced stress on the spine in all participants (Çelenay and Kaya 2017), which was effective at ameliorating disability experienced in daily life activities. Moreover, patients exhibited muscle imbalance and altered movement patterns to compensate for and protect injured areas, which exacerbated pain in daily life activities (Lund et al. 1991). The hip muscle stretching and strengthening exercises in this study reduced imbalances by stretching muscles that had been shortened and strengthening muscles that had become weaker, facilitating normal movement patterns and improving QOL.
With regards to therapeutic methods for NSLBP patients, previous studies have focused on hip muscle strengthening exercises (Kendall et al. 2015; Bade et al. 2017). However, the overall results of the present study show that hip muscle stretching exercises were even more effective than hip muscle strengthening exercises at improving lower back instability and hip muscle flexibility scores. The increased hip joint motion and reduced lower back instability as a result of hip muscle stretching exercises have been associated with changes such as improved muscular performance (Ferreira et al. 2007), prevention of muscle atrophy (Coutinho et al. 2004), reduced stiffness (Marshall et al. 2011), and improved proprioception sense (Walsh 2017). In addition, reduced lower back instability may have many positive effects including on various limb movements, heavy lifting, personal care, walking, and sitting. Increased hip muscle flexibility is expected to have a positive effect on leg flexion movements, stair walking, wearing socks, and lumbar flexion which require the motion of the hip joint. It is thought that these positive changes have an effect on physical function and activity of NSLBP patients. Thus, the results of our study demonstrate the necessity of hip muscle stretching exercises.
This study had several limitations. First, the intervention period was short, and a 6-month follow-up was not possible after the experiment, limiting the ability to quantify and compare the results. Second, since objective assessments using devices such as ultrasound or electromyography were not performed, the actual changes in the muscles could not be determined. Further studies will be needed in the future to overcome these limitations.
In conclusion, this study investigated the effects on physical function and activity after intervention with hip muscle stretching exercises in combination with CSE for patients with NSLBP. Similar to hip muscle stretching exercises, CSE and hip muscle strengthening exercises improved physical function and activity. In particular, hip muscle stretching exercises improved lower back instability and hip muscle flexibility. In this study, hip muscle stretching exercises seem to be more effective for improving NSLBP than hip muscle strengthening exercises. Based on these results, we believe that hip muscle stretching exercises could be used effectively alongside CSE in a clinical setting.
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (Ministry of Education) (No. 2017R1D1A1B03035062).
The authors declare no conflict of interest.