2020 Volume 252 Issue 1 Pages 53-61
2020 Volume 252 Issue 1 Pages 53-61
The anti-DIC biological agent, recombinant human soluble thrombomodulin (rhTM), is being used clinically for DIC treatment in Japan. Patients with acute cholangitis associated with DIC are severe and require improved treatment. In addition, although clinical efficacy of rhTM in patients with acute cholangitis and DIC is expected, its efficacy is controversial. Thus, it is useful to evaluate rhTM in patients with acute cholangitis with DIC. This study aimed to validate the hypothesis that rhTM use improves in-hospital mortality in patients with acute cholangitis with DIC. A propensity score-matching analysis using a nationwide administrative database, the Japanese Diagnosis Procedure Combination Inpatient Database from April 2012 to March 2018, was performed. This database includes administrative claims data for all inpatients discharged from more than 1,000 participating hospitals, covering 92% of all tertiary-care emergency hospitals in Japan. Eligible patients (n = 2,865) were categorized into the rhTM (n = 1,636) or control groups (n = 1,229). Propensity score-matching created a matched cohort of 910 pairs with and without rhTM. In-hospital mortality between the groups in the unmatched analysis showed no significant difference (rhTM vs. control; 10.8% vs. 12.2%; p = 0.227). However, in-hospital mortality between the groups in the propensity score-matched analysis showed a significant difference (rhTM vs. control; 9.5% vs. 12.9%; p = 0.021). These results demonstrated that the rhTM group had significantly lower in-hospital mortality for patients with acute cholangitis with DIC. We propose that rhTM should be used for the treatment of patients with acute cholangitis with DIC.
Disseminated intravascular coagulation (DIC) is a systemic disease that causes both thrombosis and hemorrhage (Tagami et al. 2015c). DIC, a syndrome with a poor prognosis in severe cases, frequently complicates acute cholangitis (Nakahara et al. 2013). Acute cholangitis is an infectious disease caused mainly by a Gram-negative bacillus often associated with DIC (Morita et al. 2019). In acute cholangitis induced DIC, the treatment, including biliary drainage, can immediately resolve DIC. However, some patients still have poor outcomes, and further improvements in therapy are needed (Suetani et al. 2015).
The anti-DIC biological agent, recombinant human soluble thrombomodulin (rhTM, Asahi Kasei Pharma Corp., Tokyo, Japan), was approved in 2008 and is being used clinically for DIC treatment in Japan (Saito et al. 2007; Iba et al. 2013). Thrombomodulin is a thrombin receptor on the endothelial cell surface that plays a vital role in the regulation of intravascular coagulation (Maruyama 1999; Faust et al. 2001). rhTM is composed of the active, extracellular domain of thrombomodulin (Saito et al. 2007). Similar to membrane-bound thrombomodulin, rhTM binds to thrombin to inactivate coagulation. The thrombin-rhTM complex activates protein C to produce activated protein C, which, in the presence of protein S, inactivates factors VIIIa and Va. This activation inhibits further thrombin formation (Maruyama 1999; Saito et al. 2007). This mechanism of rhTM is expected in clinical practice, and the use of rhTM has dramatically increased in Japan (Honda et al. 2011; Murata et al. 2016).
Recently, Vincent et al. (2019) reported the results of a prospective, randomized, multinational, multicenter, placebo-controlled, phase 3 trial of rhTM in patients (n = 800) with sepsis-associated coagulopathy. As a result, the administration of rhTM did not significantly reduce mortality. Yamakawa et al. (2019) reported a systematic review and meta-analysis of rhTM therapy for sepsis-induced coagulopathy in randomized controlled trials; they observed the reduction in the risk of mortality in the rhTM group, but the difference was not significant. Also, in the previous study for the patients (n = 66) with acute cholangitis with DIC, although DIC resolution rate of rhTM group is significantly better, significantly reduced mortality was not observed (Suetani et al. 2015). Whether rhTM use in DIC treatment results in a significant reduction in mortality remains unclear. Besides, in previous studies, the insufficient sample size is considered to be the limit of research (Suetani et al. 2015; Vincent et al. 2019). Therefore, it remains controversial as to whether rhTM is effective in decreasing mortality for DIC.
As indicated above, patients with acute cholangitis associated with DIC are severe and require improved treatment. In addition, although clinical efficacy of rhTM in patients with acute cholangitis and DIC is expected, its efficacy is controversial. Thus, it is useful to evaluate rhTM in patients with acute cholangitis with DIC. We hypothesized that rhTM improves in-hospital mortality in patients of acute cholangitis with DIC. The current study aimed to validate our hypothesis using the DPC database.
This retrospective observational study used inpatient data included in the Japanese Diagnosis Procedure Combination (DPC) database (Murata et al. 2011c, 2012, 2014). The DPC database includes discharge and administrative claims data for all inpatients discharged from more than 1,000 participating hospitals, covering 92% of all tertiary-care emergency hospitals in Japan (Matsuda et al. 2012; Tagami et al. 2014, 2015b, c).
The database includes patient baseline information such as sex, age, primary diagnosis, admission-precipitating diagnosis (on Day 1), comorbidities on admission (on Day 1), and post-admission complications coded with International Classification of Diseases 10th Revision (ICD-10) codes and written in the Japanese language. The primary diagnosis is limited to one. The DPC database also includes the dosages and dates of all drugs and blood products administered each day during hospitalization. All interventional or surgical procedures utilize original Japanese codes determined by the Japanese Ministry of Health, Labor and Welfare. We recorded the dates of hospital attribution, hospital admission and discharge, surgery, bedside procedures, drugs administered, and discharge status (dead or alive) using a uniform data submission format. The responsible physicians are required to record the diagnoses regarding medical charts to optimize the accuracy of the recorded diagnoses. Also, the diagnostic records are linked to the payment system, and the attending physicians are required to report objective evidence for the diagnosis of the disease for reimbursement of treatment (Matsuda et al. 2012; Tagami et al. 2014, 2015b, c).
This study was approved by the institutional review board of The Tokyo Medical and Dental University (No. M2000-788-15), which waived the requirement for informed patient consent because of the anonymous nature of the data.
Patient selectionWe identified patients with acute cholangitis in the DPC database discharged from hospital between April 2012 and March 2018, and who also had DIC diagnosed on admission.
The inclusion criteria for the current analysis were as follows:
(ⅰ)Acute cholangitis in the primary diagnosis of hospitalization (i.e., ICD-10 coded ‘K830’ in the primary diagnosis section of the database). (ⅱ)DIC diagnosis at admission (i.e., ICD-10 coded ‘D65’ in the admission-precipitating diagnosis or ICD-10 coded ‘D65’ in the comorbidities on admission section of the database or started rhTM on Day 1 or Day 2). (ⅲ)‘Suspected cases in diagnosis’ written in the Japanese language were excluded. The exclusion criteria were as follows: (ⅰ) patients who died on Day 1 or Day 2; and (ⅱ) started rhTM after Day 3 (i.e., patients who were administered rhTM in this study were limited to the start of early phase on admission).
We defined patients who started rhTM on Day 1 or Day 2 of admission as the rhTM group. Those who did not use rhTM were defined as the control group.
OutcomesThe primary outcome was in-hospital mortality. In-hospital mortality was measured in a previous research that evaluated acute cholangitis with DPC data. This research paper was also cited in the Tokyo guidelines, which are clinical guidelines for acute cholangitis and acute cholecystitis (Murata et al. 2011b). The secondary outcome was the length of hospital stay, excluding deceased and transferred patients. The reason for the exclusion was that it would extend or shorten the length of hospital stay.
Statistical analysisWe performed propensity score matching to account for the differences in baseline characteristics, including treatments and interventions, between rhTM and control groups (Rosenbaum and Rubin 1985). The application of propensity score-matching involves estimation of the propensity score, followed by matching of patients according to the estimated propensity scores and comparison of the outcomes in the matched patients. We estimated propensity scores with logistic regression with the use of rhTM as a dependent variable. Independent variables included sex; age; hospital type (academic or non-academic) (Morita et al. 2017); emergency admission; Charlson Comorbidity Index (CCI) (Quan et al. 2005; Sundararajan et al. 2007; Murata et al. 2014; Tarasawa et al. 2018); treatment in Intensive Care Unit (ICU) or Emergency Room (ER); use of drugs for DIC (i.e., Antithrombin, Gabexate mesilate, Nafamostat mesilate, Ulinastatin) (Iba et al. 2014; Tagami et al. 2014); use of intravenous immunoglobulin (Laupland et al. 2007); use of broad-spectrum antibiotics (i.e., Carbapenem, Tazobactam/Piperacillin, New Quinolone) (Ely et al. 2018); use of catecholamines (i.e., Noradrenaline, Adrenaline, Dopamine, Dobutamine) (De Backer et al. 2010); blood transfusion (i.e., Red blood cells, Platelets) (Park et al. 2012); Mechanical ventilator (Iwagami et al. 2014); Continuous hemodiafiltration (CHDF) (Sakamaki et al. 2013); and surgery (i.e., Nasobiliary drainage, Transhepatic biliary drainage, Biliary stenting) (Suetani et al. 2015). To assess the severity of chronic comorbid conditions, we used the CCI, the most widely used index of comorbidity, which has been validated in various studies (Murata et al. 2014). The CCI was expressed as a score for comorbidities including solid malignant tumors and was evaluated as a continuous variable (Murata et al. 2014). It has been reported that patients who developed DIC in solid malignant tumors had a worse outcome than those with infection-related DIC (Tamura et al. 2015). In the current study, the presence of solid malignant tumors were assessed using the CCI. Also, in the current study, we regarded the treatments (including treatment in ICU or ER, DIC drugs use, immunoglobulin use, broad-spectrum antibiotics use, catecholamines use, blood transfusion, mechanical ventilator, CHDF, and surgery) given at the same time as rhTM as ‘pre-rhTM treatments,’ because the critically ill status requiring these treatments had already existed at admission (Tagami et al. 2015c). Therefore, data extraction of these ‘pre-rhTM’ treatment was limited to implementation on Day 1 or Day 2 after admission.
This study utilized the C-statistic to determine conformity. We performed propensity score matching between the rhTM and control groups based on the estimated propensity scores for each patient. For Propensity score-matching, we set a caliper width at 20% of the standard deviation of the propensity scores, and performed one-to-one matched analysis using nearest-neighbor matching (Griswold et al. 2010; Jo et al. 2020). This study evaluated the balance in baseline characteristics between the two groups using the standardized difference and defined significant imbalance as an absolute standardized difference of > 10% (Austin 2011). We presented descriptive statistics for all patients (unmatched) and propensity score-matched patients. Categorical variables were reported as number, percentages and compared using the Chi-squared test. Continuous variables were reported as means ± standard deviation and compared using Welch’s t-test. The primary outcome was presented for all patients (unmatched) and propensity score-matched patients and reported as number, percentages and compared using the Chi-squared test.
We added two analytical methods using propensity scores to confirm the robustness of the results. The first analytical method is an inverse probability of treatment weighting (IPTW) (Lunceford and Davidian 2004; Sato et al. 2017; Jo et al. 2020). Propensity-score stabilized IPTW employs a pseudo-population in which the treatment is independent of the measured potential confounders, meaning that the weighted treatment effect estimates will be less biased. The second analytical method is the adjustment for the propensity score as the covariate (Drake 1993; Sato et al. 2017). Two analytical methods have the advantage of estimating the clinical effect of rhTM while maintaining sample size (Sato et al. 2017). We performed a logistic regression analysis to examine the association between rhTM and in-hospital mortality on all patients (unmatched), propensity score-matched patients, all patients (IPTW), and all patients (adjustment for the propensity score as the covariate).
We presented a secondary outcome for all patients (unmatched) and propensity score-matched patients, excluding deceased and transferred patients. The secondary outcome was reported as the median, interquartile range (IQR) and compared using the Mann-Whitney U test.
All p values were two-tailed, considering p < 0.05 as statistically significant. We conducted all statistical analyses using IBM SPSS version 25.0 for Windows (IBM Corp., Armonk, NY, USA).
During the 72-month study period, 3,081 patients diagnosed with acute cholangitis with DIC were discharged. Of the patients initially identified, 2,865 eligible patients had acute cholangitis and DIC on the day of admission. These patients were categorized into rhTM (n = 1,636) or control (n = 1,229) groups, from which 910 propensity score-matched pairs were generated (Fig. 1).
Table 1 shows the baseline characteristics of the unmatched and propensity score-matched groups. The C-statistic indicated that the conformity was 0.743 in the propensity score model. A comparison of the unmatched groups determined that patients were more likely to receive rhTM if they were male, admitted to an academic hospital, were emergency hospitalizations, higher CCI, and required more treatment in ICU or ER, more medications, and more interventions. Propensity score matching resulted in well-balanced baseline characteristics between the groups (i.e., standardized differences < 10.0%).

Patients selection in this study.
We extracted a total of 3,081 patients with acute cholangitis with disseminated intravascular coagulation from the Diagnosis Procedure Combination data in Japan. Those excluded from this study were patients who died on Day 1 or Day 2 of admission (n = 133) and patients who started recombinant human soluble thrombomodulin after Day 3 of admission (n = 83). Thus, 2,865 patients were eligible for this study. After data extraction, we defined patients who started recombinant human soluble thrombomodulin on Day 1 or Day 2 of admission as the rhTM group and patients who did not use recombinant human soluble thrombomodulin as the control group. Propensity score-matching created a matched cohort of 910 pairs with and without recombinant human soluble thrombomodulin.
rhTM, recombinant human soluble thrombomodulin.

Baseline characteristics in the unmatched and propensity score-matched groups.
Values were numbers of subjects per group (n) with percentages or means ± standard deviation.
p values were derived from the Chi-squared test 1) or Welch’s t-test 2).
The C-statistic indicated 0.743 in the propensity score model.
rhTM, recombinant human soluble thrombomodulin.
Table 2 shows in-hospital mortality rates in the unmatched and propensity score-matched groups. The overall in-hospital mortality rate was 11.4% (326/2,865). No Significant difference in-hospital mortality was shown between the two groups in the unmatched analysis (rhTM vs. control; 10.8%, 176/1,636 vs. 12.2%, 150/1,229; p = 0.227). On the other hand, there was a significant difference in-hospital mortality rates between the two groups in the propensity score-matched analysis (rhTM vs. control; 9.5%, 86/910 vs. 12.9%, 117/910; p = 0.021).
Table 3 shows logistic regression analyses between the use of rhTM and in-hospital mortality. Logistic regression analyses revealed a significant association between the use of rhTM and in-hospital mortality, except for the pattern of all patients (unmatched). Odds ratio (OR) and 95% confidence interval (95% CI) were 0.867 (0.688-1.093) in pattern of all patients (unmatched), 0.707 (0.527-0.950) in pattern of propensity score-matched patients, 0.754 (0.570-0.998) in pattern of all patients (IPTW), and 0.755 (0.585-0.975) in pattern of all patients (adjustment for the propensity score as the covariate), respectively.
Table 4 shows the length of hospital stay in the unmatched and propensity score-matched groups. Table 4 excludes deceased and transferred patients. Hence, the number of patients in Table 4 is different from that in Table 1. There was a significant difference in the length of hospital stay between the two groups in the unmatched analysis (rhTM vs. control; Median 19 IQR 14-29 vs. Median 17 IQR 12-27; p < 0.001). On the other hand, no significant difference in the length of hospital stay between the two groups in the propensity score-matched analysis (rhTM vs. control; Median 19 IQR 13-29 vs. Median 18 IQR 12-27; p = 0.054).

In-hospital mortality rates in the unmatched and propensity score-matched groups.
Values were indicated percentages and deaths/cases.
All p values were derived from the Chi-squared test.
rhTM, recombinant human soluble thrombomodulin.

Logistic regression analyses between the use of recombinant human soluble thrombomodulin and in-hospital mortality.
CI, confidence interval; IPTW, inverse probability of treatment weighting; OR, odds ratio.
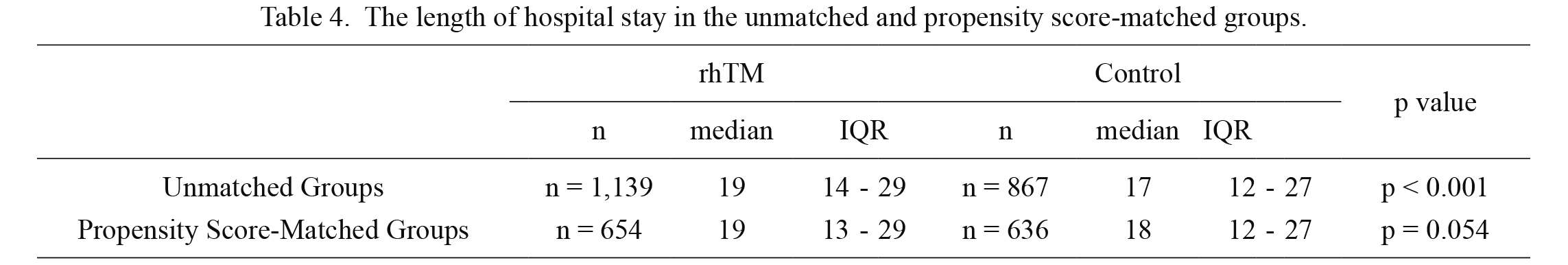
The length of hospital stay in the unmatched and propensity score-matched groups.
Excluding deceased and transferred patients.
All p values were derived from Mann-Whitney U test.
IQR, interquartile range; rhTM, recombinant human soluble thrombomodulin.
The current study reported the clinical effect of rhTM for acute cholangitis with DIC.
Pathophysiology and mortality in DIC may differ by an underlying disease. Hence, the current study focused on the analysis of acute cholangitis. Acute cholangitis is a potentially fatal systemic condition characterized by infected bile juice, which can occur due to bile duct obstruction or the presence of bile duct stones (Okuda et al. 2018). As a result, sepsis may occur due to acute cholangitis (Okuda et al. 2018). Recently, because of the use of Endoscopic Biliary Drainage (EDB) or intravenous antibiotics, the survival rate has also improved (Okuda et al. 2018). However, treatment of severe acute cholangitis may still be challenging even with adequate EBD or intravenous antibiotics, because this disease is sometimes associated with sepsis-induced DIC, which can lead to multiple organ failure (Okuda et al. 2018). The Tokyo Guideline 18 for acute cholangitis were the first in the world to make a statement about anticoagulant therapy for acute cholangitis induced DIC and showed that the administration of rhTM may be considered for severe cholangitis complicated with DIC, although the evidence level for this recommendation was low (level D) (Miura et al. 2018). Only a few reports on anticoagulant therapy for acute cholangitis-induced DIC exist, so very little evidence exists that can form a basis for the selection of anticoagulant agents for this condition (Nakahara et al. 2013; Suetani et al. 2015; Morita et al. 2019). Thus, it is significant to examine the clinical effect of rhTM on acute cholangitis associated with DIC.
This study has two strengths. First, by using a large-scale nationwide DPC database of 72 months of more than 1,000 hospitals in Japan, we were able to analyze a large number of eligible patients. The large sample size of the current study is an advantage, compared to the small sample sizes of previous studies on the efficacy of rhTM (Suetani et al. 2015; Vincent et al. 2019). Second, we used propensity score analyses to adjust for confounding factors affecting treatment choice and outcomes. Propensity score matching is a powerful tool by which we can simulate a randomized experiment-like situation by comparing groups with similar observed characteristics without specifying the relationships between confounders and outcomes (Rosenbaum and Rubin 1985; Griswold et al. 2010).
After propensity score matching, we found significant differences in in-hospital mortality rates between rhTM and control groups. Before propensity score matching, there were differences in the baseline characteristics of rhTM and control groups, and there was no significant difference in in-hospital mortality rates. However, after propensity score matching, the baseline characteristics of the rhTM and control groups were balanced, and in-hospital mortality rates in the rhTM group were significantly lower. Further, in order to examine the robustness of the results, we added IPTW and adjustment for the propensity score as the covariate. As a result, the in-hospital mortality of rhTM use was significantly lower. These multiple propensity score analyses suggest that rhTM use may contribute to a reduction of in-hospital mortality in patients with acute cholangitis with DIC. Some previous studies using DPC data showed that rhTM use had no significant effect on mortality in the patients with DIC (Murata et al. 2015; Tagami et al. 2015a, c; Umegaki et al. 2020). The result of the current study is the first report to show the efficacy of rhTM on in-hospital mortality in patients with acute cholangitis with DIC using DPC data. We were able to analyze a large number of cases, even if the disease was limited to acute cholangitis with DIC. We also used propensity scores to adjust for many important confounders, such as biliary drainage. These two points may have contributed to significantly lower in-hospital mortality in the rhTM group and may differ from previous studies. Based on the above, we determined that rhTM should be used positively for the treatment of patients with acute cholangitis with DIC.
Also, we compared the length of hospital stay of the rhTM and control groups as a secondary outcome. As a result, the length of hospital stay in the rhTM group was significantly longer before propensity score-matching. However, after propensity score matching, there was no significant difference in the length of hospital stay. That is, there is no difference in the length of hospital stay after the propensity score matching, and the rhTM and control groups require the same length of hospitalization. This outcome also helped to adjust confounding factors by propensity score-matching. Overall, inpatients with resolution from DIC in the early stages of hospitalization were considered to require similar length of hospital stay for treatment of acute cholangitis, regardless of rhTM use. The average hospital stay in acute care hospitals in Japan is longer than in other countries. This fact reflects the diversity of care in hospitals, probably because many hospitals in Japan offer both acute care and subsequent nursing care (Hashimoto et al. 2011). Thus, the generalization of the length of hospitalization in the current study was limited.
Several concerns and limitations must be considered in the interpretation of the current results. First, this study focused on acute cholangitis as the underlying disease associated with DIC. Therefore, this result cannot be generalized to underlying diseases other than acute cholangitis (e.g., cancer, trauma, and others.). It is necessary to research underlying diseases other than acute cholangitis for the future. Second, we could not confirm the cause of death because there was no data in the DPC database. Thus, if the cause of death was mainly due to diagnosis other than DIC, it may be reasonable that rhTM is not associated with in-hospital mortality. Third, we could not determine the exact time to the minute or hour when rhTM was administered. Also, we could not identify whether the variables used in our propensity score were ‘pre-treatment’ or ‘post-treatment’ of rhTM, and could not be used to estimate the propensity score in the latter case (Pattanayak et al. 2011; Sauer et al. 2013). However, from a pharmacological point of view, rhTM, with a half-life of 20 hours, could not have affected the other interventions and medications on Day 1 or Day 2, as it results in a coagulation cascade and a delay before presenting any measurable symptom changes and laboratory findings (Nakashima et al. 1998; Moll et al. 2004; Saito et al. 2007). rhTM has a more significant safety margin than other anticoagulants (Mohri et al. 1999; Aikawa et al. 2011; Iba et al. 2014). Fourth, since DPC data does not include laboratory data or image findings, it was difficult to accurately determine the severe grade according to the Tokyo Guidelines. Instead, in the current study, we analyzed useful items such as biliary drainage, mechanical ventilator, and catecholamine that affect severity. Fifth, the treatment rate of acute cholangitis according to guidelines varies by institutions, and it is reported that the higher the number of cases, the higher the compliance rate (Murata et al. 2011a). Since academic hospitals have a large number of cases, this study used the hospital type (academic or non-academic) as a surrogate variable representing the number of the cases. In the future, it is necessary to consider analysis of institution factors using multi-level analysis. Finally, although the study population was significant, we conducted the study retrospectively in an observational manner without randomization. Although this study used propensity score methods to adjust for differences in baseline characteristics and disease severity, bias could still be present in the form of confounders that were not measured. Because of these limitations, care must be taken in interpreting the results.
In conclusion, we examined the clinical efficacy of rhTM in patients with acute cholangitis with DIC using a Japanese nationwide DPC database. The analysis using propensity scores demonstrated that the in-hospital mortality was significantly lower in rhTM group. We propose that rhTM should be used for the treatment of patients with acute cholangitis with DIC.
Grants from the Ministry of Health, Labour and Welfare, Japan, supported this research. The authors are grateful to Dr. Satoshi Miyata (Tohoku University) for statistical advice.
The authors declare no conflict of interest.