2020 Volume 252 Issue 2 Pages 143-152
2020 Volume 252 Issue 2 Pages 143-152
Secondary prevention with medications is essential for the better prognosis of patients who have experienced cardiovascular events. We aimed to evaluate the use of guideline-based medications for secondary prevention in older adults in the community settings after discharge following percutaneous coronary intervention (PCI). A retrospective cohort study was conducted using anonymized claims data of older beneficiaries in a suburban city of Japan between April 2012 and March 2015. The prescriptions of antiplatelets, statins, angiotensin-converting enzyme inhibitors (ACEi)/angiotensin II receptor blockers (ARB), and β-blockers were evaluated for 3 months before and after the month in which the participants underwent PCI. Multivariable logistic regression analysis was conducted to evaluate the associations of age (“pre-old” group [63-72 years] vs. “old” group [≥ 73 years]) and sex with the prescriptions, adjusting for whether a participant was followed-up by the PCI-performing hospital. Of 815 participants, 59.6% constituted the old group and 70.9% were men. The prescription rates for antiplatelets, statins, ACEi/ARB, and β-blockers after discharge were 94.6%, 65.0%, 59.3%, and 32.9%, respectively. The adjusted analysis indicated that statins were less likely to be prescribed for the old group (adjusted odds ratio [aOR], 0.70; 95% confidence interval [CI], 0.51-0.95; p = 0.023) and for men (aOR, 0.64; 95% CI, 0.45-0.89; p = 0.008). β-blockers were more likely to be prescribed for men (aOR, 1.66; 95% CI, 1.17-2.33; p = 0.004). Our results suggest the potential for improvements in secondary prevention by increasing the prescription rates of guideline-based medications in this population.
During the past few decades, both short-term and long-term mortality after myocardial infarction have markedly improved owing to prompt performance of coronary revascularization via percutaneous coronary intervention (PCI) combined with the initiation of and adherence to pharmacological treatment (Tjia et al. 2013; Szummer et al. 2019). The current practice guidelines developed by the Japanese Circulation Society (JCS), American Heart Association and American College of Cardiology (AHA/ACC), and European Society of Cardiology (ESC) universally recommend the use of the following four types of drugs for the secondary prevention of myocardial infarction: antiplatelets, statins, angiotensin-converting enzyme inhibitors (ACEi)/angiotensin Ⅱ receptor blockers (ARB), and β-blockers (O’Gara et al. 2013; Windecker et al. 2014; Kimura et al. 2019). Furthermore, the Japan Geriatrics Society recommends that physicians should consider starting statins for secondary prevention in patients with coronary artery disease (Kojima et al. 2016). This is of particular importance due to the substantial increase in the number of older adults undergoing PCI, which is attributed to the large aging population in Japan (Numasawa et al. 2019; Uemura et al. 2019).
Contrary to the recommendations, several studies conducted in Western and Asian countries have reported low prescription rates for guideline-based medications among older patients with coronary artery disease (Borden et al. 2011; Maddox et al. 2014; Byeon et al. 2016; Fanaroff et al. 2017; Eindhoven et al. 2018; Kang et al. 2018). In Japan, insufficient use of guideline-based medications at discharge after PCI or hospitalization for coronary artery disease has also been reported (Endo et al. 2013; Kohsaka et al. 2015; Miyachi et al. 2016; Nakao et al. 2019); however, the administration of pharmacotherapy for secondary prevention in the community settings after discharge following PCI remains unclear, despite its importance in preventing cardiac events in the future. In this study, we aimed to evaluate the use of guideline-based medications in the community settings among older adults undergoing PCI. We also aimed to assess the associations of age and sex with the prescription of guideline-based medications.
We used anonymized data regarding medical and long-term care claims of older beneficiaries of the National Health Insurance or the Late Elders’ Health Insurance system between April 2012 and March 2015 in Kashiwa City, a suburban city in the Tokyo metropolitan area of Japan. Most of the older people in Japan are beneficiaries of one of these two insurance systems (Ikegami et al. 2011). The National Health Insurance system is designed for those who have retired or do not have employer-based insurance. All individuals 75 years of age or older are enrolled in the Late Elders’ Health Insurance, irrespective of previous health insurance coverage. In April 2013, more than 402,000 citizens resided in Kashiwa City, including 88,000 (22%) that were more than 65 years of age. An agreement between Kashiwa City and the University of Tokyo allowed us to utilize the medical and long-term care claims data for research purposes. The study protocol was approved by the Ethics Committee of the University of Tokyo (approval number 18-109). The requirement of obtaining informed consent was waived because of the anonymous nature of the data.
During the data anonymization process, birth years were converted from continuous to 5-year range categories. For example, a person born between 1940 and 1944 was considered 68 to 72 years old as of January 1, 2013. Based on the available data, we categorized the study participants into a pre-old group (63-72 years) and an old group (≥ 73 years) based on the approximated birth year data available.
Study populationThe study participant selection process is shown in Fig. 1, and the study design is presented in Fig. 2. Initially, there were approximately 96,900 older beneficiaries between April 2012 and March 2015. We selected participants who underwent PCI during the same period (n = 1,217). For each participant, we defined the index month as the first month undergoing PCI during the study period. We excluded participants with a history of coronary artery bypass grafting before their first PCI during the study period. We limited participants to those with at least 3 months of baseline and follow-up data, resulting in 899 remaining participants. We then excluded participants whose claims for prescription drugs were unavailable because of bundled payments or receipt of public welfare, for example. As a result, the study ultimately included 815 participants for analysis.

Selection of the study participants.
CABG, coronary artery bypass grafting; LEHI, Late Elders’ Health Insurance; LTCF, Long-term care facility; NHI, National Health Insurance; PCI, percutaneous coronary intervention.

Schematic diagram of the study design.
The latest JCS 2018 guidelines recommend secondary prevention with antiplatelets, statins, ACEi/ARB, and β-blockers for people undergoing PCI (Kimura et al. 2019). This recommendation has not changed since 2011 (JCS Joint Working Group 2013), and thus the guideline-based medications had not changed during the study period for this study. In this study, antiplatelets included aspirin and P2Y12 inhibitors. The same four-drug combination is generally recommended for stable coronary artery disease (e.g., stable angina) as acute coronary syndromes (e.g., acute myocardial infarction and unstable angina) (Iqbal and Serruys 2017). Prescriptions of these drugs were evaluated during the 3 months before and after the index month (Fig. 2). We did not evaluate the drug prescriptions during the index month because we could not distinguish prescriptions administered before and after hospitalization, or at discharge due to a lack of information regarding the exact date of the prescriptions.
Statistical analysisDescriptive statistics were used to summarize baseline characteristics of the study participants during the index month, including prescriptions of guideline-based medications during the 3 months before the index month. Frailty for each participant was assigned based on a care needs level of 1 to 5 according to the presence of certified long-term care needs (Tsutsui and Muramatsu 2005). The changes in medications from the baseline to follow-up periods were tested using the McNemar’s test. We compared the proportions of participants who were prescribed guideline-based medications according to age group and sex by using the chi-squared test. The associations of age and sex with prescriptions were evaluated using multivariable logistic regression analysis, adjusting for follow-up at the PCI-performing hospital, and adjusted odds ratios (aOR) and 95% confidence intervals (CI) were reported. Participants that received at least one prescription of any of the guideline-based medications from the PCI-performing hospital during the 3-month follow-up period were considered to be followed-up at the PCI-performing hospital. These participants were expected to have more severe conditions with increased comorbidities and complications. Further, we conducted an exploratory analysis to compare prescription rates after PCI by the chi-squared test between participants who underwent acute PCI (i.e., PCI for acute myocardial infarction and unstable angina) and those that underwent elective PCI (i.e., PCI for all others), which could be determined by medical procedure data for participants who underwent PCI in April 2014 or after. p < 0.05 was considered statistically significant. All analyses were conducted using STATA version 16.0 (Stata Corp. LP, College Station, TX, USA).
The study included 815 participants; of these, 59.6% were in the old group (≥ 73 years) and 70.9% were men (Table 1). The study participants underwent PCI in 40 different hospitals (the number of participants at a given hospital ranged from 1 to 357). More than 90% of the participants underwent PCI at one of the top five hospitals. The old group included more women than the pre-old group (32.9% vs. 23.4%). The proportions of participants with long-term care needs were 5.9% at baseline and 7.5% during the follow-up period, with higher frequencies for the old group and women. The participants were prescribed the following drugs during the baseline period: antiplatelets, 58.3%; statins, 42.2%; ACEi/ARB, 54.8%; and β-blockers, 27.9%. Additionally, the old group was more likely to receive antiplatelets than the pre-old group, and men were more likely than women to be prescribed antiplatelets and statins.

Characteristics of the study participants.
Frequencies (percentages) are shown, except for the p values.
ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor antagonists.
aDuring the data anonymization process, the birth year was converted from continuous to 5-year range categories.
bComparison between the pre-old (63-72 years) and old (≥ 73 years) groups.
cPrescriptions of drugs during the 3 months before the index month.
Prescription rates of guideline-based medications increased after PCI, irrespective of age, sex, and follow-up at the PCI-performing hospital, with some exceptions (Table 2). No statistically significant increases in prescriptions were observed for ACEi/ARB or β-blockers in the old group, women, or follow-up by hospitals/clinics other than the PCI-performing hospital group.
Prescriptions of individual guideline-based medications after discharge are shown in Table 2 and Fig. 3. During the 3 months after the index month, participants were prescribed the following: antiplatelets, 94.6%; statins, 65.0%; ACEi/ARB, 59.3%; and β-blockers, 32.9%. Statins were less likely to be prescribed to the old group than to the pre-old group (61.7% vs. 69.9%; p = 0.016), and they were less likely to be prescribed to men than to women (62.5% vs. 71.3%; p = 0.016). Moreover, β-blockers were less likely to be prescribed to women than to men (25.7% vs. 35.8%; p = 0.005). Participants followed-up by the PCI-performing hospital were more likely to be prescribed all of the guideline-based medications (p < 0.001 for antiplatelets, statins, and β-blockers, p = 0.003 for ACEi/ARB).
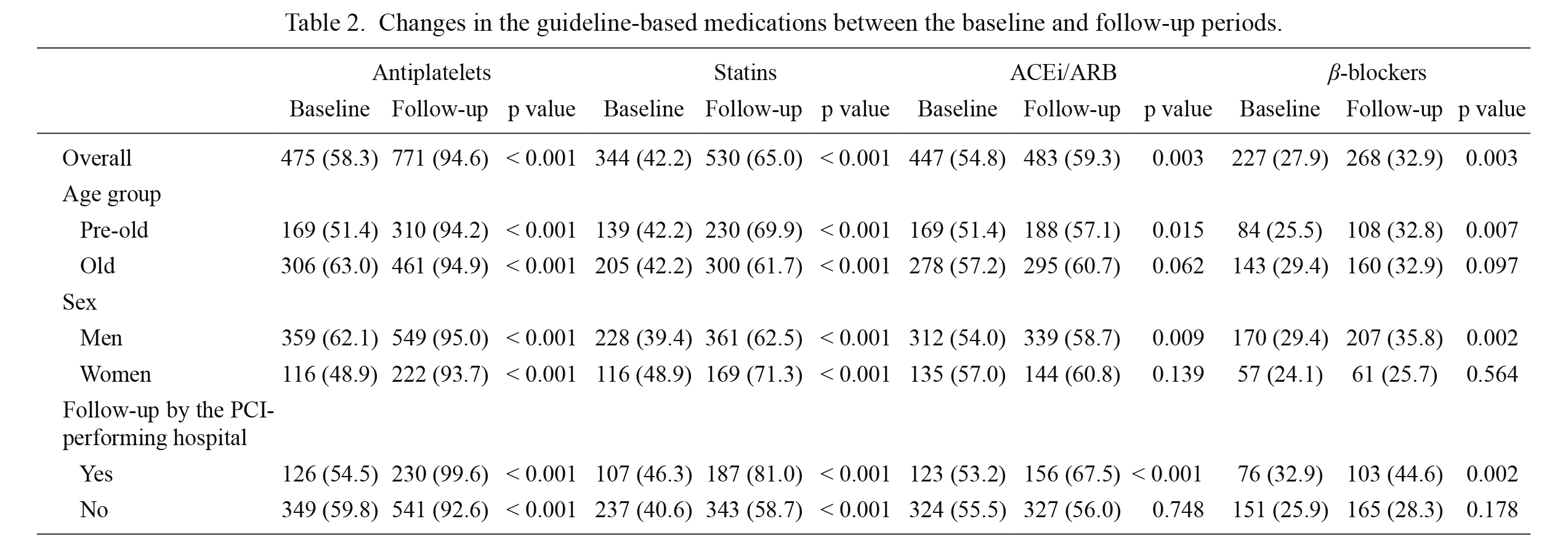
Changes in the guideline-based medications between the baseline and follow-up periods.
Frequencies (percentages) are shown, except for the p values.
ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor antagonists; PCI, percutaneous coronary intervention.

Prescription rates of guideline-based medications after discharge.
Prescription rates of the indicated medications are shown according to the age group (A) and sex (B).
ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor antagonists.
The associations of age and sex with individual guideline-based prescriptions after PCI are shown in Table 3. The old group was less likely to be prescribed statins than the pre-old group (aOR, 0.70; 95% CI, 0.51-0.95; p = 0.023). Statins were less likely to be prescribed to men than to women (aOR, 0.64; 95% CI, 0.45-0.89; p = 0.008), whereas β-blockers were more likely to be prescribed to men than to women (aOR, 1.66; 95% CI, 1.17-2.33; p = 0.004). There were no differences in prescriptions of the other guideline-based medications in terms of age and sex.

Associations of age and sex with prescription of guideline-based medications after discharge.
ACEi, angiotensin-converting enzyme inhibitors; aOR, adjusted odds ratio; ARB, angiotensin II receptor antagonists; CI, confidence interval.
The exploratory analysis was conducted in participants who underwent PCI after April 2014 (n = 247) after excluding those with a procedure code for PCI with high-speed rotating percutaneous transluminal atherectomy catheter (without diagnosis) (n = 10). This analysis included 51 acute PCI (20.6%; 16 acute myocardial infarction and 35 unstable angina) and 196 elective PCI (79.4%) participants; 151 (61.1%) participants were in the old group and 171 (69.2%) participants were men. The proportions of acute PCI tended to be higher in the pre-old group (24.0% vs. 18.5% for the old group) and men (22.2% vs. 17.1% for women).
The prescription rates of guideline-based medications in participants who underwent PCI after April 2014 were similar to those of overall study participants (Table 4). Participants who underwent acute PCI were more likely to be prescribed β-blockers, and tended to be more frequently prescribed statins (Table 4).

Exploratory analysis according to the indications for PCI.
Frequencies (percentages) are shown, except for the p values.
Participants who underwent PCI in or after April 2014 were included in this analysis (n = 247).
ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor antagonists; PCI, percutaneous coronary intervention.
In this study, we demonstrated that a substantial proportion of older adults that underwent PCI did not receive some of the guideline-based medications recommended for secondary prevention in the community settings after discharge. Although the old group was more likely to be prescribed antiplatelets at baseline, which may be a reflection of a higher frequency of previous cardiovascular events, almost all of the study participants were prescribed antiplatelets after PCI regardless of age and sex. The majority of study participants were prescribed ACEi/ARB at baseline, and prescription rates increased after PCI with no apparent differences based on age or sex. Only one-third of the study participants were prescribed β-blockers, which could be partially explained by the low proportion of acute PCIs seen in the exploratory analysis. This may also partially explain the lower prescription rate of β-blockers in women than in men.
The prescription rate of statins at baseline was higher in men than in women; however, after PCI, it was higher in women than in men. In addition, the prescription rate of statins was similar in the pre-old and old groups at baseline; however, after PCI, the prescription rate increase was greater in the pre-old group. These differences were considered to be attributed to prescribing decisions based on serum cholesterol levels, which are generally higher in women and the younger population (Roth et al. 2011). Low cholesterol levels in the older adults may have indicated a terminal decline in the last years of life (Charlton et al. 2018); therefore, some of the omitted statin prescriptions could have been appropriate. Nevertheless, we considered statins to be under-used in this population at high risk for cardiovascular events because we expected most of the study participants to be fit (not require long-term care) with enough life expectancy to benefit from secondary preventive medications.
Comparisons with previous studies performed in JapanOur findings complement those obtained from registry-based studies performed in Japan that had indicated insufficient use of guideline-based medications at the time of hospital discharge. The JCD-KiCS study showed that among 1,612 patients that underwent PCI (mean age, 67 years) at 14 hospitals between 2008 and 2009, aspirin and statins were frequently prescribed (97.1% and 82.3%, respectively); however, ACEi/ARB and β-blockers were less frequently prescribed (63.4% and 69.2%, respectively) at the time of discharge (Endo et al. 2013). These findings were similar to those of other related studies (Kohsaka et al. 2015; Sawano et al. 2017). Additionally, an age older than 80 years was associated with fewer prescriptions of guideline-based medications, including dual antiplatelet therapy, statins, ACEi/ARB, and β-blockers (Endo et al. 2013). One study, which focused on statins and included 13,024 patients with established coronary artery disease (mean age, 69 years; 37.3% underwent PCI), found that the presence of chronic kidney disease was associated with the non-prescription of statins at discharge (Sawano et al. 2017). Our study also showed an association between older age and lower frequency of statin prescription; however, this might have been confounded by unconsidered or unmeasured factors, such as lower renal function, which were not included in the insurance claims data.
Some studies have reported the use of guideline-based medications for patients with acute myocardial infarction. The Tokyo CCU network study showed that patients with acute myocardial infarction (mean age, 68 years; 83.5% underwent PCI) were prescribed the following mediations during hospitalization: aspirin, 93.6%; thienopyridine (a P2Y12 inhibitor), 73.1%; statins, 65.0%; ACEi/ARB, 58.3%; and β-blockers, 38.8% (Miyachi et al. 2016). The prescription rates of guideline-based medications in this study were quite similar to our results. More recently, the JROAD-DPC study of patients with acute myocardial infarction (mean age, 69 years; 85.7% underwent PCI) at 741 hospitals showed that there were wide variations in prescription rates among hospitals, and that the median prescription rates at discharge were 80% (interquartile range [IQR], 75%-85%) for aspirin, 68% (IQR, 58%-76%) for statins, 60% (IQR, 47%-70%) for ACEi/ARB, and 51% (IQR, 36%-63%) for β-blockers (Nakao et al. 2019). Compared to our results, despite the low rate of aspirin, the greater use of β-blockers was consistent with the findings from the exploratory analysis in the present study.
Comparisons with previous studies performed in other countriesCompared with our results, higher prescription rates, especially for β-blockers and statins, were often reported in Western and other Asian countries. To some extent, the differences may be explained by the higher frequency of elective PCI in Japan as compared to other countries (Bradley et al. 2015; Kohsaka et al. 2015; Inohara et al. 2019). In addition, differences in reimbursement and payment schemes between other countries and Japan might explain the use of guideline-based medications. Furthermore, our study found that men were less likely to be prescribed statins; however, studies conducted in other countries often reported lower prescription rates of guideline-based medications for women rather than for men.
In the United States, antiplatelet agents, statins, and β-blockers were all prescribed to 66.0% of the 293,795 patients with stable angina that underwent PCI between 2007 and 2009 (Borden et al. 2011). The prescription rates for antiplatelet therapy, statins, ACEi/ARB, and β-blockers were 99.2%, 84.7%, 60.7%, and 75.9%, respectively, at discharge. The TRANSLATE-ACS study showed that 10,870 patients that underwent PCI (with data regarding angina status; median age, 60 years) from 2010 to 2012 were prescribed aspirin, P2Y12 inhibitors, statins, ACEi/ARB, and β-blockers at rates of 98.7%, 99.6%, 95.5%, 74.5%, and 93.4%, respectively, at discharge (Fanaroff et al. 2017). Another study reported that, among patients with coronary artery disease at outpatient cardiology practices (mean age, 68 years; 21.7% underwent PCI in the previous 12 months), 66.5% were prescribed statins, ACEi/ARB, and β-blockers (Maddox et al. 2014). Men were more likely than women to be prescribed all three of the drugs, without any associations of older age with the three-drug combination.
In Sweden, national registry data showed that approximately 80% and 50% of patients with ST-elevation myocardial infarction and non-ST-elevation myocardial infarction, respectively, underwent PCI during 2013 and 2014 (Szummer et al. 2019). For patients with ST-elevation myocardial infarction, dual antiplatelet therapy, statins, and β-blockers were prescribed to approximately 90% of patients, and ACEi/ARB was prescribed to approximately 80% of patients. In the Netherlands, prescriptions for patients with acute myocardial infarction (mean age, 67 years; 53% underwent PCI) were evaluated 1 year after discharge (Maddox et al. 2014). There were differences in the prescription rates of guideline-based medications based on sex; women were less likely than men to be prescribed aspirin (77% vs. 83%), P2Y12 inhibitors (72% vs. 78%), statins (79% vs. 87%), ACEi/ARB (71% vs. 75%), and β-blockers (81% vs. 82%). More recently, prescriptions of guideline-based medications for patients with ST-elevation myocardial infarction (mean age, 64 years) that were referred to a tertiary hospital for primary PCI between 2014 and 2016 in Switzerland were studied (Bruggmann et al. 2020). At discharge, prescription rates for aspirin, P2Y12 inhibitors, statins, ACEi/ARB, and β-blockers were 98.6%, 93.9%, 83.8%, 98.6%, and 97.1%, respectively. One year after discharge, these prescription rates had decreased, especially for P2Y12 inhibitors and statins. Female sex and age older than 65 years were factors associated with incomplete prescriptions for all drugs at discharge and one year after discharge.
A study performed in South Korea showed that the prescription rate of all of aspirin, P2Y12 inhibitors, statins, ACEi/ARB, and β-blockers was 75.7% at discharge for 494 patients with acute coronary syndrome, and there was a tendency for lower prescription rates with increasing age and female sex (Byeon et al. 2016). These prescription rates decreased over time to 34.2% and 21.3% at 12 and 18 months after discharge, respectively. Another study using national insurance claims data reported that the prescription rates for aspirin, P2Y12 inhibitors, statins, ACEi/ARB, and β-blockers were 94.4%, 96.1%, 86.5%, 63.5%, and 67.4%, respectively (Kang et al. 2018). All five recommended medications were prescribed to less than half of the patients (44.2%), and there was no difference in the prescription rate based on sex.
Strengths and limitationsOne of the strengths of this study was that the use of claims data enabled the investigation of all prescriptions from any hospital or clinic after the participants were discharged. Evaluating all prescriptions is generally difficult in registry-based or hospital-based studies. To avoid underestimation of the prescription rates, we carefully selected the study participants by using not only medical claims data, but also long-term care claims and related data, to identify those without claims data for prescription drugs.
There were several limitations to this study. We could not evaluate prescriptions at discharge from the hospital because the data regarding the exact dates of the prescriptions were not available. However, medications are rarely introduced in general practice after discharge from a hospital (Bruggmann et al. 2020); therefore, improvements in prescription rates at discharge may be the most important target for intervention. In addition, data regarding diagnoses and severity of disease for PCI (e.g., ST-elevation or non-ST-elevation myocardial infarction, or unstable or stable angina) were generally not available for this study although these may have affected the prescription rates of guideline-based medications (Endo et al. 2013; Byeon et al. 2016; Miyachi et al. 2016; Fanaroff et al. 2017; Szummer et al. 2019). However, in this study, the majority of participants might have had stable coronary artery disease, not acute coronary syndrome, according to the exploratory analysis and previous reports from Japan (Kohsaka et al. 2015; Inohara et al. 2019); and the four-drug combination is not always recommended for those with stable coronary artery disease. Specifically, there is a lack of sufficient evidence supporting the use of ACEi/ARB in patients without hypertension and β-blockers in patients with stable coronary artery disease (JCS Joint Working Group 2019). Moreover, we could not completely distinguish participants undergoing their first PCI because of the short duration of the study period. Therefore, some of the study participants had already received secondary prevention at baseline. As with other studies using claims databases, we were not able to know whether the participants took their prescribed drugs, the reasons for the prescription or non-prescription of the drugs, and the reasons for discontinuation of the drugs. Lack of laboratory test results in the claims database limited us to evaluate adverse events appropriately. Some reasons for the non-prescription of statins for older adults were considered, including statin intolerance, muscular disorders (such as myopathy and rhabdomyolysis), liver disorders, and new-onset diabetes (Russo et al. 2009; Zhang et al. 2013; Mancini et al. 2016). We considered the guideline-based medications to be appropriate for most of the study participants who underwent PCI without the need for long-term care; however, the non-prescription of some of the recommended drugs might have been appropriate for some participants because the potential risks of adverse effects outweighed the expected benefits. Further evidence is needed to individualize some specific populations by evaluating the benefits, risks, and dosing of guideline-based medications for older adults (Peeters et al. 2017; Madhavan et al. 2018). Finally, the generalizability of the findings from this study to other areas in Japan and other countries may be limited because of the wide variations in adherence to the guidelines (Maddox et al. 2014; Nakao et al. 2019). Our results may have been influenced by policies or directions of some of the hospitals included in the study.
ConclusionsThe present study used claims data to demonstrate that guideline-based medications are not always prescribed for older adults in the community settings after discharge following PCI. Although the non-prescription of some drugs is a result of appropriate individualized treatment, further studies are needed to identify the reasons for non-prescriptions of guideline-based medications unrelated to individualized treatment. Our results suggest the potential for improvements in secondary prevention with increased prescription of guideline-based medications in this population.
The authors declare no conflict of interest concerning the present study. On the other hand, K.S., H.Y., and H.M. are also affiliated with the Department of Healthcare Quality Assessment at The University of Tokyo. The department is a social collaboration department supported by grants from the National Clinical Database, Johnson & Johnson K.K., and Nipro Corporation. K.S. reports receiving a portion of his salary from joint research funding by AstraZeneca K.K. of the JST-OPERA Program. M.S. received a grant from Takeda Japan Medical Office Funded Research Grant 2018 outside of the submitted work.