Abstract
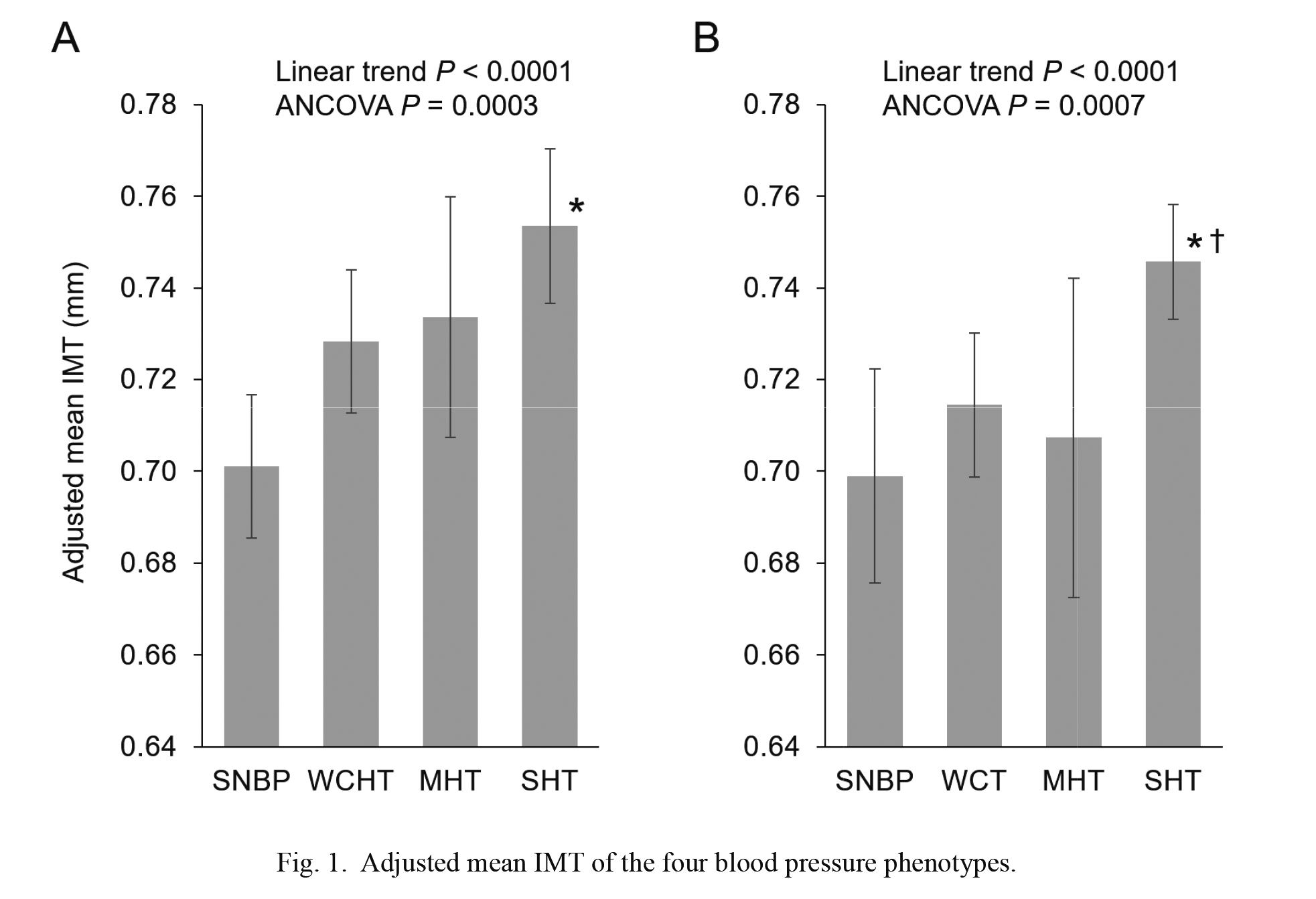
White coat hypertension is defined as elevated blood pressure in the office, but a normal blood pressure out-of-office, whereas masked hypertension is defined as elevated blood pressure in the office, but normal out-of-office blood pressure. The objective was to investigate the associations between these blood pressure phenotypes and carotid artery changes. Conventional blood pressure, ambulatory blood pressure, and carotid ultrasonography were evaluated in 851 Ohasama residents (31.8% men; mean age 66.3 years). The blood pressure phenotypes were defined by the ordinary thresholds (140/90 mmHg for conventional blood pressure, 135/85 mmHg for daytime blood pressure) and then by the 2017 American College of Cardiology/American Heart Association (ACC/AHA) thresholds for hypertension (130/80 mmHg for both conventional and daytime blood pressure), irrespective of antihypertensive medication treatment status. Blood pressure phenotypes were linearly associated with the mean intima-media thickness of the carotid artery in ascending order for sustained normal blood pressure, white coat hypertension, masked hypertension, and sustained hypertension according to the ordinary thresholds and the 2017 ACC/AHA thresholds (both linear trends P < 0.0001) after adjustments for possible confounding factors. The odds ratios for the presence of carotid plaques showed similar linear trends with the blood pressure phenotypes according to the 2017 ACC/AHA thresholds (linear trend P < 0.0191). In conclusion, there was a close relationship between blood pressure phenotypes and carotid artery changes, suggesting that blood pressure phenotypes as defined by ambulatory blood pressure are potentially useful for risk stratification of carotid artery changes in the Japanese general population.
Introduction
Hypertension has been the leading cause of cardiovascular death (Ikeda et al. 2012; Benjamin et al. 2018). For accurate diagnosis of hypertension, hypertension guidelines recommend using not only office blood pressure, but also out-of-office blood pressure (Whelton et al. 2018; Williams et al. 2018; Umemura et al. 2019). The guidelines recommend diagnosing the blood pressure phenotypes of sustained normal blood pressure (SNBP), white coat hypertension (WCHT), masked hypertension (MHT), and sustained hypertension (SHT). WCHT is defined as elevated blood pressure in the office, but normal out-of-office blood pressure, whereas MHT is defined as elevated blood pressure in the office, but normal out-of-office blood pressure. These phenotypes have a different prognostic significance (Bobrie et al. 2004; Ohkubo et al. 2005; Hansen et al. 2007; Stergiou et al. 2014; Satoh et al. 2016), and they should be treated differently (Whelton et al. 2018; Williams et al. 2018; Umemura et al. 2019). WCHT has a low risk of cerebrocardiovascular disease, and it should therefore be handled with health management, such as daily salt restriction and appropriate exercise without antihypertensive medication. On the other hand, masked hypertension is associated with metabolic disorders, hypertensive organ damage, and a poor prognosis. Therefore, an antihypertensive medication using the out-of-office blood pressure as an index is required in addition to lifestyle modifications. These blood pressure phenotypes have been studied intensively in relation to prognosis (Bobrie et al. 2004; Ohkubo et al. 2005; Hansen et al. 2007; Stergiou et al. 2014; Satoh et al. 2016) and end organ damage (Cavallini et al. 1995; Puato et al. 2008). In terms of the methodology of measuring out-of-office blood pressure, there have been two approaches with different concepts. Ambulatory blood pressure monitoring measures unrestricted blood pressure in daily life during daytime and during nighttime sleep. On the other hand, home blood pressure measurement obtains self-measurements of blood pressure at home under certain measurement conditions for a long period of time (Umemura et al. 2019). In both blood pressure measurement methodologies, MHT and SHT have been reported to have a poor prognosis compared with SNBP both in Western countries (Bobrie et al. 2004; Hansen et al. 2007; Stergiou et al. 2014) and in Japan (Ohkubo et al. 2005; Satoh et al. 2016). However, with respect to carotid artery changes as end organ damage, there has been insufficient evidence in the Japanese population for their relationship with blood pressure phenotypes evaluated by ambulatory blood pressure monitoring. In Europe and the United States, most studies were based on ambulatory blood pressure (Cavallini et al. 1995; Puato et al. 2008), but in Japan, most studies were carried out by home blood pressure measurement (Hara et al. 2007; Matsui et al. 2007; Fukuhara et al. 2013) rather than by ambulatory blood pressure monitoring. There has been only one report based on ambulatory blood pressure monitoring that investigated the blood pressure phenotypes and carotid artery changes in Japan, in which 332 outpatients with chronically treated essential hypertension were examined (Tomiyama et al. 2006).
The blood pressure phenotypes obviously depend on the definition of the reference values for hypertension. Most current guidelines for hypertension state the reference values for hypertension as the threshold of conventional blood pressure (140/90 mmHg), with the exception of the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline for hypertension (Whelton et al. 2018), which lowered the threshold to 130/80 mmHg. As a result, the prevalence of hypertension has been substantially increased by the reclassification of hypertension (Muntner et al. 2018). However, one study (Poudel et al. 2019) have investigated the relationship between the blood pressure phenotypes according to the 2017 ACC/AHA thresholds and hypertensive end organ damage, but no studies of carotid artery changes have been published.
The objective of the present study was to investigate carotid artery changes by the blood pressure phenotypes (WCHT, MHT, SNBP, and SHT) defined based on a combination of conventional and ambulatory blood pressures according to both the ordinary thresholds and the 2017 ACC/AHA thresholds for hypertension in a general Japanese population.
Methods
Design
This cross-sectional study was a part of the Ohasama Study, a community-based blood pressure measurement project started in 1986. The socioeconomic and demographic characteristics of this region and the full details of the project have been described elsewhere (Imai et al. 1993). The study complies with the Declaration of Helsinki, and institutional review boards of Teikyo University School of Medicine and Showa Pharmaceutical University approved the study protocol.
Study population
In 1998, Ohasama had a total population of 7,202 persons, and 3,077 persons were 55 years old or older. Persons who were bedridden, psychiatrically ill, or hospitalized (n = 185), as well as those who were not at home during the study nurses’ normal working time (n = 492), were not eligible for this study. Of those who were eligible (2,400 persons), 851 (35.5%) provided details of their medical history and cardiovascular risk factors, underwent ambulatory blood pressure monitoring and carotid ultrasound examination, and provided their written, informed consent to be included in the study.
Carotid ultrasonography
Ultrasound imaging was performed with a real-time, B-mode ultrasound imaging unit (Toshiba Sonolayer SSA-250A; Toshiba Corp., Tokyo, Japan) with an annular array probe at 7.5-MHz generating an axial resolution of 0.25 mm. Carotid ultrasonograms were examined by trained physicians blinded to subject characteristics following a standardized protocol. Intima-media thickness (IMT) of the near and far walls of the common carotid arteries was measured at a point that was 1.0-cm distal from the carotid bifurcation. The mean IMT was defined as the mean of the maximal wall thicknesses of the near and far walls of the right and left common carotid arteries. The examiners then looked for plaques in the bilateral carotid artery bifurcations and in the external, internal, and common carotid arteries. Plaque was defined as a focal lesion relative to adjacent segments, with either calcified deposits alone or a combination of calcification and non-calcified material protruding into the lumen (Bots et al. 1997). The details of the protocol have been previously reported, and the reproducibility of the IMT measurement has also been shown (Hara et al. 2007; Shintani et al. 2007).
Blood pressure measurements
Ambulatory blood pressure was monitored using an ABPM-630 (Nippon Colin, Komaki, Japan; 1992-2004) (Imai et al. 1990) and an FM800 (Fukuda Denshi, Tokyo, Japan; 2004-2010) (Nakamura et al. 2010), which are fully automatic cuff-oscillometric method devices that were preset to measure blood pressure every 30 min. Each device was attached by well-trained study nurses who visited each subject on a weekday morning and detached the device the following morning. The participants were asked to record their daily activities in a diary, including the time they went to bed and the time they arose. According to the diary, daytime blood pressure and nighttime blood pressure were defined as the calculated mean of the ambulatory blood pressure values recorded while awake and asleep, respectively. Artefactual measurements during recordings were defined according to reported criteria (Imai et al. 1990). Conventional blood pressure was measured twice consecutively in a sitting position, after a rest interval of at least 2 min, by a physician using a mercury sphygmomanometer or an automatic USM-700F device (UEDA Electric Works Co. Ltd., Tokyo, Japan) (Imai et al. 1992) during 1992-2002, and a HEM907 device (Omron Healthcare Co. Ltd, Kyoto, Japan) (White and Anwar 2001) during 2002-2010, at the time of carotid ultrasound examination. The average of the two readings was defined as conventional blood pressure. All of these devices have been validated and meet the criteria of the Association for the Advancement of Medical Instrumentation (1987).
Categorization of participants according to blood pressure phenotypes
Participants were classified into the four blood pressure phenotypes based on their conventional blood pressure and daytime blood pressure. The ordinary thresholds of hypertension, 140/90 mmHg for conventional blood pressure and 135/85 mmHg for daytime blood pressure (Williams et al. 2018; Umemura et al. 2019), were used first. SNBP was defined as less than the thresholds of both conventional blood pressure and daytime blood pressure. WCHT was greater than or equal to only the thresholds of conventional blood pressure. MHT was greater than or equal to only the thresholds of daytime blood pressure. SHT was greater than or equal to both thresholds of conventional blood pressure and daytime blood pressure. Then, the participants were also classified into four groups of blood pressure phenotypes according to the 2017 ACC/AHA thresholds, 130/80 mmHg for both conventional blood pressure and daytime blood pressure (Whelton et al. 2018).
In line with previous papers (Bobrie et al. 2004; Ohkubo et al. 2005; Shintani et al. 2007), blood pressure phenotypes were defined by combinations of conventional blood pressure and ambulatory blood pressure, irrespective of antihypertensive medication treatment status.
Data analysis
The biochemical examinations and the definitions of cardiovascular diseases, hypercholesterolemia, and diabetes mellitus in the Ohasama Study have been reported previously (Ohkubo et al. 2005; Hara et al. 2007; Satoh et al. 2016). Participants’ characteristics were compared among the blood pressure phenotypes by analysis of variance or the χ2 test. Analysis of covariance was performed for mean IMT among the blood pressure phenotypes with adjustment for sex, age, body mass index, smoking status, drinking status, hypercholesterolemia, diabetes mellitus, history of cardiovascular disease, and use of antihypertensive medication. Tukey’s multiple comparison test was used to compare the adjusted mean IMT among the blood pressure phenotypes. The odds ratio for plaque among the blood pressure phenotypes was calculated with adjustment for the same covariates as above. Linear trend P values were for linear trend of the adjusted mean IMT or the adjusted odds ratio across the blood pressure phenotypes in the ascending order of SNBP, WCHT, MHT, and SHT. These analyses were repeated in subgroup analyses of participants with and without antihypertensive treatment.
SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses. For all analyses, two-tailed P < 0.05 was considered significant.
Results
The 851 participants (31.8% men; mean age, 66.3 ± 6.4 years) consisted of 272 (32.0%) with SNBP, 255 (30.0%) with WCHT, 92 (10.8%) with MHT, and 232 (27.2%) with SHT according to the ordinary thresholds. The corresponding numbers and prevalence of participants according to the 2017 ACC/AHA thresholds were 125 (14.7%), 258 (30.3%), 52 (6.1%), and 416 (48.9%).
Significant differences were observed in sex, age, body mass index, smoking, alcohol drinking, use of antihypertensive medication, ambulatory blood pressure, conventional blood pressure, mean IMT, and plaque among the blood pressure phenotypes according to both the ordinary thresholds (Table 1) and the 2017 ACC/AHA thresholds (Table 2).
The adjusted mean IMT increased progressively in the order of SNBP, WCHT, MHT, and SHT (linear trend P < 0.0001) for both the ordinary (Fig. 1, panel A) and the 2017 ACC/AHA thresholds (Fig. 1 panel B). The adjusted mean IMT was greater in subjects with SHT than in those with SNBP (P < 0.0001 by Tukey’s multiple comparison test). Similar linear trends were observed in subgroup analyses with and without antihypertensive treatment (Table 3); the interaction P values among the linear trend × with and without antihypertensive treatment were not significant.
The adjusted odds ratios for plaque displayed similar tendencies in terms of the linear trend in the order of SNBP, WCHT, MHT, and SHT according the 2017 ACC/AHA thresholds (linear trend P = 0.0191, Fig. 2, panel B). A marginally significant trend was observed among the blood pressure phenotypes according to the ordinary thresholds (linear trend P = 0.0696, Fig. 2, panel A). In the subgroup analyses by treatment status (Table 4), a roughly similar linear tendency was observed only in treated patients.
The analyses were repeated with the four blood pressure phenotypes according to 24-h ambulatory blood pressure (Table 5 and Table 6) and nighttime blood pressure (Table 7 and Table 8) instead of daytime blood pressure, and roughly similar results were obtained.
Discussion
The present study showed that carotid IMT was linearly related with the blood pressure phenotypes of WCHT, MHT, SNBP, and SHT defined based on a combination of conventional blood pressure and daytime ambulatory blood pressure in a general Japanese population. Patients with SHT had significantly greater mean IMT than those with SNBP. A linear relationship was observed in the blood pressure phenotypes according to both the ordinary thresholds and the 2017 ACC/AHA thresholds.
These findings extend previous studies of the relationship between blood pressure phenotypes based on ambulatory blood pressure and carotid artery changes conducted in the United States and European countries (Cavallini et al. 1995; Puato et al. 2008) to the Japanese general population. Home blood pressure has been well accepted because of its relatively low cost and its feasibility for individuals, and it has also been widely available for routine clinical assessment in Japan. Along with the widespread use of home blood pressure devices, home blood pressure measurement rather than ambulatory blood pressure monitoring as representative of out-of-office blood pressure has been mainly used in studies of carotid changes as evidence of hypertensive end organ damage (Hara et al. 2007; Matsui et al. 2007; Fukuhara et al. 2013), with the exception of one study that reported the relationship between the blood pressure phenotypes based on a combination of conventional and daytime blood pressures and carotid artery changes in 332 outpatients with chronically treated essential hypertension (Tomiyama et al. 2006). They reported that maximal IMT defined as the maximal intima-media thickness including plaques was significantly greater in MHT (1.93 ± 1.07 mm) than in SNBP (1.61 ± 0.67 mm) and WCHT (1.60 ± 0.82 mm). Although there were differences in the methods of evaluation of IMT and the statistical analyses, the present study also found a progressive increase in the IMT with the blood pressure phenotypes in participants taking and not taking antihypertensive medication. Given that marked differences exist in the epidemiology of cardiovascular disease between the USA or European countries and Japan (Umemura et al. 2019), the present research conducted in a Japanese general population has some importance as a cardiovascular epidemiological study.
Participants with WCHT showed similar IMT and odds ratio for plaque compared with those with SNBP. This result was in line with previous studies (Cavallini et al. 1995; Tomiyama et al. 2006; Hara et al. 2007), which noted that carotid IMT was similar in patients with WCHT and those with SNBP. However, others (Puato et al. 2008; Fukuhara et al. 2013) suggested that carotid IMT was greater in participants with WCH than in those with SNBP. A systematic review (Cuspidi et al. 2015b) including 3,478 untreated patients from 10 studies reported that the IMT was significantly greater in WCHT than in SNBP (standardized mean difference 0.54 ± 0.13, P < 0.01). However, the papers covered in the review involved only untreated patients with various definitions of hypertension, and no papers used the 2017 ACC/AHA thresholds. Further studies are needed in terms of the possible effect of white coat hypertension on carotid artery damage.
There were no significant differences in the mean IMT and the odds ratio of plaque between subjects with MHT and those with SNBP. Previous prospective studies of cardiovascular outcomes (Bobrie et al. 2004; Ohkubo et al. 2005; Hansen et al. 2007; Stergiou et al. 2014; Satoh et al. 2016) consistently reported increased hazard ratios for fatal and non-fatal cardiovascular outcomes. The International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO) (Hansen et al. 2007) researchers reported, relative to SNBP, significantly increased hazard ratios of MHT for cardiovascular events, strokes, and cardiac events (1.62, 1.73, and 1.63, all P < 0.001) in their meta-analysis that included individual participant data of 7,030 subjects from the general population in four countries. Similarly, in relation to carotid artery changes, several studies reported thicker IMT in subjects with MH than in those with SNBP (Tomiyama et al. 2006; Hara et al. 2007; Matsui et al. 2007; Fukuhara et al. 2013). A systematic review (Cuspidi et al. 2015a) that included 2,752 untreated patients from 5 studies reported an increased IMT in patients with MH than in those with SNBP (0.763 ± 0.057 vs. 0.681 ± 0.024 mm, P < 0.01); however, when corrected for publication bias, the difference between MH and NT became borderline in their review. Further studies of the blood pressure phenotypes with carotid artery changes were still needed to confirm the effect of MH on carotid artery alteration.
The 2017 ACC/AHA thresholds used for the definition of the blood pressure phenotypes were examined in the general population in Japan. Generally, guidelines for hypertension depend on the properties of the population in each country. The 2017 ACC/AHA guideline for hypertension is essentially the guideline for the United States population. However, the concept of lowering the reference blood pressure for hypertension and preventing cardiovascular disease from the early stage is a universal idea, and research using it as an alternative threshold for hypertension should be promoted even in other countries (Satoh et al. 2019). When the 2017 ACC/AHA thresholds were used to define the blood pressure phenotypes, the number of subjects with SNBP and those with MHT decreased by about half, and those with SHT almost doubled. Despite the changes in the prevalences of the blood pressure phenotypes, the linear trends of IMT and the odds ratios of plaque among the blood pressure phenotypes were grossly similar to those determined according to the ordinary thresholds. These results indirectly support the validity of the 2017 ACC/AHA thresholds in terms of hypertensive end organ damage.
The present study must be interpreted within the context of its potential limitations. First, cross-sectional data do not allow cause-and-effect relationships to be determined. Second, the present analyses were restricted to measurements of common carotid IMT. The question of whether the results differ by arterial segment cannot therefore be answered using the present analyses. Third, this study measured only hard plaque. Because the carotid ultrasonography devices used in the Ohasama study were used from 1992, the measurement function is old and cannot measure plaque properties. The conditions change when we change a device, so that only data measured with the same device was included in this study. Finally, selection bias must be considered before generalizing the present findings, since only 35.5% of individuals who were eligible to participate consented to do so. Nevertheless, there may not have been in fact much selection bias, since the IMT values in the present study were not significantly different from those reported by other large population studies (Bonithon-Kopp et al. 1996; Bots et al. 1997) in which measurements of IMT were taken in areas that were free of focal atherosclerotic lesions (plaque).
In conclusion, there was a close relationship between the blood pressure phenotypes and carotid artery changes. Conventional blood pressure measurements alone could not identify individuals with SHT, who have a significant risk for increased mean IMT. However, the combination of conventional blood pressure and ambulatory blood pressure measurements can identify such individuals. Blood pressure phenotypes as defined by ambulatory blood pressure are potentially useful for risk stratification for carotid artery changes in the Japanese general population.
Acknowledgments
This study was supported by Grants for Scientific Research, Ministry of Education, Culture, Sports, Science and Technology, Japan (17H04126, 17K15853, 17K19930, 18K09674, 18K09904, 18K17396, 19K19466, 19H03908, 19K10662, and 20K08612); Grant-in-Aid for Young Scientists of Showa Pharmaceutical University H28-4; the Japan Arteriosclerosis Prevention Fund; Grant-in-aid from the Ministry of Health, Labour, and Welfare, Japan (H29-Junkankitou-Ippan-003 and 20FA1002); The Academic Contributions from Pfizer Japan Inc.; Scholarship donations from Chugai Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd.; Research Support from Astellas Pharma Inc. and Takeda Pharmaceutical Co., Ltd.; The Health Care Science lnstitute Research Grant. Health Science Center Research Grant; Takeda Science Foundation.
Conflict of Interest
The authors declare no conflict of interest concerning the present study. On the other hand, K. Asayama, H. Metoki, Y. Imai, and T. Ohkubo concurrently held the position of director of the Tohoku Institute for Management of Blood Pressure, which was supported by Omron Healthcare Co., Ltd.
References
-
Association for the Advancement of Medical Instrumentation
(1987) American National Standard. Electronic or automated sphygmomanometers ANSI/AAMI SP10-1987, Association for the Advancement of Medical Instrumentation, USA.
-
Benjamin,
E.J.,
Virani,
S.S.,
Callaway,
C.W.,
Chamberlain,
A.M.,
Chang,
A.R.,
Cheng,
S.,
Chiuve,
S.E.,
Cushman,
M.,
Delling,
F.N.,
Deo,
R.,
de Ferranti,
S.D.,
Ferguson,
J.F.,
Fornage,
M.,
Gillespie,
C.,
Isasi,
C.R., et al.
(2018) Heart disease and stroke statistics: 2018 update: a report from the American Heart Association. Circulation, 137, e67-e492.
-
Bobrie,
G.,
Chatellier,
G.,
Genes,
N.,
Clerson,
P.,
Vaur,
L.,
Vaisse,
B.,
Menard,
J. &
Mallion,
J.M.
(2004) Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA, 291, 1342-1349.
-
Bonithon-Kopp,
C.,
Touboul,
P.J.,
Berr,
C.,
Leroux,
C.,
Mainard,
F.,
Courbon,
D. &
Ducimetière,
P.
(1996) Relation of intima-media thickness to atherosclerotic plaques in carotid arteries. The Vascular Aging (EVA) Study. Arterioscler. Thromb. Vasc. Biol., 16, 310-316.
-
Bots,
M.L.,
Hoes,
A.W.,
Koudstaal,
P.J.,
Hofman,
A. &
Grobbee,
D.E.
(1997) Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation, 96, 1432-1437.
-
Cavallini,
M.C.,
Roman,
M.J.,
Pickering,
T.G.,
Schwartz,
J.E.,
Pini,
R. &
Devereux,
R.B.
(1995) Is white coat hypertension associated with arterial disease or left ventricular hypertrophy? Hypertension, 26, 413-419.
-
Cuspidi,
C.,
Sala,
C.,
Tadic,
M.,
Rescaldani,
M.,
De Giorgi,
G.A.,
Grassi,
G. &
Mancia,
G.
(2015a) Untreated masked hypertension and carotid atherosclerosis: a meta-analysis. Blood Press., 24, 65-71.
-
Cuspidi,
C.,
Sala,
C.,
Tadic,
M.,
Rescaldani,
M.,
Grassi,
G. &
Mancia,
G.
(2015b) Is white-coat hypertension a risk factor for carotid atherosclerosis? A review and meta-analysis. Blood Press. Monit., 20, 57-63.
-
Fukuhara,
M.,
Arima,
H.,
Ninomiya,
T.,
Hata,
J.,
Hirakawa,
Y.,
Doi,
Y.,
Yonemoto,
K.,
Mukai,
N.,
Nagata,
M.,
Ikeda,
F.,
Matsumura,
K.,
Kitazono,
T. &
Kiyohara,
Y.
(2013) White-coat and masked hypertension are associated with carotid atherosclerosis in a general population: the Hisayama study. Stroke, 44, 1512-1517.
-
Hansen,
T.W.,
Kikuya,
M.,
Thijs,
L.,
Björklund-Bodegård,
K.,
Kuznetsova,
T.,
Ohkubo,
T.,
Richart,
T.,
Torp-Pedersen,
C.,
Lind,
L.,
Jeppesen,
J.,
Ibsen,
H.,
Imai,
Y. &
Staessen,
J.A.;
IDACO Investigators
(2007) Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J. Hypertens., 25, 1554-1564.
-
Hara,
A.,
Ohkubo,
T.,
Kikuya,
M.,
Shintani,
Y.,
Obara,
T.,
Metoki,
H.,
Inoue,
R.,
Asayama,
K.,
Hashimoto,
T.,
Harasawa,
T.,
Aono,
Y.,
Otani,
H.,
Tanaka,
K.,
Hashimoto,
J.,
Totsune,
K., et al.
(2007) Detection of carotid atherosclerosis in individuals with masked hypertension and white-coat hypertension by self-measured blood pressure at home: the Ohasama study. J. Hypertens., 25, 321-327.
-
Ikeda,
N.,
Inoue,
M.,
Iso,
H.,
Ikeda,
S.,
Satoh,
T.,
Noda,
M.,
Mizoue,
T.,
Imano,
H.,
Saito,
E.,
Katanoda,
K.,
Sobue,
T.,
Tsugane,
S.,
Naghavi,
M.,
Ezzati,
M. &
Shibuya,
K.
(2012) Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLoS Med., 9, e1001160.
-
Imai,
Y.,
Abe,
K.,
Sasaki,
S.,
Minami,
N.,
Munakata,
M.,
Sekino,
H.,
Nihei,
M. &
Yoshinaga,
K.
(1990) Determination of clinical accuracy and nocturnal blood pressure pattern by new portable device for monitoring indirect ambulatory blood pressure. Am. J. Hypertens., 3, 293-301.
-
Imai,
Y.,
Abe,
K. &
Sekino,
H.
(1992) Evaluation of autonomic devices for blood pressure measurement. Annual Review of Nephrology, 1992, 55-61 (in Japanese).
-
Imai,
Y.,
Satoh,
H.,
Nagai,
K.,
Sakuma,
M.,
Sakuma,
H.,
Minami,
N.,
Munakata,
M.,
Hashimoto,
J.,
Yamagishi,
T.,
Watanabe,
N.,
Yabe,
T.,
Nishiyama,
A.,
Nakatsuka,
H.,
Koyama,
H. &
Abe,
K.
(1993) Characteristics of a community-based distribution of home blood pressure in Ohasama in northern Japan. J. Hypertens., 11, 1441-1449.
-
Matsui,
Y.,
Eguchi,
K.,
Ishikawa,
J.,
Hoshide,
S.,
Shimada,
K. &
Kario,
K.
(2007) Subclinical arterial damage in untreated masked hypertensive subjects detected by home blood pressure measurement. Am. J. Hypertens., 20, 385-391.
-
Muntner,
P.,
Carey,
R.M.,
Gidding,
S.,
Jones,
D.W.,
Taler,
S.J.,
Wright,
J.T. Jr. &
Whelton,
P.K.
(2018) Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation, 137, 109-118.
-
Nakamura,
K.,
Kikuya,
M.,
Hara,
A.,
Hirose,
T.,
Obara,
T.,
Metoki,
H.,
Asayama,
K.,
Inoue,
R.,
Ohkubo,
T.,
Totsune,
K. &
Imai,
Y.
(2010) Validation of the FM-800 ambulatory blood pressure monitor according to the Association for the Advancement of Medical Instrumentation criteria and the International Protocol. Clin. Exp. Hypertens., 32, 523-527.
-
Ohkubo,
T.,
Kikuya,
M.,
Metoki,
H.,
Asayama,
K.,
Obara,
T.,
Hashimoto,
J.,
Totsune,
K.,
Hoshi,
H.,
Satoh,
H. &
Imai,
Y.
(2005) Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J. Am. Coll. Cardiol., 46, 508-515.
-
Poudel,
B.,
Booth,
J.N. 3rd, Sakhuja, S.,
Moran,
A.E.,
Schwartz,
J.E.,
Lloyd-Jones,
D.M.,
Lewis,
C.E.,
Shikany,
J.M.,
Shimbo,
D. &
Muntner,
P.
(2019) Prevalence of ambulatory blood pressure phenotypes using the 2017 American College of Cardiology/American Heart Association blood pressure guideline thresholds: data from the Coronary Artery Risk Development in Young Adults study. J. Hypertens., 37, 1401-1410.
-
Puato,
M.,
Palatini,
P.,
Zanardo,
M.,
Dorigatti,
F.,
Tirrito,
C.,
Rattazzi,
M. &
Pauletto,
P.
(2008) Increase in carotid intima-media thickness in grade I hypertensive subjects: white-coat versus sustained hypertension. Hypertension, 51, 1300-1305.
-
Satoh,
M.,
Asayama,
K.,
Kikuya,
M.,
Inoue,
R.,
Metoki,
H.,
Hosaka,
M.,
Tsubota-Utsugi,
M.,
Obara,
T.,
Ishiguro,
A.,
Murakami,
K.,
Matsuda,
A.,
Yasui,
D.,
Murakami,
T.,
Mano,
N.,
Imai,
Y., et al.
(2016) Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the Ohasama study. Hypertension, 67, 48-55.
-
Satoh,
M.,
Asayama,
K.,
Murakami,
T.,
Kikuya,
M.,
Metoki,
H.,
Imai,
Y. &
Ohkubo,
T.
(2019) Stroke risk due to partial white-coat or masked hypertension based on the ACC/AHA guideline’s blood pressure threshold: the Ohasama study. Hypertens. Res., 42, 120-122.
-
Shintani,
Y.,
Kikuya,
M.,
Hara,
A.,
Ohkubo,
T.,
Metoki,
H.,
Asayama,
K.,
Inoue,
R.,
Obara,
T.,
Aono,
Y.,
Hashimoto,
T.,
Hashimoto,
J.,
Totsune,
K.,
Hoshi,
H.,
Satoh,
H. &
Imai,
Y.
(2007) Ambulatory blood pressure, blood pressure variability and the prevalence of carotid artery alteration: the Ohasama study. J. Hypertens., 25, 1704-1710.
-
Stergiou,
G.S.,
Asayama,
K.,
Thijs,
L.,
Kollias,
A.,
Niiranen,
T.J.,
Hozawa,
A.,
Boggia,
J.,
Johansson,
J.K.,
Ohkubo,
T.,
Tsuji,
I.,
Jula,
A.M.,
Imai,
Y. &
Staessen,
J.A.;
International Database on HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) Investigators
(2014) Prognosis of white-coat and masked hypertension: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension, 63, 675-682.
-
Tomiyama,
M.,
Horio,
T.,
Yoshii,
M.,
Takiuchi,
S.,
Kamide,
K.,
Nakamura,
S.,
Yoshihara,
F.,
Nakahama,
H.,
Inenaga,
T. &
Kawano,
Y.
(2006) Masked hypertension and target organ damage in treated hypertensive patients. Am. J. Hypertens., 19, 880-886.
-
Umemura,
S.,
Arima,
H.,
Arima,
S.,
Asayama,
K.,
Dohi,
Y.,
Hirooka,
Y.,
Horio,
T.,
Hoshide,
S.,
Ikeda,
S.,
Ishimitsu,
T.,
Ito,
M.,
Ito,
S.,
Iwashima,
Y.,
Kai,
H.,
Kamide,
K., et al.
(2019) The Japanese society of hypertension guidelines for the management of hypertension (JSH 2019). Hypertens. Res., 42, 1235-1481.
-
Whelton,
P.K.,
Carey,
R.M.,
Aronow,
W.S.,
Casey,
D.E. Jr.,
Collins,
K.J.,
Dennison Himmelfarb,
C.,
DePalma,
S.M.,
Gidding,
S.,
Jamerson,
K.A.,
Jones,
D.W.,
MacLaughlin,
E.J.,
Muntner,
P.,
Ovbiagele,
B.,
Smith,
S.C. Jr.,
Spencer,
C.C., et al.
(2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol., 71, 2199-2269.
-
White,
W.B. &
Anwar,
Y.A.
(2001) Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press. Monit., 6, 107-110.
-
Williams,
B.,
Mancia,
G.,
Spiering,
W.,
Agabiti Rosei,
E.,
Azizi,
M.,
Burnier,
M.,
Clement,
D.L.,
Coca,
A.,
de Simone,
G.,
Dominiczak,
A.,
Kahan,
T.,
Mahfoud,
F.,
Redon,
J.,
Ruilope,
L.,
Zanchetti,
A., et al.
(2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J., 39, 3021-3104.