2020 Volume 252 Issue 4 Pages 329-337
2020 Volume 252 Issue 4 Pages 329-337
Disasters influence various health conditions; however, little has been reported about urinary symptoms. The objective of this study is to evaluate whether night-time urinary frequency was influenced by the Great East Japan Earthquake (GEJE) in March 2011. We also evaluated seasonal variation of night-time frequency, which may affect the primary objective. A retrospective chart review was conducted on 300 evaluable patients who resided in the impacted area: 263 men with benign prostatic hyperplasia and/or overactive bladder and 37 women with overactive bladder. Data concerning night-time frequency were collected repeatedly every three months from March 2009 until March 2014, then compared yearly and seasonally among same patients. In addition, night-time frequency was analyzed for potential relations to sex, age, comorbidities, and whether residences had been destroyed. There was a significant increase of night-time frequency during 2011-2013 when compared yearly with 2009 and 2010. In seasonal comparisons of the entire period, night-time frequency was greater during autumn and winter compared with summer. In quarterly comparisons, a sudden increase was not observed after the GEJE, but night-time frequency was increased significantly in spring, summer and autumn in 2011 when compared with the corresponding seasons in 2010. While hypertension was related to exacerbation of night-time frequency during winter, we did not find any factors associated with increase after the disaster out of sex, age, comorbidities or residential situations. In conclusion, night-time urinary frequency is increased shortly after the GEJE and remains elevated for the following three years along with seasonal variation.
On March 11th 2011, the Great East Japan Earthquake and tsunami (GEJE) struck broad areas of east Japan and its devastating impact resulted in 19,729 deaths and 2,559 missing (Fire and Disaster Management Agency of Japan 2020). Survivors would suffer from various problems including traumatization, bereavement, financial problems and environmental changes resulting from evacuation and/or relocations. It is presumed to take from months to several years of recovery until reconstruction of the psychosocial phase (Kõlves et al. 2013). Disasters of this scale are well understood to cause not only psychological stress but also various physical problems (van den Berg et al. 2008). Several studies have reported elevated blood pressure and the increased prevalence of cardiovascular events after the GEJE (Aoki et al. 2012; Yamauchi et al. 2013).
At present, lower urinary tract symptoms (LUTS) are known to be influenced by psychological stresses (Breyer et al. 2013; Lai et al. 2015), environmental changes (Sanford and Rodriguez 2017), and also other medical conditions (Coyne et al. 2009). In particular, nocturia is a multifactorial condition with several underlying causes that include benign prostatic hyperplasia, overactive bladder, polyuria, nocturnal polyuria, sleep disturbance, psychological problems, and behavioral problems (Drake 2012). However, little has been reported on changes in urinary symptoms associated with disaster.
Herein we studied whether the GEJE influenced night-time urinary frequency (NF) over a five-year period before and after the GEJE among patients with LUTS in Kesennuma City. Additionally, as seasonal variations in nocturia have been previously described (Yoshimura et al. 2007; Choi et al. 2015), we collected data multiple times every three months for a total of five years and compared NF on a yearly basis and a seasonal basis. We also investigated comorbid diseases and loss of habitation in order to identify risk factors for increased NF resulting from the GEJE with seasonal variation.
Kesennuma is a city located in the northeast coastal area of Japan with temperate climate and four seasons similar to many other parts of Japan. Out of a total population of 73,489 in Kesennuma City at the time of the GEJE, 1,218 (1.7%) died in the GEJE, 214 (0.3%) went missing, and 40,331 (54.9%) had their habitation inundated by the tsunami (Statistics Bureau, Ministry of Internal Affairs and Communications of Japan 2013). Of 25,457 family units, 8,483 dwelling houses (33.3%) were completely destroyed and 20,086 (27.3%) residents were evacuated to shelters or temporary residences. As at March 2014, 6,631 still resided within prefabricated housing in Kesennuma City (Miyagi Prefecture 2014).
With approval from the Internal Ethical Board of Kesennuma City Hospital (No. 859), we retrospectively reviewed charts of 523 patients who had visited the Department of Urology at Kesennuma City Hospital for benign prostatic hyperplasia (BPH) or overactive bladder (OAB) during July 1st-October 31st, 2014. We excluded patients who started medical treatment after the GEJE or who lacked comparable data for either pre or post-disaster period. Patients with urological cancers, advanced chronic kidney diseases, and with indwelling/intermittent urinary catheterization were also excluded.
Data were obtained from medical records listing numbers of NF or International Prostate Symptom Score (IPSS) nocturia scores. When the recorded numbers of NF exceeded 5 times, it was counted as 5 following IPSS nocturia scoring protocol. NF was collected repeatedly for each patient every three months from March 12th, 2009 until March 11th, 2014. For descriptive purposes, we defined that each yearly timeframe started on March 12th and ended on March 11th, i.e., the year 2009 and 2010 are considered before the disaster and the year 2011, 2012 and 2013 after the disaster. In this study, one year was divided into quarters and seasons were defined as follows: Spring: March 12th-June 11th, Summer: June 12th-September 11th, Autumn: September 12th-December 11th, Winter: December 12th-March 11th.
Subsequently, mean NF of pre-disaster (2009-2010) was compared with post-disaster (2011-2013), and mean NF of summer was compared with winter (2009-2013) in subgroups stratified by sex, age at the time of the GEJE (≥ 80, 70-79, and ≤ 69), comorbidities, and whether the residence was destroyed. As comorbidities, hypertension (HTN), diabetes mellitus (DM), stroke, coronary artery disease (CAD), and sleep disturbance (SD) were identified from the hospital database of the Japanese National Health Insurance in 2014. Destroyed residences were identified from request documents for medical bill waivers for those who lost their habitation in the GEJE.
Statistical analyses were performed using JMP® Pro 14.2.0 (SAS Institute Inc. NC, USA) and P value < 0.05 was considered statistically significant in this study. Least square means (LSM) of each year and season during the entire period (i.e., 2009-2013) were calculated by two-way repeated measures of variance (ANOVA) within subjects (same patients). Subsequently, multiple comparisons were performed by Tukey Kramer’s post hoc test. In subgroup analysis, longitudinal/seasonal changes were evaluated by paired t-test, and NF between stratified subgroups were compared by paired t-test. In addition, we investigated the factors associated with meaningful increase of NF after the GEJE or in winter using univariate chi-square analyses and multivariate logistic regression analyses. In this study, ≥ 0.5 times increases of mean NF after GEJE or in winter were considered as meaningful increase.
Out of 523 prospective patients, we identified 300 who met our criteria. Mean age ± standard deviation was 73.4 ± 8.0 years at the time of the GEJE. Out of 263 male patients, 260 and 88 were clinically diagnosed with BPH and OAB, respectively. All 37 female patients were diagnosed with OAB. Table 1 shows the patients’ characteristics and their distributions with or without HTN. Prevalence of HTN was significantly correlated with the prevalence of DM, stroke, CAD and SD. The number of patients whose NF was available at least once per year was 257 (85.7%) in 2009, 300 (100%) in 2010, 278 (92.7%) in 2011, 268 (89.3%) in 2012, and 262 (87.3%) in 2013. During the observation period, all patients were prescribed single or multiple medications at least once for LUTS. Medications included alpha-adrenergic blockers, 5-alpha-reductase inhibitors, anticholinergics, beta-3-adrenergic agonists, and prescribed herbal remedies.
Fig. 1 demonstrates yearly and seasonal variations of NF during 2009-2013. The least square means (LSM) ± standard errors (SE) of NF were 2.096 ± 0.029 times in 2009, 2.086 ± 0.025 in 2010, 2.216 ± 0.027 in 2011, 2.243 ± 0.029 in 2012, and 2.301 ± 0.029 in 2013 (Fig. 1a). NF significantly increased during 2011-2013 when compared to 2009 or 2010. Table 2 summarizes the results of multiple comparisons for each combination. Additionally, there were significant increases in winter (2.247 ± 0.024) and in autumn (2.217 ± 0.025) when compared to summer (2.120 ± 0.025) (Fig. 1b, Table 2). Although a sudden increase after the GEJE was not observed between winter 2010 and spring 2011, there were significant increases in the first three quarters (i.e., spring, summer, and autumn) in 2011 when compared to the corresponding seasons in 2010 (Fig. 2).
Mean NF of pre-disaster (2009-2010) was compared with post-disaster (2011-2013) in each stratified subgroup (n = 300). As shown in Fig. 3, there were significant increases in NF after the GEJE in most subgroups except for age ≥ 80 and with CAD (paired t-test). Subgroup of age ≥ 80 had greater NF than younger subgroups regardless of pre or post disaster (unpaired t-test). Patients with HTN and CAD also had greater NF than those without HTN and CAD in the pre-disaster period whereas the difference was not significant after the disaster.
Subsequently, mean NF of summer and winter during 2009-2013 were compared in each stratified subgroup (n = 283). As shown in Fig. 4, NF was increased in winter in most subgroups except for age ≤ 69, female, without SD and without HTN (paired t-test). Patients with HTN had greater NF than those without HTN in winter (unpaired t-test); however, the difference was not detected in summer. This tendency was also observed among patients with/without stroke, CAD and SD.
To investigate the factors associated with meaningful increase of NF after GEJE or in winter, univariate and multivariate analyses were performed. Out of total 300 patients, 76 (25.3%) experienced ≥ 0.5 times increases of mean from pre-disaster (2009-2010) to post-disaster (2011-2013) (Table 3). Out of 283 evaluable patients, 81 (28.6%) experienced ≥ 0.5 times increases of mean NF in winter compared to summer during 2009-2013 (Table 4). HTN was significantly associated with ≥ 0.5 times increases in winter in univariate analysis; however, none of the listed factors were associated with meaningful increase after the GEJE.

Patients’ characteristics and correlations with prevalence of HTN.
HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; SD, sleep disturbance.

Yearly and seasonal variations of night-time frequency during 2009-2013.
(a) Yearly variation. Night-time urinary frequency (NF) was significantly increased after the GEJE in yearly comparisons (P < 0.05 for any combination of years between 2009-2010 × 2011-2013). Differences in continuous two years were significant only between 2010 and 2011. (b) Seasonal variation. Significant increase in NF was observed in winter and autumn when compared to summer. Columns and bars describe least square means (LSM) ± standard errors (SE) calculated by repeated measures ANOVA within subjects (n = 300) during the entire period (2009-2013).
ns, no significance.
*P < 0.05; **P < 0.01.

Results of multiple comparisons for each yearly and seasonal combination.
Multiple comparisons were performed by Tukey Kramer’s post hoc test.
SE, standard error; CI, confidential interval.
*P < 0.05; **P < 0.01.

Quarterly comparisons of night-time frequency in 2010-2011.
Although night-time urinary frequency (NF) was not increased immediately after the GEJE (winter 2010-spring 2011), there were significant increases during the first three quarters after the GEJE when compared to the corresponding seasons in 2010 (Paired t-test). Columns and bars describe mean ± standard errors of NF in each quarter (n = 300).
ns, no significance.
*P < 0.05.

Pre-post disaster changes on stratified subgroups.
Vertical scales describe mean (times) ± standard errors of night-time urinary frequency (NF) in pre (mean of 2009-2010) vs. post-disaster (mean of 2011-2013) for each stratified subgroup (n = 300). NF was increased after the GEJE in most subgroups except age ≥ 80 and with CAD (Paired t-test). Patients with HTN and CAD had greater NF than those without HTN and CAD in the pre-disaster period (unpaired t-test).
HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; SD, sleep disturbance; ns, no significance.
*P < 0.05; **P < 0.01 for paired t-test.
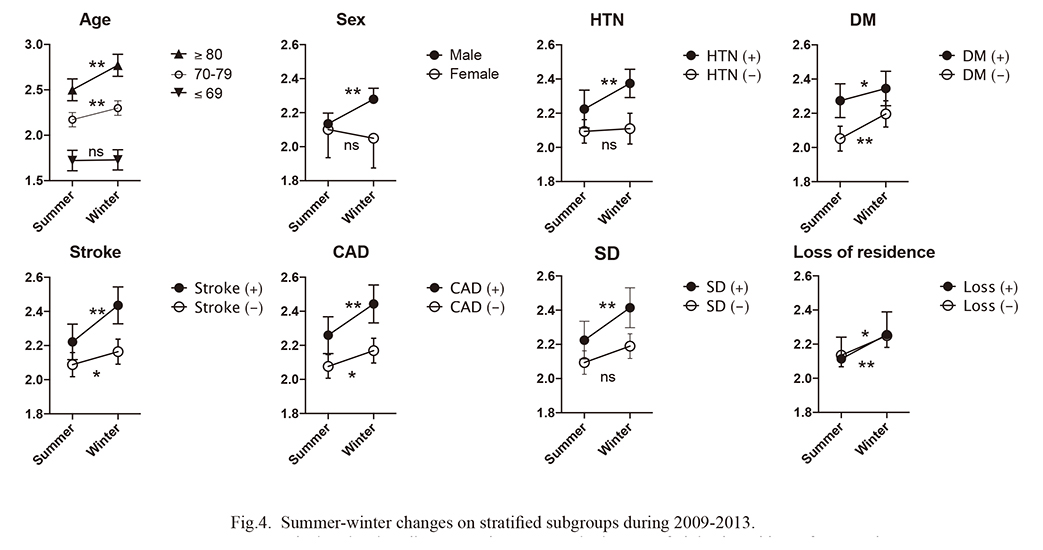
Summer-winter changes on stratified subgroups during 2009-2013.
Vertical scales describe mean (times) ± standard errors of night-time urinary frequency (NF) in summer vs. winter (mean of 5 years) for each stratified subgroup (n = 283). NF was increased during winter in most subgroups except age ≤ 69, female and without HTN (paired t-test).
HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; SD, sleep disturbance; ns, no significance.
*P < 0.05; **P < 0.01 for paired t-test.

Association with ≥ 0.5 times increase in mean NF from pre (2009-2010) to post-disaster (2011-2013).
There was no significant factor related with increase after the GEJE.
HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; SD, sleep disturbance.
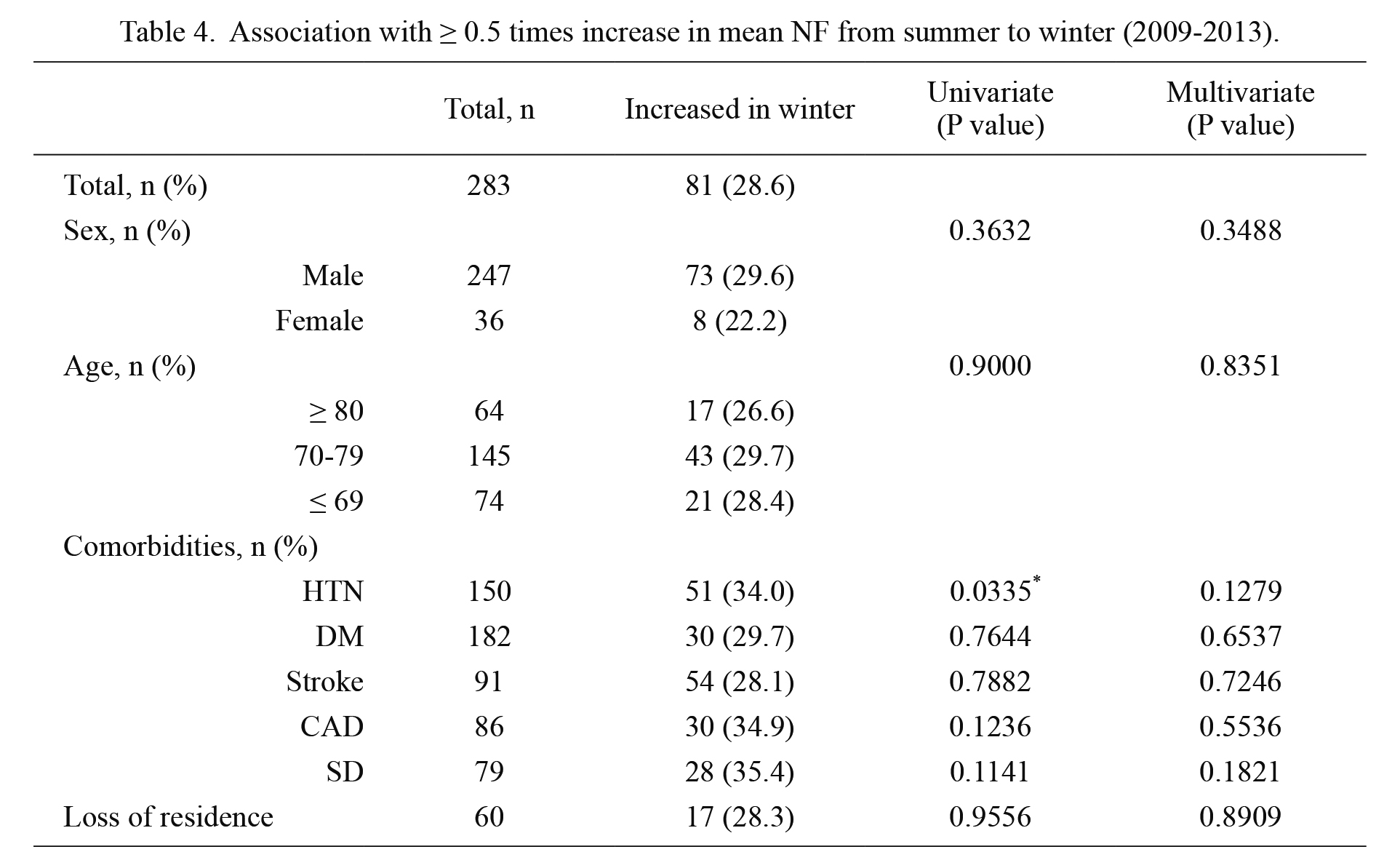
Association with ≥ 0.5 times increase in mean NF from summer to winter (2009-2013).
There was a significant relation between HTN and patients with ≥ 0.5 times increase from summer to winter in univariate analysis.
HTN, hypertension; DM, diabetes mellitus; CAD, coronary artery disease; SD, sleep disturbance.
*P < 0.05.
When compared on a yearly basis, a significant increase in NF was observed during 2011-2013 when compared to 2009 or 2010 (Fig. 1a, Table 2). Even though there was no significant difference between the quarters immediately preceding and following the GEJE, the impact may have been already present during the early phase as the significant increases were observed in the first three quarters of 2011 when compared with the corresponding seasons in 2010 (Fig. 2). Along with the seasonal variation, these results indicate the GEJE as a possible factor related to an increase in NF.
Several factors are considered to affect nocturia among disaster victims in the acute and chronic phases. Shortly after the GEJE, the incidence of acute coronary syndrome, heart failure, stroke, and cardiopulmonary arrest was increased (Aoki et al. 2012). Those events were possibly caused by sympathetic nervous activation resulting from disaster-induced stress (Kario et al. 1997; Takegami et al. 2015). Hypertension can also cause polyuria through its effect on glomerular filtration and tubular transport (Feldstein 2013). When congestive heart failure complicates hypertension, the release of atrial natriuretic peptide induces nocturnal polyuria (Feldstein 2013). Additionally, victims had consumed high-salt preservative foods in shelters during the early phase of evacuation, which can potentially induce both hypertension and nocturia (Matsuo et al. 2017). The majority of the victims were evacuated to shelters for up to several months. In the shelters, victims may hesitate to void at night when bothered by a lack of privacy, difficult access to toilets, and an unsanitary environment. This situation may worsen the urinary urgency and conversely force some victims to restrict fluid intake.
After a few months following a disaster have passed, victims are considered to confront the disillusionment phase, when mental health problems potentially arise (Kõlves et al. 2013). In a prospective cohort study, 14.6% of survivors complained of newly-onset sleep disturbance at the third year after the GEJE with a higher incidence of musculoskeletal pains (Yabe et al. 2018). Their study suggested that the GEJE had long-term and lasting effects on both psychological and physiological health. As limited physical activity among victims had been concerned as social issues, Ohira et al. (2016) reported that the proportion of overweight or obese people was increased among the GEJE survivors. Reduced exercise and obesity could also become risk factors for increase in NF (Sugaya et al. 2007; Aoki and Yokoyama 2012). Another longitudinal study of the GEJE demonstrated that the proportion of victims with more severe psychological distress was higher among those who had lived in prefabricated temporary housing for a long period (Tanji et al. 2018). Even though our data did not show the difference between residential situations, NF could be affected by multifactorial psycho-social problems including post-traumatic stress disorder, undiagnosed sleep disturbance, financial problems, bereavement, and environmental changes other than loss of residence.
There have been some clinical studies reporting correlations between psychological stress and urinary symptoms (Breyer et al. 2013; Lai et al. 2015). In experimental literatures, psychiatric stress is reported to induce urinary frequency in rat model (Smith et al. 2011). Even though the mechanism is not well established, a likely explanation is that dysregulation of the hypothalamic-pituitary-adrenal axis and subsequent release of corticotropin-releasing factor could induce visceral hypersensitivity and detrusor overactivity (Wang et al. 2017).
Previous studies revealed that hypertension, heart disease, stroke, and diabetes mellitus were the major risk factors for nocturia (Asplund 2002; Gourova et al. 2006; Fitzgerald et al. 2007; Weiss et al. 2011). Our study also showed that patients with HTN and CAD presented with greater NF in pre-disaster period, which later became insignificant after the GEJE (Fig. 3). As NF was increased in most subgroups, we did not identify any worsening factors after the GEJE (Table 3).
In addition, seasonal variation was observed independently from the effects of the GEJE. Of particular note, NF was significantly greater in winter among patients with hypertension, stroke, and CAD when compared to those without the comorbidities; however, the significance was not detected in summer. In rat models, Imamura et al. (2013) demonstrated that cold stress induced detrusor overactivity, which is mediated through the sympathetic nervous system that is also associated with transient hypertension. While seasonal variation of blood pressure has been well established (Hanazawa et al. 2017), it is still unknown whether seasonal hypertension or cold stress induces night-time diuresis. Longer sleep duration in winter may also contribute to increases of NF (Udo et al. 2009; Suzuki et al. 2019).
This study has several limitations that must be considered. Firstly, advancing age is known to be the strongest risk factor for nocturia (Asplund 2002; Fitzgerald et al. 2007), therefore, the aging effect may have contributed to the increase in NF over the five years. A large cohort of study involving 4,427 elderly volunteers revealed that the prevalence of nocturia was significantly increased after a one-year period (Hirayama et al. 2013). In our smaller dataset, the differences of NF in continuous years were insignificant except only between 2010 and 2011, which could indicate that the GEJE had some impact on nocturia.
Secondly, there was a lack of background information potentially related to LUTS, e.g., prostate volume, alcohol and smoking habits. All patients were prescribed for LUTS at least once in the observational period; however, the type of medication, changes and/or cessation of the medications were not analyzed.
Thirdly, this study was conducted only in a community hospital in Kesennuma and did not cover control samples in other affected or non-affected areas. The demographic of the candidates was biased toward elderly males having relatively severe comorbidities. Therefore, the impacts of the GEJE on the general population remain unclear.
Limitations arising from the retrospective aspect of this study and a chaotic situation during aftermath of the disaster made it more difficult to obtain reliable and sufficient materials (e.g., validated questionnaires) from both pre and post-disaster periods. While there have been some longitudinal studies using public sources of information obtained before natural disasters, to our knowledge, there has been no other report based on long-term changes in urinary symptoms in a semi-closed community affected by a great disaster.
In conclusion, an increase in night-time frequency was observed following the GEJE along with seasonal variation. Despite limitations, our study indicates the potential impact for a major disaster to cause an increase in NF. This could be informative regarding urinary care for elderly victims suffering from large-scale natural catastrophes in the future.
Dr. Shigeto Ishidoya and Mr. Vincent Cummings supported this study in terms of critical revision of the manuscript.
The authors declare no conflict of interest.