2021 年 254 巻 3 号 p. 155-161
2021 年 254 巻 3 号 p. 155-161
Management of nausea is an important dimension of palliative care. The first choice for treating nausea is antiemetics, but their efficacy is inadequate. Acupressure intervention for nausea in cancer patients has been studied as a non-pharmacological therapy, and appears to have had some effect. However, such a therapy has not been well reviewed in patients with terminal cancer. The purpose of this study was to clarify the feasibility of acupressure intervention and examine its safety and preliminary efficacy. We recruited cancer patients that fulfilled the eligibility criteria and were admitted to the palliative care unit, from August 2018 to February 2019, in Tohoku University Hospital, Japan. We conducted a longitudinal assessment of acupressure intervention in a single arm. We identified the patient’s research accomplishments and evaluated possible fainting due to the vagal reflex and symptom severity. Descriptive statistics were used to calculate the completion rate for the feasibility and Wilcoxon signed-rank tests to compare the average of continuous variables for the safety and efficacy. Twelve patients participated in this study and completed the procedure. Their average age was 70 years (SD = 9.3), and the most common primary cancer sites were the rectum and pancreas. The blood pressure and pulse rate did not drop sharply. Four patients exhibited decreased nausea but there was no statistically significant difference (P = 0.5). We suggested that acupressure has high feasibility and safety, as an intervention for patients with terminal cancer. However, no significant differences were observed regarding its effect on nausea.
Nausea care is an important in palliative care, since nausea is a symptom that reduces the patient’s Quality of life (QOL) (Davis and Walsh 2000; Hirai et al. 2006; Miyashita et al. 2007), and its prevalence in terminal cancer patients is reported to be ranged from 40% to 75% in hospices and home care (Stephenson and Davies 2006; Wood et al. 2007). Although the first choice for treatment is antiemetics corresponding to the cause of nausea, their efficacy is inadequate (Glare et al. 2004). Accordingly, both non-pharmacological and drug therapies are receiving attention.
In previous trials, acupressure intervention for nausea which is non-pharmacological therapy, appears to have had some effect (Dibble et al. 2000; Treish et al. 2003; Dibble et al. 2007; Roscoe et al. 2009; Genc et al. 2013; Molassiotis et al. 2014; Genc and Tan 2015). Acupressure stimulates the somatic afferent nerves of the skin and muscles. The somatic sensory information is carried to the cortex area of the brain and affects various biomechanical responses. Wright’s study reported the use of a wristband that continuously pressed on the acupressure site “Neiguan” of hospice patients (Wright 2005). Eighty-eight percent of the 33 cancer patients who participated in the before-after study, responded that their nausea and vomiting had improved. This study was scored on a 6-point Likert-type scale from 0 to 5 but lacked reliability and validity and did not integrate the onset and duration of intervention and evaluation time. In addition, since studies regarding acupressure interventions for terminal cancer patients have not been conducted in other ethnicities, the feasibility of implementation needs to be clarified.
This is a pilot study aimed at clarifying the feasibility of acupressure intervention, as well as at examining its safety and preliminary efficacy.
This study is a prospective single-arm before-after study with patients diagnosed with advanced cancer in a palliative care unit in a university hospital in Japan.
Participants and settingWe recruited patients admitted to the palliative care unit of Tohoku University Hospital, Japan, from August 2018 to February 2019.
The patients’ inclusion criteria comprised: (1) having a diagnosis of incurable advanced cancer; (2) being older than 20 years at the time of obtaining consent; (3) being admitted to the palliative care unit in Tohoku University Hospital; (4) ability to communicate in Japanese; (5) having Numerical Rating Scale (NRS) of nausea ≧ 1 (for example, 0 = none; 10 = severe) before the intervention; (6) ability to give consent themselves. The exclusion criteria were: (1) undergoing chemotherapy or radiotherapy for therapeutic purposes; (2) having undergone past acupressure therapy of the Neiguan and the Zusanli (Fig. 1) (Kaneko et al. 2013; Shimizu and Miyashita 2016); (3) meeting Palliative Performance Scale (PPS) (Anderson et al. 1996) score between 10 and 20; (4) having a medical history of bradycardia arrhythmias such as sick sinus syndrome, atrioventricular block or bradycardiac atrial fibrillation; (5) having mental symptoms such as delirium; or (6) being considered unsuitable for the study by the researcher (for example, due to edema at the acupressure site).
In bradycardia arrhythmia, the vagal reflex was considered as a side effect of acupressure in Oriental medicine. Since there was no report from the previous studies, we set the criteria based on the advice of the physician (S.T.) and the Japan Circulation Society Guidelines (The Japanese Circulation Society 2012). This study was performed in accordance with the principles of the Declaration of Helsinki. Approval was granted by the institutional review board of the Graduate School of Medicine, Tohoku University (Approval number 2018-1-693). Its clinical trial registration number is UMIN000033563. Informed consent was obtained from all individual participants included in the study.

Neiguan and Zusanli.
Neiguan is located on the midline of the inner forearm. Zusanli is located on the lower limb (below the knee, on the tibialis anterior muscle).
Neiguan and Zusanli were set as the acupressure sites based on the previous study (Dibble et al. 2000, 2007) and as advised by the physician (S.T.) specializing in Oriental medicine and acupuncture treatment. Neiguan located on the midline of the inner forearm and Zusanli is located on the lower limb. The researcher (H.T.) performed acupressure after receiving guidance from the physician (S.T.).
Acupressure was performed on each limb, and the pressure-time was 30 seconds for each of the acupressure points. One intervention for both limbs comprised a set. The researcher performed three sets at each of the acupressure point and the total intervention time was six minutes. The researcher checked with the patient about the strength of the pressure during interventions and adjusted the acupressure strength accordingly.
MeasurementThe following attributes were assessed.
1. Feasibility
We evaluated the patients’ benefits and probable causes of dropouts. In addition, we sought patients’ feedback on how they felt during the acupressure intervention.
2. Safety
We measured blood pressure, pulse rate, and fainting due to the vagal reflex. We confirmed a sharp drop in circulation and fainting at 4 time points; before and immediately after acupressure intervention, as well as 15 and 30 minutes after intervention. We measured vital signs at these four points in time on the advice of the physician (S.T.).
3. Efficacy
We noted symptom severity of nausea at three time points; before acupressure intervention as well as 15 and 30 minutes after intervention. We used the Edmonton Symptom Assessment System revised Japanese version (ESAS-r-j) (Yokomichi et al. 2015) before acupressure to evaluate nausea and anxiety. Edmonton Symptom Assessment System revised Japanese version includes nine items (for example, Pain; Tiredness; Drowsiness; Nausea; Lack of Appetite; Shortness of Breath; Depression; Anxiety; Best Wellbeing) that are scored on an 11-point Likert-type scale from 0 “none” to 10 “severe”. The reliability and validity of Edmonton Symptom Assessment System revised Japanese version has been established. We evaluated anxiety using Edmonton Symptom Assessment System revised Japanese version because anxiety is related to nausea. In conducting the analysis, we used the value 30 minutes after acupressure, which is the most responsive time to acupressure on the advice of the physician (S.T.).
4. Patient characteristics
From their medical records, we obtained information on the patient sex, age, primary cancer site and Palliative Performance Scale to evaluate their condition, and on the Palliative Prognostic Index (PPI) to form a prognosis (Morita et al. 1999). Information on the following factors of nausea was obtained: the number of vomiting incidents, the use of antiemetic and medical narcotics and the application of digestive tract decompression treatment, the last defecation timing, and the presence of visitors on the day of acupressure intervention. The causes of nausea include medical narcotics, constipation, digestive tract pressure, and anxiety. In this study, we investigated the medical narcotics, antiemetics, presence of visitor, the application of digestive tract decompression treatment, and last defecation timing to verify the effectiveness.
ProcedureAcupressure intervention was conducted with standard treatment and nursing care. It was limited to weekdays because sufficient medical staff was required in case the acupressure caused vagal reflex.
First, the ward physician selected eligible patients who had recently been admitted to the palliative care unit. The researcher explained as well as gave in writing the aim, procedure, and potential benefits/harms of the study to the patients who expressed interest in participating.
Second, the patients’ symptoms were evaluated using Edmonton Symptom Assessment System revised Japanese version, followed by measurement of blood pressure and pulse rate. The researcher then conducted acupressure intervention for six minutes observing the patient’s state; the patient’s blood pressure and pulse rate were evaluated immediately, as well as 15 and 30 minutes after acupressure, and nausea intensity was simultaneously measured using Numerical Rating Scale. In this study, we performed acupressure interventions twice a day, and the afternoon intervention was conducted two hours after lunch. We performed acupressure intervention at approximately 10 a.m. and 2 p.m. respectively.
Third, after the intervention, the researcher provided a brochure with instructions regarding the acupressure points/sites, to assist the patients who had completed the process, had no change in their circulation movements, and were interested in doing self-acupressure after the study.
In all cases, the researcher acquired the patient’s characteristics from the medical record with the cooperation of the physician (N.S.).
Statistical analysisDescriptive statistics were used to calculate the completion rate for the feasibility and Wilcoxon signed-rank tests to compare the average of continuous variables for the safety and efficacy. The distinct time points were before acupressure intervention and 15 and 30 minutes after intervention. In all the analyses, the significance level was set at P < 0.05, and the tests were conducted with JMP Pro version 14.0.
During the study, thirty-four cancer patients had nausea. Twenty-two of them were excluded, either because their symptoms had subsided at the time of intervention, their Palliative Performance Scale was within the 10 to 20 range, or they had bradycardia arrhythmias or heart disease. Hence, twelve patients were recruited.
Table 1 shows the participants’ descriptive statistics. Seven patients were male. Their average age was 70 years (SD = 9.3). As regards the primary site of cancer, three had rectal cancer and three had pancreatic cancer. One patient had digestive stent placement. None of the patients had received acupressure prior to the study. Eight patients were in the Palliative Performance Scale 50 condition, comprising ambulation (mainly sit/lie), activity (unable to do any work), and intake (normal or reduced). In the Palliative Prognostic Index was greater than 6 in three patients. Ten used medical narcotics.
In patient B (Table 2), it was more than three days since the last defecation, due to fasting. None of the patients exhibited vomiting. Patients A, C and K (Table 2) were only using additional antiemetic drugs prior to acupressure intervention.
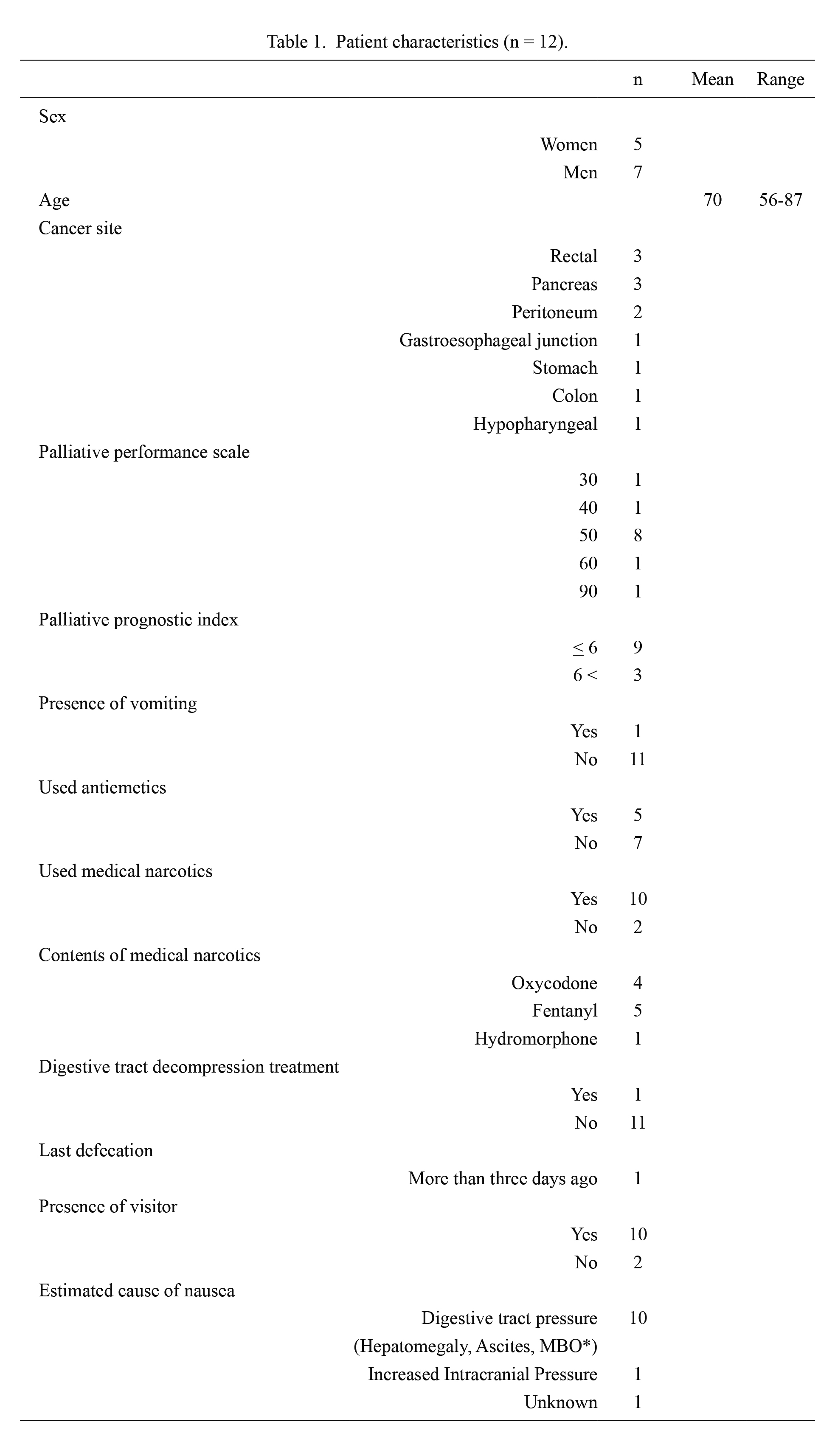
Patient characteristics (n = 12).
*Malignant Bowel Obstructions.
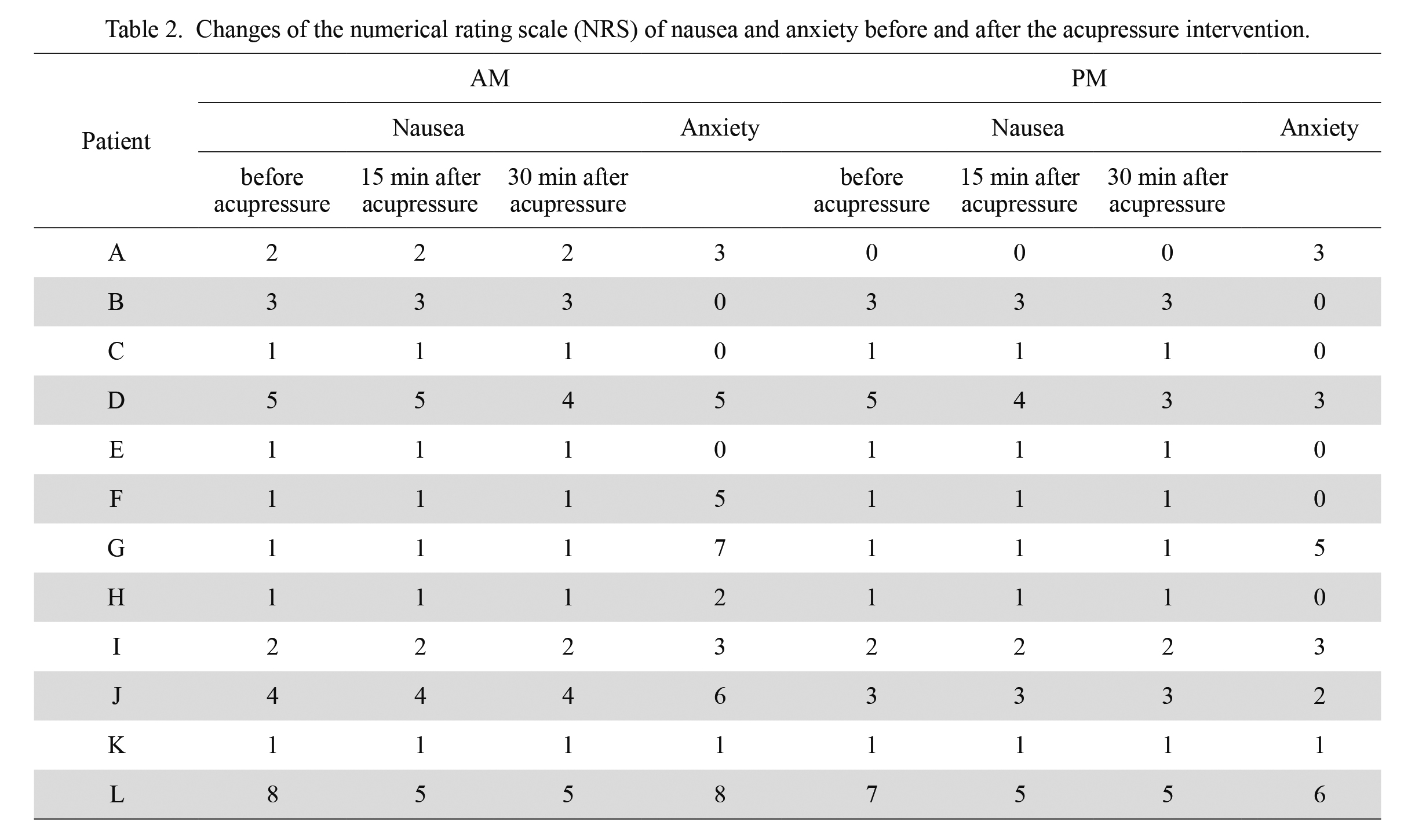
Changes of the numerical rating scale (NRS) of nausea and anxiety before and after the acupressure intervention.
All 12 patients completed the study’s various treatments and measurements. They did not report being uncomfortable during the study.
SafetyTable 3 shows the blood pressure and pulse rate, both of which did not drop sharply. None of the patients experienced vagal reflex. Although blood pressure and pulse rate decreased during the study period, the changes were within the normal range.
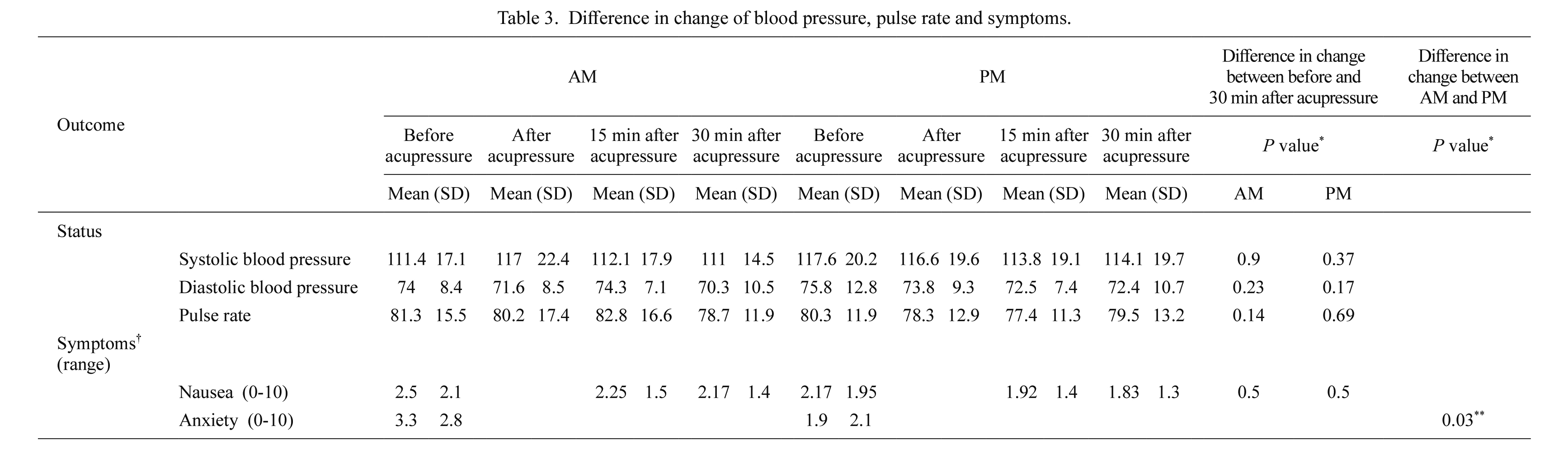
Difference in change of blood pressure, pulse rate and symptoms.
*Wilcoxon signed-rank tests.
**p < 0.05.
†We evaluated these symptoms by Numerical Rating Scale ranged from 0 to 10. The data in the table show the mean and standard deviation.
Tables 2 and 3 show the changes in nausea and anxiety symptoms, before and after the acupressure intervention. The median Numerical Rating Scale (range) for nausea was 1.5 (1-8) at the time of participation in the study. We observed decreased nausea after acupressure in four patients (patients A, D, J and L in Table 2). But the difference was not significant (p = 0.5). The other eight patients had no change in nausea.
Regarding anxiety, the difference in scores between the AM and PM interventions was 1.4, and significantly lower than before acupressure (p = 0.03).
Seven patients reported a positive feeling. A day after the intervention, one patient said, “Nausea has reduced post the intervention.” A patient’s key person said, “As I was interested in pressing the acupressure points, I will push it.”
On the other hand, another patient said “Nausea is not different. It is not getting any better or worse.” None of the patients reported a negative feeling.
This study investigated the feasibility, safety, and efficacy of acupressure for cancer patients with nausea in the palliative care unit.
Acupressure intervention for terminal cancer patients was feasible. As there were no negative comments, the results suggested that the next treatment round could be conducted by extending the intervention periods. In connection with safety, we were concerned about the vagal reflex due to acupressure, but no one fainted. Decreases in blood pressure and pulse rates were observed, but may be the diurnal variation, timing or time of intervention. It was therefore negligible from a clinical standpoint.
On the contrary, there was no significant reduction in nausea. In all 12 patients, most of them have nausea caused by digestive tract pressure. Among the four patients with reduced nausea, the proportion of women was high, and we confirmed an anxiety reduction. In the other eight patients, we confirmed mild nausea at the time of participation. The four patients with reduced nausea may have had nausea caused by anxiety. In addition, since we performed acupressure directly in this study, the touching effect may have affected the reduction of anxiety. On the other hand, we assessed the patient’s condition using age, primary cancer site, palliative performance scale, and palliative prognosis index, but the association with reduction nausea was uncertain. Future studies may be able to verify the efficacy of acupressure enrolling patients with moderate nausea and without digestive tract pressure and extended intervention period, previous study (Wright 2005) had shown an improvement in nausea, although it had not used a proper measuring method and had not determined the timing of symptom evaluation. Therefore, the present study evaluated symptoms using Edmonton Symptom Assessment System revised Japanese version scale at the time of validity evaluation as advised by the physician (S.T.) specializing in Oriental medicine. There were few patients with improved nausea probably because: 1) their nausea was caused by digestive tract pressure; 2) they initially suffered from mild nausea; 3) the intervention period was short; 4) they did not make use of the band. Regarding 1) and 2), it is necessary to choose patients without digestive tract pressure and with moderate nausea (for example, nausea ≧ 5). Regarding 3) and 4), it is necessary to extend the intervention period and consider the use of the acupressure band.
Several limitations of this study need to be acknowledged. First, this study included only 12 cases. We need to conduct a study with more patients to verify the safety and efficacy of acupressure. Second, in this study acupressure intervention was conducted without using a wristband to adjust pressure strength. Consequently, the acupressure’s direct touching effect may have led to reduced nausea. Third, the intervention period was set to one day to investigate its feasibility. It is necessary to extend the intervention period and evaluate its safety in the long term. Fourth, the symptom evaluation may have been affected because the acupressure practitioner and the symptom evaluator were the same. Finally, the results of this study should not be generalized, because it was a single-center intervention and was intended only for patients hospitalized in the palliative care unit.
We investigated the feasibility, safety, and efficacy of the acupressure intervention for cancer patients admitted in the palliative care unit. Although the sample size was small, we demonstrated the feasibility and the safety of acupressure treatment. On the other hand, there were no significant differences in nausea symptom before and after acupressure intervention.
We express gratitude and respect to the patients and staffs who participated in our study. Our gratitude also goes to Jun Kako for his helpful advice on the study protocol.
The authors declare no conflict of interest.