2021 Volume 255 Issue 3 Pages 267-273
2021 Volume 255 Issue 3 Pages 267-273
The aim of this study was to evaluate the admission chest and abdominal computed tomography (CT) findings of patients who presented to the emergency department with complaints of abdominal pain, fever, and shortness of breath and who had RT-PCR-confirmed COVID-19 infection. Seventy-five patients with RT-PCR-confirmed (in laboratory) COVID-19 infection who underwent chest and abdominal CT were included in the study. The radiological scales [the COVID-19 Reporting and Data System (CO-RADS) and severity score] of the chest and abdominal findings were examined on CT images. Forty-one (54.7%) patients were male and 34 (45.3%) were female. The mean age of the patients was 63.03 (range 24-89) years. The most frequently calculated CO-RADS score was found to be 5 (n = 53, 70.7%). Bilateral (72.0%) and multibolar (74.7%) involvement, peripheral (72.0%) and posterior (60.0%) distribution, and ground-glass opacity (66.7%) pattern were the most common pulmonary findings. A positive correlation was observed between CO-RADS and total severty score (p < 0.001). All patients were hospitalized. One (1.3%) patient was surgically treated because of acute appendicitis. Nine (12.0%) patients were admitted to the intensive care unit. Six (8.0%) patients died in the intensive care unit. Patients presenting to the emergency department with both abdominal and respiratory complaints during the pandemic should be evaluated for COVID-19. Patients can be diagnosed early with the data collected from CT without waiting for the PCR result. Hospital staff can take the necessary protective measures against virus transmission early, minimizing the in-hospital transmission of the virus.
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease emerged in the last month of 2019 and was declared a pandemic by WHO on March 11, 2020 (World Health Organization 2020). Even though more than a year has passed since the pandemic, our knowledge of the virus and the diseases caused by SARS-CoV-2 is still inadequate. Patients often present with fever, respiratory symptoms, and myalgia. However, the presenting symptoms may also include atypical gastrointestinal complaints (abdominal pain, nausea, vomiting, diarrhea, etc.) (Amaravathi et al. 2021).
The gold standard diagnostic method for COVID-19 infection is reverse transcription-polymerase chain reaction (RT-PCR). Although not routinely recommended, chest computed tomography (CT) can be used for the diagnosis in cases of false-negative RT-PCR results. Chest CT is useful not only for diagnosis but also for evaluation of the disease progression and response to treatment (American College of Radiology 2020).
In Turkey, as in the entire world, it is aimed to use the healthcare system efficiently and rationally during the pandemic. However, the delay in getting RT-PCR test results in the emergency department affects the patient dynamics. Early diagnosis of patients is of importance both in planning early and effective treatment and minimizing virus transmission to hospital staff. At the same time, rational use of limited resources can be achieved by predicting the intensive care requirement of patients who are scheduled for conservative treatment or surgery.
The aim of this study was to evaluate the chest and abdominal CT findings on admission in patients who presented to the emergency department with complaints of abdominal pain, fever, and shortness of breath and who had RT-PCR-confirmed COVID-19 infection.
This was conducted as a single center, cohort study at our City Hospital. Prior to this study, approval was obtained from our local Ethics Committee (2021/514/201/5) and the Ministry of Health Scientific Research Platform. It was in accordance with the revised declaration of Helsinki. Written informed consent collected from the participiants.
Patients who presented to the emergency department of our hospital with complaints of abdominal pain, fever, and shortness of breath between December 2020 and April 2021 were evaluated. Among these patients, 75 patients with RT-PCR -confirmed (in laboratory) COVID-19 infection who underwent chest and abdominal CT were included in the study. Those with malignant diseases were not included. The patients’ requirements for surgical treatment, admission to the intensive care unit (ICU), intubation, length of stay in the intensive care unit, and mortality were analyzed.
CT TechniqueAll chest CT examinations for the screening of SARS-CoV-2 pneumonia were performed with one scanner (128 section Philips ingenuity) without the use of contrast material. Scans were obtained in the supine position on normal breathing. CT examinations for the screening of abdomen were performed with one scanner (128 section Philips ingenuity) with the use of contrast material in portal venous phase. The main scanning protocol was as follows: tube voltage, 120 kVp; tube current modulation, 120 mA-380 mA; detector configuration, 64 × 0.625 mm or 16 × 0.625 mm; rotation time, 0.5-0.7 s; slice thickness, 5 mm; and pitch, 0.984. Reconstruction kernel was done with a thickness and an interval of 0.625 mm in lung.
Chest CT EvaluationThe images were interpreted using the lung window setting. The CT images were assessed, following a standardized protocol, for the presence and distribution of the following abnormalities: (a) ground-glass opacities (GGO) defined as hazy areas of increased attenuation without obscuration of the underlying vascular markings; (b) nodules (centrilobular, perilymphatic, or random in distribution); (c) linear densities (interlobular septal thickening, intralobular septal line, or parenchymal bands); (d) crazy paving; (e) consolidations (parenchymal opacities obscuring underlying vessels); (f) architectural distortion, or traction bronchiectasis; (g) pleural effusion; (h) lymphadenopathy (defined as lymph node with a short-axis dimension of > 1.0 cm); (i) air bronchogram; (j) tree-in-bud sign (defined as multiple areas of centrilobular nodules with a linear branching pattern); and (k) white lung.
The overall anatomic distribution (subsegmental, segmental, lobar), zonal predominance (upper, middle, lower lung; central, middle, or peripheral location), and extent (focal, multifocal, and diffuse) of the lesions were also recorded.
The standardized reporting system for suspected patients of COVID-19 infection is named as CO-RADS which was developed by Dutch Radiological Society for moderate to high prevalence setting. CO-RADS scoring is based on CT images. The severity or level of suspicion of the infection is listed from very low or CO-RADS 1 up to very high or CO-RADS 5. Two additional classifications, respectively, describe a technically inadequate examination (CO-RADS 0) and SARS-CoV-2 infection as proven by positive RT-PCR at the time of examination (CO-RADS 6) (Table 1) (Palmer 2020).
Each of the five lung lobes was assessed for degree of involvement. Severity score is by scoring the percentages of each of the five lobes that is involved:
1. < 5% involvement
2. 5%-25% involvement
3. 26%-49% involvement
4. 50%-75% involvement
5. > 75% involvement.
The total CT score is the sum of the individual lobar scores and can range from 0 (no involvement) to 25 (maximum involvement), when all the five lobes show more than 75% involvement.

Scales of COVID-19 Reporting and Data System (CO-RADS) and the corresponding level of suspicion for pulmonary involvement in COVID-19.
Adapted from Palmer (2020).
Acute abdomen findings were evaluated. Variables of acute appendicitis, mesenteric ischemia, mesenteric paniculitis, diverticulitis, acute cholecystitis, cholelithiasis, acute pancreatitis and acute pyelonephritis were recorded.
Statistical analysisIBM® SPSS® (Statistical Package for the Social Sciences) Statistics version 23 were used for the analyzing tool, thus demographic characteristics and collected data of patients were entered to this tool. All values are expressed as mean, maximum, and minimum; percentage values were used for qualitative variables. Normal distributions were reported as mean ± SD. For correlation analysis between CT scores, Pearson correlation coefficient (r) was used, assuming the data was normally distributed. If the correlation coefficient was positive, there was a positive relationship between the two variables. The level of statistical significance was set at p < 0.05.
Forty-one (54.7%) patients were male and 34 (45.3%) were female. The mean age of the patients was 63.03 (range 24-89) years.
Chest CT parenchymal findings and CO-RADS scores are shown in Table 2. The most frequently calculated CO-RADS score was found to be 5 (n = 53, 70.7%). This was followed by CO-RADS scores of 3 (n = 12, 16.0%). Bilateral (72.0%) and multibolar (74.7%) involvement, peripheral (72.0%) and posterior (60.0%) distribution, and GGO (66.7%) pattern were the most common pulmonary findings. Twenty-six (34.7%) patients had a rounded GGO/consolidation pattern. Regarding total severity score (TSS), the right lung mean severity score was 4.65 (range 2-15), the left lung mean severity score was 4.02 (range 0-10), and the mean TSS was 8. A positive correlation was observed between CO-RADS and TSS (p < 0.001) (Fig. 1).
Abdominal CT detected acute appendicitis in 1 (1.3%) (Fig. 2), diverticulitis in 1 (1.3%) (Fig. 3), mesenteric panniculitis in 2 (2.7%), acute cholecystitis in 6 (8.0%) (Fig. 4), cholelithiasis in 14 (18.7%), mesenteric ischemia in 20 (26.7%), acute pyelonephritis in 14 (18.7%), and acute pancreatitis in 2 (2.7%) patients (Table 3).
All patients were hospitalized. The mean hospital stay was 8.74 (range 2-37) days. Conservative medical treatment was applied to 65 (86.7%) patients in the hospital. One (1.3%) patient was surgically treated because of acute appendicitis. Nine (12.0%) patients were admitted to the intensive care unit, and 3 (4%) patients were intubated. Six (8.0%) patients died in the intensive care unit (Table 4).
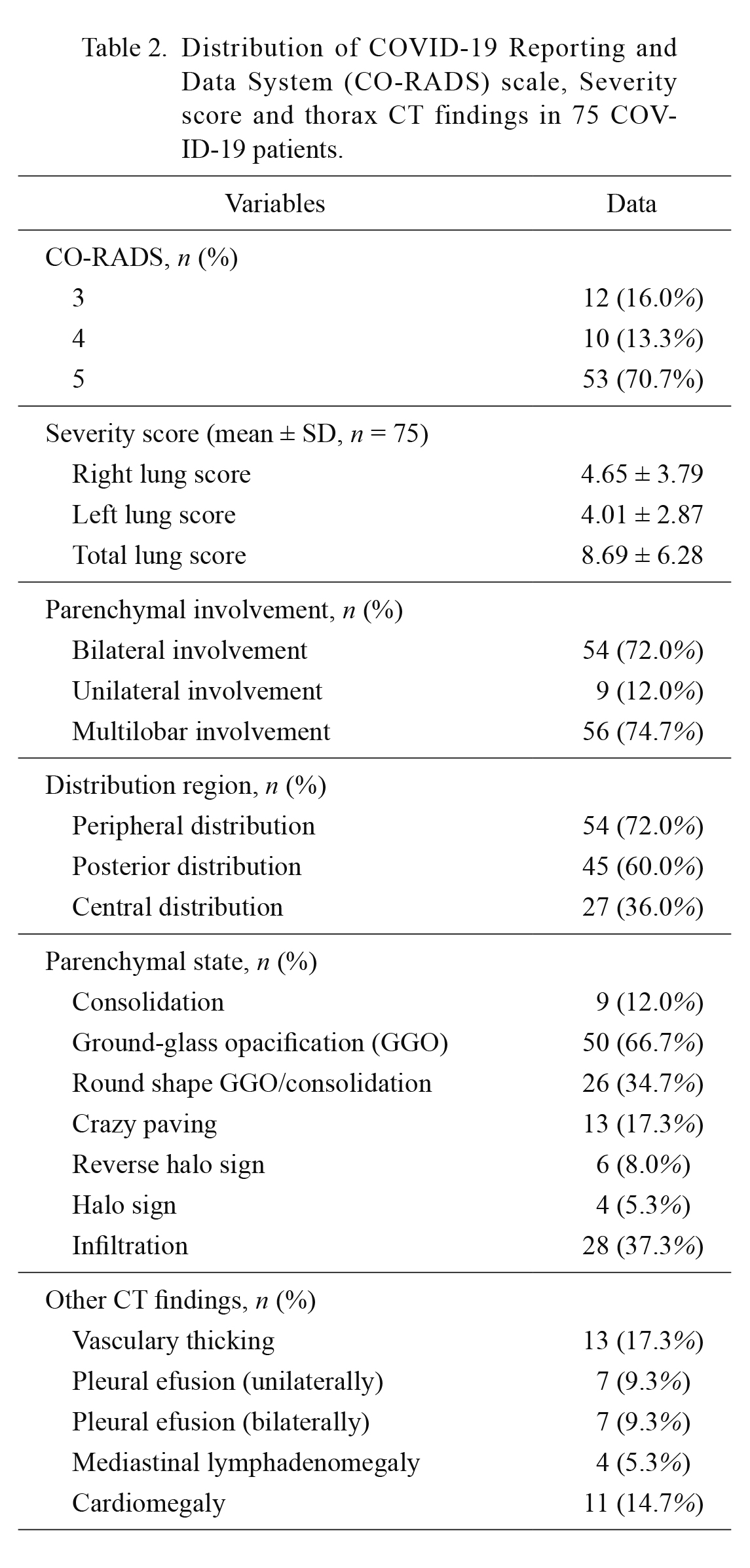
Distribution of COVID-19 Reporting and Data System (CO-RADS) scale, Severity score and thorax CT findings in 75 COVID-19 patients.
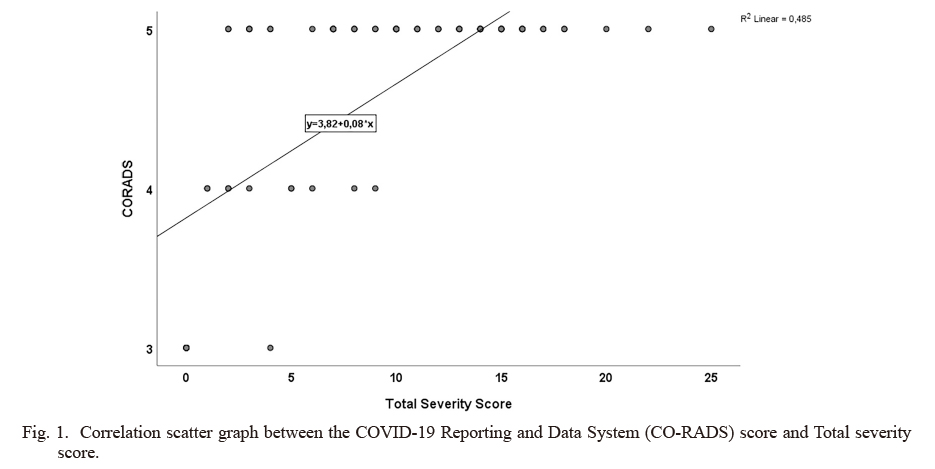
Correlation scatter graph between the COVID-19 Reporting and Data System (CO-RADS) score and Total severity score.

Chest and abdominal CT images of a thirty-one-year-old man.
A. There are ground glass opacities in the left lower lobe; ground glass opacities, interlobules septal thicking periferally in the right lower lobe, with CO-RADS 5 and a Total severity score of 4. B. There is acute appendicitis findings at abdominal CT; appendiceal dilatation, wall thickening and periappendiceal inflammation (white arrow).
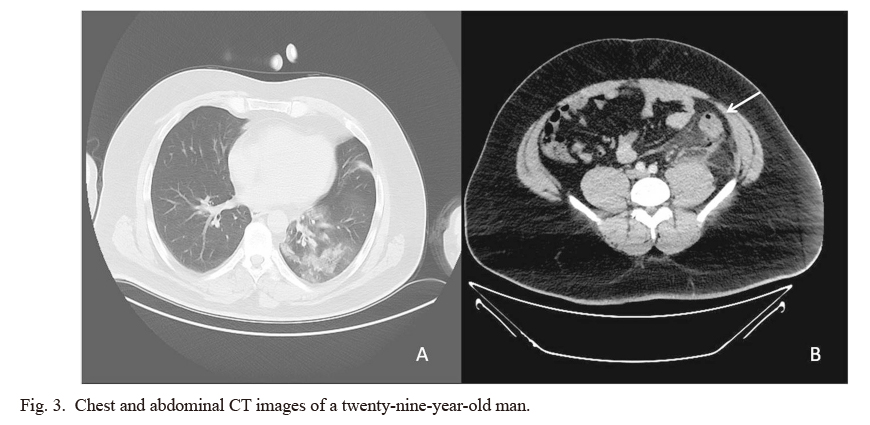
Chest and abdominal CT images of a twenty-nine-year-old man.
A. Unilateral diffuse consolidation and ground glass opacities in the left lower lobe, with CO-RADS 3 and a Total severity score of 3. B. There is colonic diverticulitis findings at abdominal CT; segmental thickening of descending colon wall, pericolic stranding and enhancement of colonic wall (white arrow).
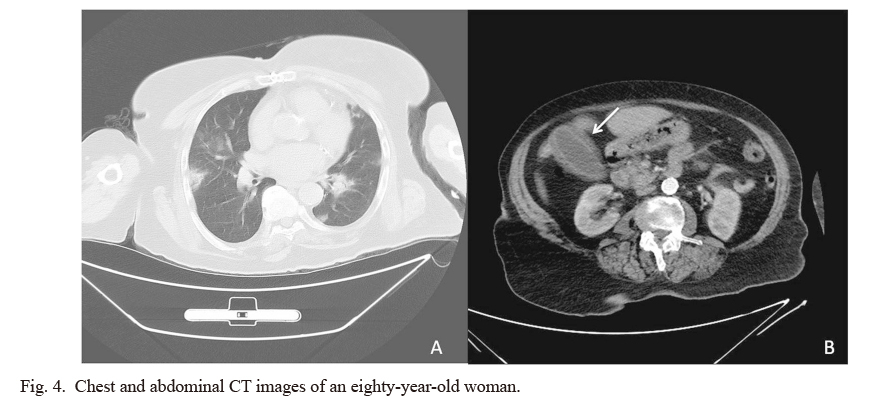
Chest and abdominal CT images of an eighty-year-old woman.
A. Bilateral patchy consolidation and ground glass opacities more pronounced in the lower lobes, peripherally and centrally, with CO-RADS 5 and a Total severity score of 8. B. There is acute cholesistitis findings at abdominal CT; distended gallbladder with wall thickening, mucosal enhancement and pericholecystic fluid and inflammatory fat stranding (white arrow).
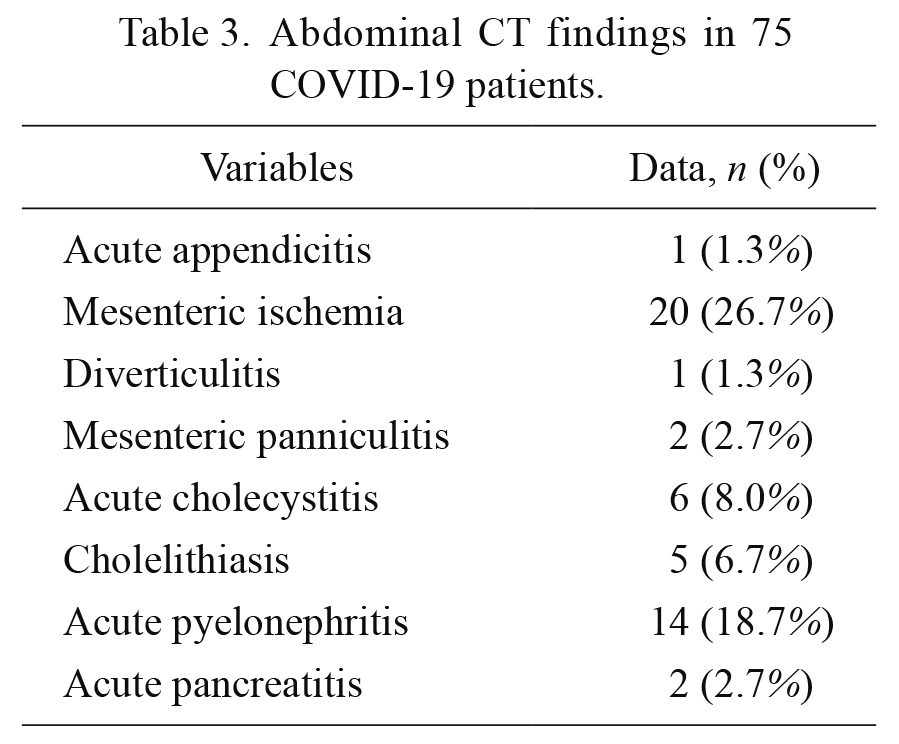
Abdominal CT findings in 75 COVID-19 patients.
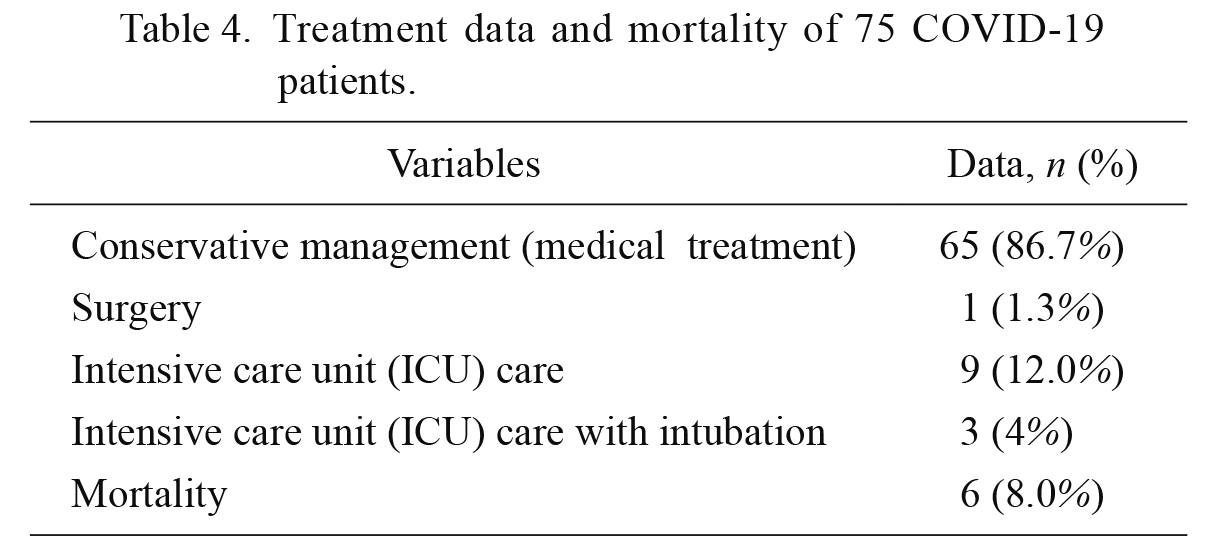
Treatment data and mortality of 75 COVID-19 patients.
Due to the highly contagious nature of SARS-CoV-2, early diagnosis and treatment are important in the management of patients. Otherwise, the spread of the disease poses a serious threat to public health (Seyhan et al. 2021).
COVID-19 symptoms are often of respiratory origin. Patients may have a clinical course ranging from mild non-pneumonic disease to severe respiratory failure (Acute respiratory distress syndrome and multiorgan failure) (Wang et al. 2020; Salehi et al. 2020). However, gastrointestinal symptoms such as nausea, vomiting, abdominal pain, and diarrhea may also be seen (Tian et al. 2020; Xiao et al. 2020; Behzad et al. 2020). Patients may manifest respiratory and digestive symptoms simultaneously or individually. However, the predominant presenting symptoms may cause other symptoms to be overlooked. Therefore, it may be necessary to question additional respiratory complaints for the differential diagnosis of potential COVID-19 in patients presenting to the emergency department with abdominal pain during the pandemic (Keshavarz et al. 2021). All of the patients included in our study also had complaints of fever and shortness of breath accompanying abdominal pain.
Nucleic acid tests are the gold standard method for the diagnosis of SARS-CoV-2 infection (Jin et al. 2020). However, these tests have a high rate of false-negative results (20-40%) (Ai et al. 2020). Some researchers have reported that chest CT is more sensitive than the RT-PCR test (Ai et al. 2020; Fang et al. 2020; Li and Xia 2020).
A prospective analysis of 1,014 patients found the sensitivity of CT as 97% and the sensitivity of RT-PCR as 60-70% for the diagnosis of COVID-19 (Ai et al. 2020). False negativity of the PCR test and high sensitivity of chest CT have made chest CT come to the fore for the diagnosis of patients who present to the emergency department (Arslan et al. 2021). In our study, chest CT was ordered in addition to abdominal CT for 75 patients due to the presence of shortness of breath, fever symptoms accompanying abdominal pain during the pandemic.
CO-RADS was developed in the early period of COVID-19 by the Dutch Radiological Society as a classification system to assess the suspected lung involvement in COVID-19 on chest CT, and to provide easy and standardized communication (Palmer 2020). Salehi et al. (2020) supported that the CO-RADS facilitated the diagnosis and management of COVID-19 patients. We also performed a CO-RADS assessment for our patients. Of the patients, 53 (70.7%) were classified as CO-RADS 5, and 10 (13.3%) as CO-RADS 4. Twelve (16.0 %) patients were evaluated as CO-RADS 3 (suspicious group for COVID-19). RT-PCR results obtained after 24 hours were positive in 75 of our patients (CO-RADS 6).
The TSS is a radiological scoring system that evaluates the severity of lung involvement and predicts prognosis in COVID-19 patients (Francone et al. 2020). Yang et al. (2020) reported that TSS could be used to rapidly identify patients with COVID-19. They showed that TSS increased as the severity of the disease increased. Moreover, they found that the mean right lung severity score (SS) was 6, the mean left lung SS was 6, and the TSS was 13 in mild infection, while in severe infection, the mean right lung SS was 6, the mean left lung SS was 6, and the TSS was 13 (Yang et al. 2020). In our study, our patients had a mean right lung SS of 4.65, a mean left lung SS of 4.01, and a mean TSS of 8.69. Based on our results, there was a significant positive correlation between CO-RADS and TSS (p < 0.001). This correlation supports the relevance of the two radiological scales in clinical practice.
There are studies showing gastrointestinal symptoms more frequently in critically ill patients (Tian et al. 2020; Pan et al. 2020). Many gastrointestinal diseases such as ileus, diffuse hepatic necrosis, acute acalculous cholecystitis, and intestinal ischemia have been observed in COVID-19 patients admitted to the ICU (Kaafarani et al. 2020). Xiao et al. (2020) reported acute calculous cholecystitis in four patients (4%) and acute pancreatitis in one patient (1%) during their stay in the ICU. In our study, 20 (26.7%) patients had mesenteric ischemia, 6 (8.0%) patients had acute cholecystitis, and 2 (2.7%) patients had acute pancreatitis at the time of admission.
In patients undergoing surgery, an early systemic inflammatory response is triggered, impairing the immune system. Therefore, surgeries performed during the incubation period of COVID-19 may exacerbate the course of the disease (Amodeo et al. 2018). Lei et al. (2020) also stated that surgery accelerated and exacerbated the progression of the COVID-19 disease. A contrast-enhanced abdominopelvic CT scan is recommended in any case of COVID-19 with gastrointestinal signs and symptoms (Azouz et al. 2020). Because CT scan leads the surgeon to a medical treatment approach rather than surgery. A positive result can be achieved by administering conservative treatment to the patient (Gartland and Velmahos 2020). In our study, only 1 (1.3%) patient was operated for acute appendicitis. Conservative medical treatment was administered to 65 (86.7%) patients. Nine (12.0%) patients were admitted to the ICU. Six (8.0%) patients died.
In conclusion, patients presenting to the emergency department with both abdominal and respiratory complaints during the pandemic should be evaluated for COVID-19. Patients can be diagnosed early with the data collected from CT without waiting for the PCR result. Thus, appropriate treatment is planned for the patient, and morbidity and mortality can be reduced. The severity and prognosis of the disease are predicted in line with the radiological scales (CO-RADS and TSS), ensuring the optimal use of limited intensive care resources. Hospital staff can take the necessary protective measures against virus transmission early, minimizing the in-hospital transmission of the virus.
We thank the health care workers on the front lines of the current pandemic.
The authors declare no conflict of interest.