2022 年 256 巻 1 号 p. 43-52
2022 年 256 巻 1 号 p. 43-52
The number of elderly patients with hepatocellular carcinoma (HCC) has been increasing, but it remains unclear whether hepatectomy can be performed using the same criteria as in younger patients. Furthermore, the appropriate preoperative evaluation for hepatectomy in elderly patients is not yet clearly defined. Here, we investigated the applicability of preoperative assessment using the Controlling Nutritional Status (CONUT) score to help improve hepatectomy outcomes in elderly patients with HCC. This was a single-center retrospective analysis, and the study population comprised 64 consecutive patients who underwent hepatectomy for HCC between January 2012 and August 2016. We compared the preoperative assessment and perioperative outcomes between elderly (≥ 75 years old) and younger (< 75 years old) patients. A total of 61 patients were reviewed. Poor preoperative CONUT score was associated with a longer postoperative hospital stay in elderly patients undergoing hepatectomy for HCC. In addition, although elderly patients had similar perioperative outcomes to younger patients, the incidence of delirium was significantly higher, and univariate analysis confirmed that old age is a risk factor for delirium among the preoperative factors. Hepatectomy for HCC in the elderly can be safely performed with appropriate preoperative nutritional assessment using CONUT score and prevention of postoperative delirium. Preoperative nutritional assessment using the CONUT score was useful in predicting prolonged hospitalization for elderly hepatectomy with HCC.
The aging of the global population is continuously progressing, and appropriate cancer treatment for the elderly is becoming increasingly important. Primary liver cancer was the sixth most commonly diagnosed cancer and the third leading cause of death from cancer in 2020 worldwide, approximately 80% of which were hepatocellular carcinoma (HCC) (Sung et al. 2021). The number of elderly patients with HCC is expected to further increase in the future. Percutaneous therapies, such as microwave coagulation and radiofrequency ablation (RFA) for HCC in the elderly, are minimally invasive and can be easily performed compared to surgery (Yamazaki et al. 2014). In contrast, hepatectomy in the elderly is considered high-risk because of the high incidence of postoperative complications (Zhou et al. 2013). However, due to the development of advanced surgical techniques such as laparoscopic hepatectomy (LH) and better perioperative management using the enhanced recovery after surgery (ERAS) protocol, hepatectomy has been increasingly performed in the elderly (Kaibori et al. 2019a). The elderly is generally known to undergo age-related declines in cardiopulmonary function and metabolism, as well as develop multiple underlying medical comorbidities. In addition, it is said that the elderly is more likely to develop consciousness disorder accompanied by psychiatric symptoms, so-called postoperative delirium (POD), due to the upset physical condition after surgery. Symptoms of POD include various problematic behaviors, such as removal of catheters and intravenous lines by the patient, difficulty in maintaining rest, and disturbed sleep-wake cycle, resulting in longer hospital stays, additional nursing care, and greater medical costs (Park et al. 2017). Therefore, it is unclear whether they can be operated on using the same criteria as those applied in younger patients.
The preoperative nutritional status of the elderly has a significant impact on postoperative recovery (Borloni et al. 2019). Nutritional status varies greatly in patients, and careful assessment of preoperative nutritional status is essential. The Controlling Nutritional Status (CONUT) score has been developed as a nutritional screening tool calculated using measurements of serum albumin concentration, total peripheral lymphocyte count, and total cholesterol concentration (Ignacio de Ulibarri et al. 2005). In this scoring system, the level of malnutrition is classified into four levels: normal, mild, moderate, and severe; the higher the score, the more severe the malnutrition is. Due to the accessibility of obtaining these laboratory parameters, the CONUT score is convenient and easy to use for determining the nutritional status of patients. Recently, the CONUT score has been reported to be associated with postoperative complications, hepatic functional reserve, overall survival (OS), and recurrence free survival (RFS) following hepatectomy (Harimoto et al. 2017, 2018; Takagi et al. 2017, 2019a, b); however, there have been few reports using CONUT with a focus on liver resection in the elderly. Therefore, we investigated whether hepatectomy for HCC can be performed safely in elderly patients compared with younger patients, and how preoperative assessment of nutritional status using the CONUT score affects the short-term and long-term outcomes of hepatectomy in elderly patients.
The present study was approved by the Institutional Review Board of Iwate Prefectural Central Hospital (No. 617) and performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Furthermore, the need for informed consent was waived because of the retrospective nature of the study. We reviewed 64 consecutive patients who underwent hepatectomy, excluding 55 patients who underwent RFA, out of 119 HCC patients at Iwate Prefectural Central Hospital between January 2012 and April 2016.
SubjectsElderly patients were defined as those aged 75 years and above, and younger patients were defined as those aged less than 75 years; according to these, patients were classified into elderly and younger groups. The diagnosis of HCC was confirmed by histological examination after hepatectomy. Patient characteristics and perioperative data were extracted from clinical records and laboratory reports. In addition, the length of postoperative hospital stay and the 1- and 2-year OS and RFS were examined. The preoperative condition was evaluated using the American Society of Anesthesiologists (ASA) physical status classification system (Mak et al. 2002). The indications for hepatectomy were evaluated according to the extent of the tumor progression, liver function, and general condition of the patients. As long as the patient is in good general condition and can walk, there were no restrictions on surgery based on age. In our hospital, patients with an ASA 4 or more were considered contraindicated for hepatectomy except for emergency surgery. For hepatectomy for HCC, anatomic resection was performed as indicated. For non-anatomic partial resection, LH was performed where possible. Major hepatectomy was defined as the resection of four or more liver segments, while minor hepatectomy was defined as the resection of less than four liver segments. Perioperative management of patients undergoing hepatectomy was based on the clinical pathway provided in the modified ERAS protocols in hepatectomy for HCC (Fujio et al. 2020). POD was diagnosed by intensive care unit (ICU) nurses using the Intensive Care Delirium Screening Checklist (ICDSC) (Bergeron et al. 2001), which is a widely used diagnostic algorithm for the identification of delirium and has been shown to have a high sensitivity and specificity. The abdominal drain was withdrawn on postoperative day 2 or 3 if no bile leakage was observed. The criteria for discharge were in accordance with our ERAS protocol (Fujio et al. 2020). The Clavien-Dindo classification was used to classify postoperative complications. Grade III or higher complications were considered severe.
Preoperative blood samples were obtained within 1 week before the hepatectomy. Preoperative CONUT score was calculated based on serum albumin concentration, total peripheral lymphocyte count, and total cholesterol concentration for nutritional assessment (Ignacio de Ulibarri et al. 2005). An investigation of the cut-off value for the CONUT score using the receiver operating characteristic (ROC) curve showed that the most appropriate cut-off value for the CONUT score was 3 (AUC = 0.621, P = 0.038, sensitivity = 0.804, specificity = 0.412). Therefore, we set 3 as the cut-off value for the CONUT score in this study and classified the patients into high and low CONUT groups.
Statistical analysisContinuous data are expressed as the mean and standard deviation. The differences between the elderly and younger groups were analyzed using the Student’s t-test. Fisher’s exact test or chi-square test was used for categorical variables. Univariate analysis was performed using a logistic regression model. The OS and RFS rates were estimated using the Kaplan-Meier method. All analyses were performed using the JMP® Pro 15 software program (SAS Institute Inc., Cary, NC, USA). Differences were considered statistically significant at P < 0.05.
A total of 64 consecutive patients were retrospectively reviewed, and 3 patients were excluded due to emergency surgery for ruptured HCC. Thus, a total of 61 patients were included in the analysis; 22 patients (36.1%) were 75 years or older, and 39 patients (63.9%) were aged < 75 years. The preoperative characteristics of the elderly and younger patients are summarized in Table 1. The mean ages of patients in the elderly and younger groups were 78.2 ± 2.9 and 66.0 ± 6.3 years old, respectively. The proportion of patients with hypertension as a comorbidity was about 1.5 times higher in the elderly than in the younger group, but the difference was not statistically significant. Other variables, including sex, Child-Pugh score, body mass index, preoperative biochemical values, and CONUT score, were not significantly different between the two groups.
Perioperative and postoperative outcomes are summarized in Table 2. The mean amount of blood loss and transfusion frequency were higher in the elderly group, although this difference was not statistically significant. The types of liver resection and the proportion of LH were similar between the two groups. Pathological factors, including tumor size, showed no marked differences between the two groups. POD was twice as common in elderly patients as in younger patients, with a statistically significant difference (P = 0.009). Complications other than delirium, including severe ones, were more common in the elderly, but this difference was not statistically significant. The length of hospital stay was similar between the groups.
Table 3 summarizes the incidence and risk factors of POD. POD was observed in more than half of the elderly patients, but there was no difference in sex, Child-Pugh score, preoperative CONUT score, or surgical procedure. Patients with POD had a larger tumor size, more blood loss, and longer operative time as perioperative factors. In addition, they had a significantly longer interval before they left the ICU (P = 0.027), started walking (P = 0.040), and started oral feeding (P = 0.017). They also had a longer abdominal drain insertion period (P = 0.031). As a result, patients with POD had a significantly longer hospital stay (P = 0.015). Severe complications tended to be more common, but the differences were not statistically significant. Risk factors for POD as identified by univariate analysis were being in the elderly group, increased blood loss, longer operative time, and larger tumor size. In addition, increased blood loss, longer operation time and larger tumor size were positively correlated, although there was no correlation between them and being elderly.
Next, we investigated how the preoperative CONUT score for hepatectomy in HCC affected postoperative outcomes. The outcomes of the two groups are summarized in Table 4. In all cases, 42 patients (68.9%) belonged to the low CONUT group, and 19 patients (31.1%) belonged to the high CONUT group. In the high CONUT group, the tumor sizes were significantly larger (P = 0.038), and a significantly higher number of patients were classified as Child-Pugh B (P = 0.005). In addition, a larger amount of intraoperative bleeding was observed in the high CONUT group, but no statistically significant difference was observed. There were no significant differences in other factors between the two groups. Furthermore, we examined the preoperative CONUT score and perioperative factors in the elderly and younger groups. In both groups, the group with a higher CONUT score tended to have more intraoperative bleeding. Interestingly, the group with a high CONUT score had a significantly longer hospital stay among the elderly group (P = 0.042), but no significant difference was observed in the younger group.
After a median follow-up of 1,503 days, 11 young and 7 elderly patients died. Of the 18 deaths, three had no known cause of death. Among the young, 4 died of cancer progression, 3 of liver failure, and 2 of other reasons; meanwhile, in the elderly, 1 died of cancer progression, 3 of liver failure, and 2 of other reasons. There were no statistically significant differences in the causes of death between the groups. The 1- and 2-year OS rates (Fig. 1a) were 81.8% and 81.8%, respectively, in the elderly group and 86.8% and 84.2%, respectively, in the younger group. We also investigated whether there was a difference in survival rates between the elderly and younger groups depending on the preoperative CONUT score. The 1- and 2-year OS rates were slightly worse in both groups with higher preoperative CONUT scores, but the difference was not statistically significant (Fig. 1b, c). Additionally, the 1- and 2-year RFS rates were similar between the elderly and younger groups (Fig. 2a). In both groups, RFS was worse in the high CONUT group, and this trend was more pronounced in younger patients but was not statistically significant (Fig. 2b, c).

The preoperative characteristics of elderly and younger patients who underwent hepatectomy for hepatocellular carcinoma.
Continuous data are presented as mean and standard deviation, and categorical data are presented as numbers (%).
*significant difference
HBV, hepatitis B virus; HCV, hepatitis C virus: NBC, non-hepatitis B or C virus; ASA-PS, American Society of Anesthesiologists physical status; ICGR15, indocyanine green retention rate after 15 min; CONUT, Controlling Nutrition Status.
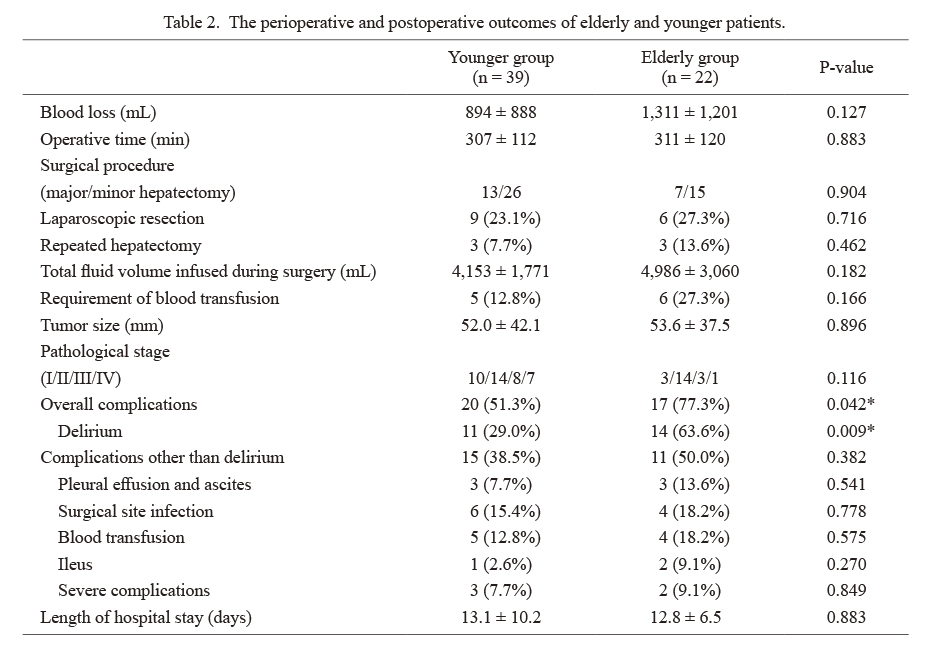
The perioperative and postoperative outcomes of elderly and younger patients.
Continuous data are presented as mean and standard deviation, and categorical data are presented as numbers (%).
*significant difference

The preoperative and perioperative characteristics and outcomes of delirium and non-delirium patients (a) and risk factors for delirium according to univariate logistic regression analyses (b).
Continuous data are presented as mean and standard deviation, and categorical data are presented as numbers (%).
*significant difference
ASA-PS, American Society of Anesthesiologists physical status; CONUT, Controlling Nutrition Status; CI, confidence interval.

The perioperative characteristics and outcomes of high and low CONUT patients. (a) All cases, (b) elderly patients, and (c) younger patients.
Continuous data are presented as mean and standard deviation, and categorical data are presented as numbers (%).
*significant difference
CONUT, Controlling Nutrition Status; HBV, hepatitis B virus; HCV, hepatitis C virus: NBC, non-hepatitis B or C virus; ASA-PS, American Society of Anesthesiologists physical status; ICGR15, indocyanine green retention rate after 15 min.

The overall survival curves after hepatectomy.
(a) Comparison of survival outcomes after hepatectomy between younger and elderly patients. The bold line indicates the overall survival curve of the younger patients. The dotted line indicates the overall survival curve of elderly patients. (b), (c) Comparison of survival outcomes after hepatectomy between high CONUT group and low CONUT group in (b) younger and (c) elderly patients. The bold line indicates the overall survival curve of the high CONUT patients while the dotted line indicates the overall survival curve of the low CONUT patients
CONUT, Controlling Nutrition Status; OS, overall survival.

The recurrence free survival curves after hepatectomy.
(a) Comparison of survival outcomes after hepatectomy between younger and elderly patients. The bold line indicates the recurrence free survival curve of the younger patients. The dotted line indicates the recurrence free survival curve of elderly patients. (b), (c) Comparison of recurrence free outcomes after hepatectomy between high CONUT group and low CONUT group in (b) younger and (c) elderly patients. The bold line indicates the recurrence free survival curve of the high CONUT patients, while the dotted line indicates the recurrence free survival curve of the low CONUT patients
CONUT, Controlling Nutrition Status; RFS, recurrence free survival.
Primary liver cancer is the fifth leading cause of death in Japan, accounting for more than 90% of HCC cases. In addition, the number of elderly patients undergoing hepatectomy for HCC is also increasing (Kudo et al. 2020). In a nationwide survey conducted from 2000 to 2007 in Japan, there were 2,020 patients (16.0%) aged 75 years or older among a total of 12,587 HCC patients who underwent hepatectomy (Kaibori et al. 2019b). In general, age-related decline occurs in many organ systems. The liver, which synthesizes albumin and prothrombin, gradually loses its ability to do so as it ages. The blood volume in the liver also declines with age (Kaibori et al. 2009). However, it is notable that liver regeneration is maintained in the elderly and remains similar to that in younger patients (Jansen 2002). Therefore, it is extremely important to identify trends in elderly patients with HCC and to evaluate the indications and limitations of surgical treatment. This study showed that age is not a risk factor for short- and long-term outcomes after hepatectomy if the patients are in good general conditions. We also demonstrated that preoperative nutritional assessment using the CONUT score is useful in determining the prolongation of hospital stay after hepatectomy in elderly patients with HCC.
CONUT score is a useful and simple assessment of nutritional status as well as the prognostic nutritional index (PNI). However, the CONUT score showed a better association than PNI with anthropometric values, accompanied by an association with severity of chronic liver disease (Taniguchi et al. 2013). Several reports have recently described the association between preoperative CONUT scores and outcomes in patients undergoing hepatectomy for HCC (Harimoto et al. 2017, 2018; Takagi et al. 2017, 2019a, b). Takagi et al. (2019a) reported that the preoperative CONUT score is associated with disease prognosis, hepatic functional reserve, and the incidence of major postoperative complications in patients with HCC. Although there was no significant difference in the 1- and 2-year OS and RFS rates, our results also showed that liver function was worse in patients with higher preoperative CONUT scores. We also demonstrated that higher preoperative CONUT scores were associated with more complications and significantly longer hospital stays in elderly patients. The biological mechanisms explaining the relationship between CONUT scores and short-term postoperative outcomes in the elderly are not well understood. The CONUT score reflects not only nutritional status but also immune function status (Wang et al. 2019). A high preoperative CONUT score indicates a low preoperative immune function, which may lead to a higher incidence of postoperative complications and a longer recovery time from hepatectomy and complications, which would increase the length of hospital stay. Calculating the CONUT score is simple and practical, making it an important tool for understanding nutritional disorders before hepatectomy. Branched-chain amino acids and late evening snacks are useful in improving the nutritional status of patients with liver disease (Maki et al. 2019). Therefore, our results suggest that elderly patients undergoing hepatectomy may benefit from preoperative immuno-nutritional support if available, which may improve preoperative CONUT score and lead to better short-term outcomes.
Our results showed that the risk factors for POD include intraoperative surgical stress, tumor size and being elderly, and there is a correlation between intraoperative stress and tumor size. Thus, a careful operation is warranted to prevent POD, especially when the tumor diameter is large. Interestingly, the only preoperative risk factor for the incidence of POD was being elderly. Several studies have reported delirium after hepatectomy, and old age is reported to be a risk factor (Yoshimura et al. 2004; Chen et al. 2015; Park et al. 2017), which is consistent with our results. Chen et al. (2015) reported that cholinergic deficiency and excessive dopaminergic activity are involved in the pathophysiologic mechanisms of delirium. In general, excessive anticholinergic effects lead to behavioral inhibition. As cholinergic transmission decreases with age, the elderly are more susceptible to anticholinergic effects. Dopamine, a neurotransmitter responsible for motor function, attention, and cognition, plays an important role in developing delirium. Some dopamine receptors also decrease with age, increasing the likelihood of delirium in elderly patients (Chen et al. 2015). Although the pathogenesis of POD is not well understood, these may be contributory reasons why elderly patients are more likely to develop POD. Recently, Janssen et al. (2020) reported that delirium is independently associated with increased 1-year mortality in elective abdominal surgery, which reiterates the importance of improving delirium prevention programs. To prevent delirium, we attempted to recover the preoperative state as soon as possible by resuming fluid and food intake early after surgery based on our ERAS protocol and advising the patients to avoid sleeping during the day. We reduced pain mainly by continuous administration of epidural anesthesia. Hokuto et al. (2020) reported that ramelteon, an agonist of the melatonin receptor, reduces the risk of POD after hepatectomy. Honda et al. (2020) also reported that ramelteon is feasible for preventing POD in elderly patients after gastrectomy. In the future, such drugs may be used to prevent delirium in elderly patients after hepatectomy.
Several limitations associated with the present study warrant mention. First, this was a retrospective analysis with limited sample size and a reliance on medical records. Not all elderly patients with HCC were evaluated since hepatologists may choose RFA instead of surgery as a treatment option because of the patient’s advanced age. Therefore, the study population and results of this study were limited to patients who underwent hepatectomy and were in good preoperative condition, which may have resulted in a selection bias. Second, there was no comparison between hepatectomy and other treatment methods, such as RFA, in this study. Therefore, the superiority of hepatectomy in elderly patients was not examined. RFA is minimally invasive compared to hepatectomy, and it has been reported that RFA performed in elderly patients had a survival rate comparable to that of younger patients (Yamazaki et al. 2014). In contrast, it has been reported that hepatectomy for a tumor diameter of 3 cm or less in elderly patients with HCC reduced the risk of recurrence and contributed to prolonged survival compared with RFA (Kaibori et al. 2019a). Considering these reports and the present study results, hepatectomy is considered a beneficial treatment for early-stage HCC in the elderly with an appropriate preoperative evaluation of the general condition and postoperative management of complications.
In conclusion, for the first time, our results showed that appropriate preoperative nutritional assessment using the CONUT score was useful in predicting prolonged hospitalization for elderly hepatectomy with HCC. In addition, these results also suggest that careful postoperative monitoring and early intervention are necessary for preventing POD in hepatectomy in elderly patients. In the future, a multicenter study including RFA and hepatectomy should be conducted to evaluate the usefulness of the CONUT score in elderly HCC.
The authors would like to thank Dr. Kazuaki Tokodai and Dr. Yohei Ozawa (Tohoku University Graduate School of Medicine) for engaging in helpful discussions during the writing of the manuscript.
Atsushi Fujio and Masahiro Usuda participated in the research design, performed the research, and wrote the paper. Other co-authors made a substantial contribution to the writing or revising of this manuscript. All authors read and approved the final manuscript.