2022 Volume 256 Issue 2 Pages 103-118
2022 Volume 256 Issue 2 Pages 103-118
Disaster endangers the nutritional health of children with resulting effects on their mental, physical, and social well-being. Adequate infant and young child feeding (IYCF) in disaster prevents malnutrition and save lives. Although much progress has been made in nutritional support in disaster, malnutrition among children is still evident. This scoping review study was conducted to identify gaps in child nutrition in disaster. Published articles (1946-2020) in PubMed were sought primarily and were assessed with some additional relevant articles. Overall, 103 articles were included in the scope of this review. Increased morbidity and mortality from malnutrition (macro- and micro-nutrient deficiencies), communicable diseases and mental health issues are nutritional effects of disaster. Pre-disaster malnutrition, food insecurity, living environments in shelters, poor breast-feeding practices, sociocultural factors, and organizational and administrative challenges strongly affect child nutrition in disaster. The efforts and collaboration of relief agencies resulted in the development of standardized guidelines and codes represented as the Sphere Project and Operational Guideline for IYCF in Emergency. This study recommends a well-coordinated and explicit approach that includes preparedness, advocacy, development/updating of policies, and education of children, family and relief aid workers on nutrition. Periodic nutritional assessment of children and nutritional support in disaster by designated IYCF authority are necessary. Education and participation of the general population are also important. Future assessments must examine food allergies in children and nutrition effects on child mental health in disaster.
Nutrition is necessary for daily living Provision of good nutrition for children is crucially important for supporting their physical, mental, and social development. Particularly often, disaster causes great damage, disruption, or loss of life, robbing individual of basic necessities of life and well-being. As one would expect, these events affect food security and nutrition by limiting food accessibility, affecting health services and disturbing the care structure within the society (Guha-Sapir and D’Aoust 2011; FAO, Food and Agriculture Organization 2015; Delbiso et al. 2017).
Food security entails food supply availability, accessibility, and utilization. It exists when all people, at all times, have physical, social and economic access to sufficient, safe, and nutritious food that meets their dietary needs and food preferences for an active and healthy life (FAO 1996; The Sphere Project 2011, 2018). Access to food and the maintenance of adequate nutrition are fundamentally important determinants of people’s survival in the aftermath of a disaster. Food security and nutrition interventions can determine nutrition and health status in the short term, and survival and well-being in the long term.
A disaster is the consequence of a hazard (natural or human-induced) and its exposure when striking a community with some degree of vulnerability and some degree of coping capacity (Egawa et al. 2018, 2020). Therefore, disaster of all forms not only exerts strong socioeconomic effects and threaten human health and well-being, but also disaster damage strongly affects the socioeconomic background. Disaster does not affect all segments of the population equally; some groups are more vulnerable to disaster than others, with the most deleterious effects exerted on children (Adhisivam et al. 2006; UNDRR, United Nations Office for Disaster Risk Reduction 2012; Gribble et al. 2019). This disproportionately severe damage is attributable to the disruption of usual family life and economic activities including sudden and forced temporary relocation and separation of family members occasioned by disaster. Furthermore, strength-advantages of older adults in struggling for survival, especially in cases where disaster response is not coordinated, make children the most vulnerable individuals in disaster. If children are consequently deprived of access to adequate nutritious food, that deprivation can have devastating effects on their growth and development, potentially compromising their health in later life.
Although considerable progress has been made since 1990 towards improving child nutrition worldwide, the progress is slow and insufficient to reach the World Health Assembly targets set for 2025 and the Sustainable Development Goals (SDGs) set for 2030 (UNIGME, United Nations Inter-Agency Group for Child Mortality Estimation 2018; UNICEF, United Nations International Children’s Emergency Fund 2019; FAO, IFAD, International Fund for Agricultural Development, UNICEF, WFP, World Food Programme and WHO, the World Health Organization 2020). Globally, 149.2 million children under 5 years old were stunted (low height for age) and 45.4 million children under five years old showed wasting (low weight for age) of which 13.6 million were severely wasted in 2020. The effects of COVID-19 are likely to exacerbate these figures further (UNICEF, WHO and World Bank Group 2021). UNOCHA , the United Nations Office for the Coordination of Humanitarian Affairs (2016) reported that approximately 60 million people were displaced from their homes during 2016, half of whom were children. The burden is particularly heavy in Africa, where conflict, political fragility, and drought are more prevalent (ADB, Africa Development Bank Group 2012; UNICEF 2019). UNICEF (2019) lamented that the greatest burden of malnutrition in all its forms is shouldered by children and adolescents from the poorest communities, irrespective of the country. Even in high-income countries, malnutrition still represents an important social problem, especially among the poorest people.
Stunting, both in utero and early childhood, is the devastating result of poor nutrition. Children suffering from stunting might never attain their full possible height. Brain development might never achieve full cognitive potential. Similarly, wasting in children is revealed to be a life-threatening result of poor nutrient intake or disease. Children suffering from wasting have weakened immunity, are susceptible to long term developmental delays, and face an increased risk of death, particularly when wasting is severe (UNICEF, WHO and World Bank Group Joint Child Malnutrition Estimates 2020; UNICEF, WHO and World Bank Group 2021). Lindtjørn (1990) reported that increased childhood mortality is associated with high prevalence of malnutrition. Specifically in the event of a disaster, children experience increasing nutritional needs that cannot be met fully by general food allowances and rations. Were et al. (2015) confirmed that almost half of all child deaths are associated with under-nutrition, which can increase during and in the aftermath of disaster.
To children, a disaster can mean starvation, rape, deprivation of movement, fear, lack of access to health care, diseases, hopelessness, and losing parents and loved ones. If conditions are prolonged through an extensive period of recovery, a disaster could mean lack of school attendance, creating an entire generation of illiterate people, especially in low-income and middle-income countries. Specifically, in a disaster, a lack of food might introduce diseases such as kwashiorkor, leaving children with an oversized head or stomach, standing on spindly legs with owlish eyes.
In spite of international commitments and progress in nutritional support for children, the increasing rate and unpredictable nature of disaster (both natural and human-induced) combined with dynamic characteristics of a society, child nutrition in disaster is becoming a more important aspect of disaster response. Attention must also be devoted to the background context including specific political affiliation, interest and socioeconomic status, and consistent and special care needs of children.
The aim of this scoping review is to identify and elucidate current achievements and gaps in child nutrition in disaster from the perspective of disaster health management.
The specific objectives are investigations of the following:
1. Effects of disaster on child nutrition and health.
2. Specific issues including, allergies, breast-feeding practices, and socio-cultural aspects.
3. Achievements and gaps of food security, policy, and ethics related to child nutrition during and immediately after disaster.
This study is a scoping literature review based on the PRISMA extension for scoping reviews (PRISMA-ScR) (Tricco et al. 2018). PubMed resources from November 1946 through October 2020 were searched to assess trends of reported studies of child nutrition in disaster. Keywords used for a search conducted on November 1, 2020 included “disaster and child nutrition”, “disaster management and child nutrition”, “food security and child nutrition” and “disaster and child food security”. We further manually selected references in the obtained articles, and also searched several international organization websites as additional data sources, e.g., UNDRR, UNICEF, WHO and FAO.
Eligibility criteriaThe following are the eligibility criteria:
1. Articles published during 1946-2020 were reviewed.
2. Article written in English language.
3. Articles with information related to disaster management, food security, and child nutrition.
Exclusion criteriaThe following conditions are the exclusion criteria:
1. Abstract-only articles
2. Non-English articles
3. Articles unrelated to child nutrition or food security
Fig. 1 shows the number of papers searched and screened. Among 1,504 search results, title screening selected 236 articles, out of which 87 articles were further identified by abstract assessment. After full review, 53 articles were retained for use in this study. There were an additional 50 manually sought documents including those from international organization websites. Overall, 103 articles were included in this study. Fig. 2A shows the trend of publications per year. Although there were several important initiative articles to alert agencies about child malnutrition in disaster, most of the articles were published after 1990. Fig. 2B presents the geographical characteristics. The most frequent region was Asia, followed by Africa and the Americas. That fact might reflect that occurrence of disaster is most frequent in Asia, whereas conflict-related situations occur frequently in Africa. Fig. 2C shows the type of hazard. It connotes that, whereas effects of disaster on child nutrition are generally considered, natural hazards show the highest proportion. Trends and categories of identified reports fundamentally indicate an improved and increasing recognition of importance of child nutrition globally.
Fig. 3 illustrates effects of child malnutrition in disaster on children’s physical and mental well-being. Disaster causes and exacerbates malnutrition in children, exerting deleterious effects on their overall health and well-being.

Numbers of papers searched and screened.
Of 1,504 search results, title screening picked up 236 articles, of which 87 articles were identified further by abstract assessment. After full review, 53 articles were retained for this study. There were additional 50 manually selected documents including some from international organization websites. Overall, 103 articles were included in this study.

Trends and categories of identified reports of the literature.
A. Trend of publications per year. B. Geographical characteristics. C. Types of hazard.

Effects of child malnutrition in disaster on child physical and mental well-being.
Multiple studies conducted worldwide have shown that disaster adversely affects child growth (Mahapatra et al. 2000; Hoddinott and Kinsey 2001; Portner 2010; Dhoubhadel et al. 2020). Large-scale emergencies in high-, middle-, and low-income countries have increased morbidity and mortality of infants and young children. These adverse outcomes are usually a result of gastrointestinal or respiratory tract infections including wound and skin infections and malaria, with associated malnutrition or dehydration (Dube et al. 2018; Gribble et al. 2019).
Existing risks to infants and young children from contaminated water, milk, and substandard sanitation increase considerably under emergency conditions and render them vulnerable to diseases (Heseltine 1952; UN, United Nations 2013). Consumption of a non-balanced diet might cause gastrointestinal symptoms in disaster survivors, even in a high-income countries, such as Japan (Inoue et al. 2014). According to a study conducted in Bangladesh, the risk of death from diarrhea faced by severely malnourished children was 17 times higher than that of other children (Fauveau et al. 1990). Adhisivam et al. (2006) confirmed diarrhea occurrence as three times more likely among children who were fed with a free breast milk substitute (BMS) than in children who were not fed with a BMS.
Most deaths that happen during complex humanitarian emergencies are attributable to preventable causes, especially increased rates of infectious diseases, malnutrition and violent trauma (Brennan and Nandy 2001). Insufficient dietary intake might compromise immune function as well as the function of many physiological systems (Golem and Byrd-Bredbenner 2015). Infectious diseases were an important cause of morbidity and mortality among children following the 2010 Haiti earthquake, with cholera being an important etiology (Dube et al. 2018). According to UNICEF (2019), undernutrition puts children at a greater risk of dying from common infections, increases the frequency and severity of infections, and delays recovery. This interaction creates a potent vicious cycle of deteriorating health and worsening nutritional status. Micronutrient intervention should accompany public health interventions to reduce common diseases associated with disaster such as measles (vitamin A) and diarrhea (zinc) (The Sphere Project 2011).
Macro-nutrient and micro-nutrient deficienciesAdverse effects of acute, chronic malnutrition, and micronutrient deficiencies on growth and development are profound in infants and young children (Dong et al. 2013). Therefore, emergency feeding should not only satisfy hunger but also meet nutritional needs (Tsuboyama-Kasaoka and Purba 2014). According to Black et al. (2013), malnutrition places children at higher risk of death. In fact, 45% of all child deaths in 2011 in low-income and middle-income countries were linked to malnutrition. This risk is heightened in disaster. Unfortunately, providing a diverse diet, including micronutrients, after a disaster has remained a challenge for disaster management (Ainehvand et al. 2019). Webb (2005) reported a rise in the prevalence of wasting among children in Aceh, Indonesia after the 2004 Indian Ocean Tsunami. Portner (2010) pointed out that each disaster occurrence increased the prevalence of stunting among children. The bulk of food aid takes the form of grains, which mainly contain carbohydrates (Webb et al. 2017; Dhoubhadel et al. 2020). A study conducted after the 2011 Great East Japan Earthquake (GEJE) by Inoue et al. (2014) showed that most food aid received, such as rice balls or bread, was carbohydrate-based, possibly because of their ready provision and abundance in emergency food pantries. Singh et al. (2006) found that many children in disaster-affected areas in India had kwashiorkor because of inadequate protein intake.
Micronutrient deficiencies are very common in disaster. Singh (2010) observed that all forms of vitamin deficiencies, micronutrient deficiencies, and diseases including iron deficiency anemia, vitamin A deficiency blindness, beriberi, pellagra, edema, and goiter are present in disaster-affected populations. Dube et al. (2018) reported that deficiencies of macro-nutrients and micro-nutrients persisted as important health concerns for children in the 2010 Haiti Earthquake despite ongoing efforts to address hunger. Emergency interventions to protect poor people should not simply be for gross caloric intake, but the quality of children’s diets as well (Block et al. 2004). This quantity and quality can be achieved by ensuring access to safe and nutritious foods, particularly for children to reduce levels of wasting and micronutrient deficiencies (Webb et al. 2017). Food rations must be fortified with essential micronutrients (Toole 1992; Pradhan et al. 2016). For example, in Algerian refugee camps, a fat spread fortified with vitamins and minerals led to increased linear growth and reductions in anemia (Lopriore et al. 2004). Choudhury and Bhuiya (1993) reported the need to distribute vitamin A to children in disaster-affected areas. The Sphere Project (2018) presented fortification of food products with micronutrients as an effective strategy for addressing micronutrient deficiencies.
Mental healthHeseltine (1952) was the first to conceptualize the effects of child malnutrition on child mental health. In a post-disaster condition, food provision must meet at least three criteria: it must be safe, allay hunger, and meet physiological needs for the maintenance of health and normal growth. The food and feeding conditions of children lead to profound implications for their emotional response to disaster. As such, both the food and conditions of feeding should help minimize psychological trauma associated with disaster. The report emphasized that measures must be taken to provide food within the accustomed setting of the family, home or the immediate neighborhood. Moreover, giving IYC familiar foods produced by familiar hands (preferably mother) helps considerably to minimize the sense of insecurity. Since Heseltine, however, few reports have described nutritional effects on child mental health in disaster, although many manually searched documents have emphasized effects of disaster on child mental health.
Children might not have some capability and experience in dealing with situations effectively because of their distinct vulnerabilities in disaster situations, including unique physiological, psychological, developmental, and social vulnerabilities. The myriads of problems caused by disaster endanger food security and further affect children’s psychological well-being. Be You (2021) confirmed that food insecurity degrades the mental health of children. When supportive persons or loved ones are missing or injured, the grief can be profound. Children can be expected to have greater difficulty processing and coping with such losses (Kousky 2016). Emotional or behavioral disorders manifested by parents and caregivers exacerbate children’s feelings of insecurity, making long-term emotional and behavioral disorders more likely (Stafford et al. 2012). Such disorders might also affect physical health and schooling (Kousky 2016).
After a disaster, children might develop symptoms such as fear, anhedonia, inattention, negative behavior at school, decline in academic performance, increased clinginess, interpersonal and behavioral control difficulties, withdrawal and isolation, hypervigilance, aggressive behavior, bed-wetting, somatic complaints, irritability, nightmares, and crying. Longer-lasting effects might include depression, anxiety, adjustment disorders, post-traumatic stress disorder, and physical symptoms including stomach pain, sleep deficiency, back pain, indigestion, arrythmia, and fainting (Speier 2000; Norris et al. 2002; Madrid et al. 2006; Stafford et al. 2012; Coombe et al. 2015; Zhang et al. 2015; SAMHSA, Substance Abuse and Mental Health Service Administration 2018). The effect is dire for children with pre-existing psychosocial stressors (homelessness, foster care, exposure to violence, etc.), low socioeconomic status, and special healthcare needs including cognitive delays and prior mental illness (Madrid et al. 2006; Toor et al. 2018). It is particularly interesting that most emotional responses of children in disaster are not pathological and require no psychiatric intervention aside from basic supportive interventions by trusted others in their environment (WHO 2011b; Stafford et al. 2012). WHO (2006) established that nutrition programs which include a psychosocial component are more effective at promoting growth and positive child development than nutritional programs without a psychosocial component.
Specific issues related to child nutrition in disaster are shown in Table 1.

Specific issues related to child nutrition in disaster.
OG, Operational Guidelines; the Code, International Code of Marketing of Breast-milk Substitutes; IYCF-E, Infant and Young Child Feeding in Emergencies
Children are steadily becoming allergic to common foods. According to Johns Hopkins Medicine (2021), during 1997-2007, the prevalence of reported food allergy increased 18% among children under age 18 years. Food allergies might be attributable to environmental pollution, poor dietary habits, climate change, increased consumption of genetically modified foods, or other causes. The increasing rate of food allergies is an emerging difficulty of child nutrition in disaster, but only one report has described food allergies of children in disaster (Hirase et al. 2019). The Japanese Society of Pediatric Allergy and Clinical Immunology recommends a week’s stock of allergen-free food. A survey of patients with food allergies in Kobe, Japan revealed that household stockpiles of allergen-free foods are inadequate. Results show that no correlation exists between the earthquake experience and the rate of stockpiling. Almost all patients carried their medication. The study suggested repeated and reinforced educational interventions about the importance of stockpiling allergen-free food and allergy sign plates with good visibility in evacuation centers to reduce confusion and to provide appropriate care (Hirase et al. 2019).
Breast-feeding practices in disasterActually, WHO and UNICEF have been promoting breast feeding and have developed the International Code of Marketing of Breast-milk Substitutes (the Code) in 1981 (WHO 1981) and IYCF programming guide (UNICEF 2011). Infants have very specific food and fluid requirements, an immature immune system, and are vulnerable to dehydration and are dependent on others for their needs (WHO 2009). Policies and guidelines on infant feeding in disaster, i.e., the Code, OG-IFE are based on protecting, promoting, and supporting exclusive breast-feeding. However, adherence to good practices is often constrained by an absence of institutional memory and failure of leadership and coordination (Young et al. 2004). Save the Children UK’s report on IYCF in Lebanon during the 2006 Israel-Lebanon conflict reported OG and the Code violations because of a lack of awareness (i.e., untargeted distribution of infant formula to the affected displaced populations), lack of commitment from NGOs and UN agencies to the Code and OG, and a failure to support mothers’ continuance of breast-feeding during and after the conflict (Save the Children 2007). Borrel et al. (2001) noted that infant-feeding products, including BMS, were perceived by many staff members of the food and non-food sector as just another type of humanitarian aid: not different from school bags, clothes, and household items.
Sulaiman et al. (2016) identified four infant feeding concerns during flooding in Kelantan, Malaysia: negative effects of the flood on infant nutritional status and their health; lack of privacy for mothers to breast-feed their babies comfortably; large donations of infant formula, rubber nipples, and feeding bottles often received from many sources; and misconceptions related to breast-feeding production and quality. Observations indicated that a large donation of infant formula to the mothers caused mothers to become hesitant to continue to breast-feed their babies. There were breast-feeding misconceptions among mothers, family members, community members, health care workers, and those involved in volunteer work in the disaster. For instance, some breast-feeding mothers believed that they should stop breast-feeding when they become malnourished or when their baby develops diarrhea (Sulaiman 2016; The Sphere Project 2018). Wrong customs and beliefs related to IYCF among mothers were the same pre-tsunami and post-tsunami and could have aggravated the occurrence of diarrhea along with the inappropriate distribution of poor-quality free BMS after a tsunami in India (Adhisivam et al. 2006). IYCF challenges in disaster include explanations of misconceptions about breast-feeding, inappropriate feeding in disaster, food insecurity hampering the procurement of nutritious food, competing household needs, and stress and psychological trauma that affect childcare practices (Save the Children 2012; Requejo et al. 2015; Prudhon et al. 2018).
Infants who are dependent on infant formula are more vulnerable because resources necessary for feeding such as infant formula, clean water, electricity or gas for heating water, hygienic food preparation and washing environments, and health care might be difficult or impossible to access in an emergency (Gribble and Berry 2011; WHO 2011a; DeYoung et al. 2018). Adhisivam et al. (2006) cautioned that if BMS supplies were widely available in emergencies, mothers who might otherwise breast-feed might needlessly start feeding with BMS. A survey of 84 countries conducted by the World Breast-feeding Trends Initiative reported that emergency preparedness was the least implemented aspect of infant feeding policy (Gupta and Suri 2016). In addition, the Global Nutrition Policy Review identified that only 25% of 172 countries had an IYCF in emergencies (IYCF-E) policy (WHO 2018). Similarly, Gribble et al. (2019) reported that emergency planners in Australia have devoted insufficient attention to the needs of infants and young children in emergencies, thereby placing them at risk of severe adverse health consequences. Reports starkly underscore the necessity for more attention worldwide to infant needs in disaster. Sulaiman et al. (2016) reported a multi-team collaboration involving various rescue missions comprising local government agencies, including their health and nutrition departments, NGOs, and individual volunteers to improve conditions of women and infants affected by disaster.
Socio-cultural factorsIn a time of disaster, distribution of food alone seems inadequate to prevent malnutrition in children. Studies have indicated that nutritionally fortified food formulations are not welcomed practically because the concept of relief food is viewed not only as provision of basic nutritional needs for survival but also of food as a symbol of cultural, religious, and psychological norms (Rukundo et al. 2015; Scott-Smith 2015; Nekouie Moghadam et al. 2017; Dhoubhadel et al. 2020). Child feeding practices and other household health, agriculture, and WASH behaviors contribute to high rates of malnutrition. Misconceptions, cultural practices, and other beliefs drive these behaviors (SPRING, Strengthening Partnerships, Results, and Innovations in Nutrition Globally 2018). Therefore, handling properties, preparation ease, religious and cultural acceptance, and individual tolerance are important food selection criteria in disaster response planning (Wien and Sabaté 2015; The Sphere Project 2018).
Ready-to-eat food items prepared for emergencies are almost identical under all conditions. In other words, different age, ethnic, and religious groups must choose their food from a limited and not very satisfying list (Jayatissa et al. 2006; Gribble et al. 2019). Young et al. (2004) opined that the general food rations should satisfy not only the population’s nutritional requirements but also qualitative criteria of cultural acceptability, safety, digestibility, and ease of preparation and storage. The Sphere Project (2011) added that project design should accommodate and respect cultural, spiritual, and traditional practices regarded as important by local people. Wien and Sabaté (2015), after analyzing many food groups, showed the propriety of plant-based foods such as nuts and dried fruits as emergency food. They pointed out that these food items are universally acceptable and that they are tolerated across cultures and religions. Ainehvand et al. (2019) concluded that emergency foods should reflect formulas and special foods for emergencies, food diversity, nutritional needs of different groups, food health and safety, and functional features such as packaging, cultural norms, and final price.
Numerous efforts by WHO, FAO, UNICEF, and other international agencies have led to the establishment of programs, guidance, and initiatives geared towards facilitating and promoting adequate and high-quality IYCF practices over the years. These include the 1963 FAO/WHO initiative of Codex Alimentarius, which is a collection of standards, guidelines and codes of practice to ensure that food is safe and that it can be traded (Codex Alimentarius Commission 2021), the International Code of Marketing of Breast-milk Substitutes (the Code) (WHO 1981); the Innocenti Declaration on the Protection, Promotion and Support of Breast-feeding (WHO and UNICEF 1990); the Baby-friendly Hospital Initiative of 1991 with subsequent revision in 2018 (WHO and UNICEF 2018), World Declaration and Plan of Action for Nutrition (FAO and WHO 1992), and the Global Strategy for Infant and Young Child Feeding (WHO 2003). To improve the quality of humanitarian responses and accountability for actions in disaster, The Sphere Project was initiated in 1997. It framed and revised the Humanitarian Charter and Minimum Standards in Humanitarian Response including food security and nutrition for IYCF (The Sphere Project 2018). Recognizing the importance of supporting IYCF in disaster, the Emergency Nutrition Network (ENN) established the IFE Core Group in 1999 with a mandate to develop policy guidance and capacity-building tools, to experience-capture on IYCF in emergency response, and to promote policy and practice changes in the context of preparedness and response. In 2001, the first Operational Guidance on Infant and Young Child Feeding in Emergencies (OG-IFE) was developed. It was endorsed in the 2010 World Health Assembly Resolution (WHA23.23) (IFE Core Group 2017, 2020). In addition, the United States Agency for International Development (USAID) adopted and established the essential micronutrient levels in relief materials (Webb et al. 2017). Researchers, practitioners and agencies have adopted and have consistently advocated that nutrition intervention should be undertaken in accordance with the OG-IFE and the Code (WHO 2011a; Shaker-Berbari et al. 2018; The Sphere Project 2018; IFE Core Group 2020; Codex Alimentarius Commission 2021).
Although the number of stunted children has declined by 10 percent globally over the last six years, progress is too slow to achieve the 2030 target of a 50 percent reduction in the number of stunted children. School-age children do not eat sufficient fruits and vegetables, regularly consume fast food and carbonated soft drinks, and are not physically active on a daily basis (FAO, IFAD, UNICEF, WFP and WHO 2019). An estimated 340 million children have hidden hunger involving vitamin and mineral deficiencies (UNICEF 2019). Disaster often unmasks pre-existing nutrition problems, particularly in low-income settings, which are far worse than the emergency threshold (CDC, Center for Disease Control and Prevention 2002; Jayatissa et al. 2006; Webb et al. 2014) and exacerbate pre-existing inequalities (The Sphere Project 2011).
In fact, higher rates of malnutrition before an emergency indicate greater vulnerability to malnutrition and a higher risk of mortality among children under five. In countries where the rate of stunting and underweight children is already high, disaster further aggravates the risk of malnutrition and mortality in newborns and growing children (Pradhan et al. 2016). Goudet et al. (2011) confirmed that barriers to appropriate IYCF practices exist in normal times and that they were escalated in the flood, thereby leading to extremely poor nutritional health in Dhaka slums in Bangladesh. Egawa et al. (2018) clarified that malnutrition in children under five worsened the INFORM disaster risk index (European Commission 2021), associated with low life expectancy. According to The Sphere Project (2011), the time necessary to reach the minimum standard depends on resources, access, insecurity, and living standards of an area before a disaster. Widespread poverty, insecurity, and poor health care are major triggers for child malnutrition in northern Nigeria (VOA, Voice of America 2019). Shoham (1996) implicated the traditional diet of Rwandans as causing vitamin A deficiency and high rates of anemia that are endemic in Rwanda.
Dong et al. (2014) observed two years after the 2008 Wenchuan earthquake in China that the proportions of stunting and wasting were significantly high in children even though the government provided a food basket of 1,730 kcal/day. A systematic review of nutrition interventions for children under five years old indicated that disaster in low-income countries are more likely to lead to higher morbidity and mortality than disaster striking middle-income and high-income countries because of higher vulnerabilities of the population, weaker healthcare systems, and limited surge capacity (Pradhan et al. 2015, 2016). In addition, in crisis-affected areas within Ethiopia, the prevalence of wasting exceeds the WHO emergency response threshold of 10%, indicating severe concerns for child nutrition. Generally, younger children are more vulnerable, with the youngest infants being the most vulnerable (WHO 2000; WHO Collaborative Study Team on the Role of the Prevention of Infant Mortality 2000; Zahran et al. 2008).
Herrera-Fontana et al. (2020) described that food insecurity was evident in all households in a rural community on the Ecuadorian coast. They inferred that this might have increased considerably after the 2016 earthquake, given the precariousness of conditions and poverty in which the population had always lived. This inference concurs with those reported by Alderman et al. (2012): floods cause malnutrition in infants and young children in rural areas and urban slum dwellings in developing countries. A rigorous nutritional assessment early in emergency might therefore cost-effectively help prevent or reduce malnutrition, provide pathways to identify, harness, and encourage local nutritious food consumption, and promote environmental hygiene and good cooking practices for better nutritional outcomes.
Conflict triggers food insecurity and affects nutrition for many reasons. Conflict often leads to disruption of crop production, destruction of food stores and livestock, compulsion of people to eat foods with lower nutritional value, disruption of market food supplies and price inflation, compulsion of people to live in unhealthy environments, degradation of health services, and degradation of productivity and family care structures (Delbiso et al. 2017).
Gaps in availability, accessibility, and quality of foodChildren’s vulnerability is increased considerably when they are separated from their families, unaccompanied, orphaned, or displaced following a disaster (UNDRR 2012). Living in evacuation shelters or temporary housing is associated with poor dietary intake (Toole 1995; Tsuboyama-Kasaoka and Purba 2014; Goryoda et al. 2019). Gribble et al. (2019) pointed that the prevalence of poor dietary intake was higher among 2011 GEJE survivors than among the general population. Raybould et al. (2018) reported that people were aware of food distributions in their camps or communities but were reluctant to use them because of reasons such as long waits in the heat, mobility concerns, and most especially fear of fighting and the physical nature of distributions. Tsuboyama-Kasaoka et al. (2014) corroborated that early post-disaster improvements in meal provision were best achieved when the numbers of evacuees per shelter were lower and by speedy restoration of the gas supply to provide a cooking environment.
Persistent severe wasting and micronutrient deficiencies among refugees and displaced persons are caused by the quality of relief food, especially when food aid is a mainstay for years. The challenge is whether the donated food commodities are fit for human consumption at the point of purchase, on arrival, and remain edible in transit and in storage (Landman 1999). Jelliffe (1969) pointed out that foods available for disaster relief are inadequately prepared to meet the needs of children. They often consist of inappropriate and poorly planned diets, and are often slightly past the expiration date. Moisture contents and broken grains were found to be important contributors to problems of infestation and spoilage in Mozambique, Zambia, and Sudan (Walker 1996). According to Marchione (2002) food aid is not as effective as it should be for protecting the nutritional well-being of disaster-affected people because of difficulties such as unreliable quantity of food supplied, the low quality of food supplied, and the lack of full recognition and coordination of food aid with other needs of people. Hossain and Kolsteren (2003) reported that 8% of the overall 9% of children who were normal during the disaster period, were found to be malnourished after four months. This finding is clearly reflective of the quantity and quality of food provided. Goudet et al. (2011) concurred that infants and young children ate the same meals as the rest of the family, which was either too spicy or which did not have the appropriate nutritional density and value.
Herrera-Fontana et al. (2020) analyzed the percentage of consumption by subgroups of foods. After the 2016 earthquake in Ecuador, they found that 100% of households consumed foods of low nutritional value such as refined cereals, sweets, spices, condiments, oils and sugary drinks, mainly soft drinks. There was low consumption of vegetables, fruits, meats, eggs and dairy products, although the households had a high food distribution. Nekouie Moghadam et al. (2017) also found absence of an emergency food distribution program and lack of food diversification up to several weeks following the 2003 Bam earthquake in Iran. Adequate efforts should be made to incorporate measures such as ensuring the supply of adequate energy and protein to all age groups and especially to preschool children, into nutrition programs to improve food security (Singh et al. 2006).
Administrative and organizational challengesDisaster is unsolved problems of development for which short-term relief is an inappropriate response because the right to adequate food in disaster and emergency response is complex (Landman 1999; Rukundo et al. 2015). Therefore, all agencies must develop road map(s) for children’s food and for nutrition security that integrate relief, recovery, and rehabilitation, and which promote sustainable development. Public health nutrition professionals must function conceptually, if not actually, within the relief-recovery-rehabilitation continuum (Macrae et al. 1997). According to Mahapatra et al. (2000), malnutrition remains a leading problem among preschool children of the Kalahandi district in India, where severe drought prevailed in the 1800s. This point has not improved in spite of nutrition intervention programs, which are currently in operation. Borrel et al. (2001) observed that strong sectoral divisions and poor communication among agencies, such as health, food and non-food agencies, limit effective co-ordination. This point was emphasized by O’Donnell et al. (2002): most agencies attempted to target vulnerable people. However, methods for identifying vulnerable people varied depending on the agency. Moreover, the definition of vulnerable populations to be targeted depended almost entirely on the mandate and discretion of the individual agencies. Seaman (1991) and Landman (1999) drew attention to operational staff who are accountable to donors, not recipients. Unfortunately, donors are more interested in the supply of, or access to food aid rather than the effects of food aid on the dietary intake and nutritional status of the recipients.
Shoham (1996) established that food and other relief aid supplied in disaster is often poorly coordinated and ineffective at reaching its target population. Furthermore, that study expressed that difficulties such as inappropriate ration planning, inequity of food distribution systems, and inefficient selective feeding programs occurred. They can be attributed to a set of institutional factors. These include failure of institutional memory, poor cooperation and coordination among relief agencies, lack of consensus among agencies over program design, and a shortage of suitably qualified technical staff. Tsuboyama-Kasaoka and Purba (2014) identified constraints faced by a nutrition programmer in disaster to include insufficient knowledge about emergency nutrition, insufficient human and material resources, partly because nutrition and health workers themselves were affected. Borrel et al. (2001) listed underlying reasons behind the failures in infant feeding in disaster, including weak institutionalization of policies, huge quantities of unsolicited donations of infant‐feeding products, absence of monitoring systems, inadequate coordination mechanisms, high costs of correcting mistakes, and cumulative effects of poor practices. Young et al. (2004) concluded that many practical challenges reduce the effectiveness of nutritional interventions in complex emergencies Important research and programmatic questions remain.
Administrative problems that were identified include improper distribution of food, absence of nutritional experts, and non-use of nutritional knowledge to examine the nutritional needs of people, non-timely provision of food, executive teams’ feeding, presence of thieves, lack of preparedness, and perceived lacks of time and funding (Marchione 2002; Young et al. 2004; Nekouie Moghadam et al. 2017; IFE Core Group 2020).
Room exists for improvement in smarter programming, more careful targeting, greater attention to cost-effectiveness (in relation to planned human outcomes, not just numbers of people fed), enhanced coordination of interagency processes, enhanced policy harmonization among international players, and application of best practices in product formulation can help increase the effect of food aid resources (Webb 2011). Making appropriate food readily available for children using the right approach can improve relief efforts (Jelliffe 1969). To deliver effective aid in disaster, international relief agencies must have a solid understanding of the political and social climates in which they are operating (Brennan and Nandy 2001). This would help to resolve ethical stances clearly to anticipate and prevent nutritional expertise or humanitarian efforts from being manipulated to serve geo-political ends (Seaman 1991; Landman 1999). Additionally, health and nutrition interventions should be based on objective epidemiological data.
Table 2 shows the achievements and existing gaps in child nutrition in disaster.

Achievements and gaps in child nutrition.
FAO, Food and Agriculture Organization; WHO, World Health Organization; UNICEF, United Nations International Children’s Emergency Fund; OG-IFE, Operational Guideline for IYCF in Emergency; IYCF, Infant and Young Child Feeding; ENN, Emergency Nutrition Network.
Disaster preparedness recommendation for child nutrition is summarized in Table 3.
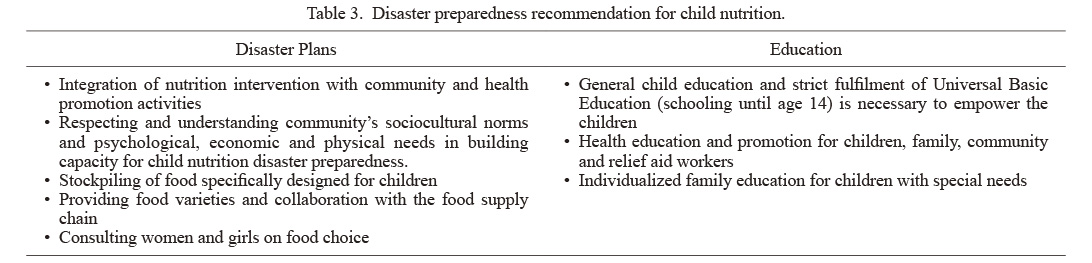
Disaster preparedness recommendation for child nutrition.
Nutrition intervention preparedness and education are fundamentally important. They have the potential to improve the nutritional outcomes of children in disaster. Specifically, interventions that are integrated with community mobilization and health promotion activities might be more sustainable in the long run. This might be particularly applicable in resource-poor settings, where the prevalence of nutrition deprivation is high, even under normal circumstances. Integrated nutrition interventions using locally available health resources might yield the best results (Pradhan et al. 2015, 2016). Tsuboyama-Kasaoka and Purba (2014) reported listening to and respecting the community’s knowledge, experience, views, and expertise Understanding their specific cultural, social, psychological, economic, and physical needs are all crucially important forces for building capacity for disaster preparedness in terms of nutrition.
Disaster risk is the potential loss of life, injury, or destroyed or damaged assets which can occur to a system, society, or a community during a specific period of time, determined probabilistically as a function of hazard, exposure, vulnerability, and capacity (UNDRR 2017; Egawa et al. 2018, 2020). Resilience can be improved when private individuals and institutions prepare by acting to build a culture of prevention and safety in a broad sense (UNDRR 2019). However, it is pertinent to include food security as part of preparedness to guarantee the nutritional health of the population, especially children, and thereby build resilience. Egawa et al. (2018) clarified that the socioeconomic categories (human development index, poverty index, Gini index, gender inequality and aid dependency) are strong determinants of the INFORM disaster risk index (European Commission 2021). Better food security and nutrition in disaster response are achieved through better preparedness. Such preparedness is the result of the capacities, relationships, and knowledge developed by governments, humanitarian agencies, local civil society organizations, communities and individuals to anticipate and respond effectively to the effects of likely, imminent or current hazards (The Sphere Project 2011).
An important responsibility of health authorities before disaster is to have exact plans and to study how foodstuffs must be supplied, stored, and distributed before, during and after the disaster. Golem and Byrd-Bredbenner (2015) established that post-disaster food supply plans provide safe food for people affected by disaster, including children. Although the humanitarian approach is prioritized in the short term, it should build on and strengthen local systems. Health effects of most major disaster can persist over months and years, irrespective of events (Nomura et al. 2016; Pradhan et al. 2016). Nutritional management in disaster is an inter-sectoral and inter-organizational issue that the relevant organizations must plan and cooperate to prevent, prepare for, respond to, and rehabilitate through (Nekouie Moghadam et al. 2017).
Several factors can contribute to deteriorating nutritional habits in the aftermath of disaster: worse access to food outlets because of residential displacement, financial difficulties, and social isolation (Goryoda et al. 2019). Providing sufficient energy for the public, devoting attention to vulnerable groups including children, providing food variety, preparing food-storage facilities, preventing food poisoning and spoilage, making use of proper methods of food distribution, and gaining people’s trust and satisfaction are of great importance (Movaghar et al. 2005; Gautschi et al. 2008). Hirase et al. (2019) stressed the importance of stockpiling allergen-free food. Amitani et al. (2017) highlighted the difficulties to ascertain what and how many items to stockpile and challenges in stock management because of the expiry dates, or perishable items, suggesting that preparedness and collaboration with food supply chain is important. For logistical reasons, Jelliffe (1969) reported that food should be packed in a compact, lightweight, weatherproof, pest-resistant, and easy-to-carry units.
The Sendai Framework is prioritizing women, children, and youths as stakeholders of disaster risk reduction (UN 2015). The role allocation is an essential principle for better preparedness. Important crisis management duty is to take exact steps to supply the nutritional needs of the people. Clarifying these steps will mitigate and eliminate difficulties that must be confronted after a disaster fewer (Nekouie Moghadam et al. 2017). Plan development for IYCF should consider factors including the following: clear allocation of responsibility for the needs of children to specific agencies; plans to maintain provision of essential services to children by agencies, organizations, educational and other facilities, especially those responsible for care and supervision of children; and consultation with child protection experts by all levels of government (Gribble et al. 2019). The latest version of The Sphere Project (2018) described consulting with women and girls about food choice because, in many settings, they most often have the primary responsibility for food preparation. Amitani et al. (2017) pointed out that nursery schools and daycare facilities for infants and small children should have stockpiles of food specifically designed for them.
EducationInvestment in education represents a clear means of financing risk reduction initiatives It makes a direct contribution to the creation of resilient societies (UNDRR-ROAMC 2021). Education, motivation, family involvement, and close follow-up to discuss barriers can empower families to be prepared to handle a disaster (Toor et al. 2018). Levac et al. (2012) clarified that most people in Canada and the US recognize the importance of emergency preparedness but do not report being prepared for a disaster or emergency situation. Rodriguez-Llanes et al. (2016) strongly recommended promotion of education in general and strict fulfillment of schooling until the compulsory 14 years of age to protect children’s health in the face of a future disaster. Young et al. (2004) reported the need for establishing guidelines for strengthening social support mechanisms and networks as a means of support for nutritionally at-risk groups. This need was echoed by Adhisivam et al. (2006): intensified health education is necessary to clarify doubts and encourage breast-feeding, especially during and after disaster. In addition, disaster nutrition education manuals are effective for the early resumption of food service. The manual contents should include human resource planning of nursery school cooks, alternative food suppliers in emergencies, and how to manage garbage when garbage collection is disrupted by disaster (Amitani et al. 2017). To improve disaster preparedness of families with parenteral nutrition-dependent children, Toor et al. (2018) advocated the use of individualized family education and the distribution of personalized disaster survival toolkits.
Imperfections of the search might have left other related articles out of our purview through the search procedures. Moreover, exclusion of non-English reports of the literature from this study is a limitation of this study.
Disaster endangers the nutritional health of children, resulting in effects on their mental, physical, and social wellbeing. Appropriate IYCF in disaster can prevent malnutrition and can save lives. Global collaborative efforts of relief agencies over the years to improve IYCF in disaster has led to the development of standardized guidelines and codes represented as Sphere Project and OG-IFE among others. However, pre-disaster malnutrition, food insecurity, living environment in shelters, poor breast-feeding including misconceptions about maintaining breast-feeding practices in disaster, sociocultural factors, and organizational and administrative challenges can strongly affect child nutrition in disaster.
Based on results of this study, one can recommend well-coordinated and explicit approaches at all levels of government and agencies that entail preparedness, advocacy, development and updating of policies, and education of children, family members, and relief aid workers about nutrition. Proactive participation of the general population, especially women, children, and youths, is necessary for advocacy and education of nutrition preparedness. Periodic nutritional assessment of children and nutritional supports in disaster by a designated IYCF authority can ensure effectiveness and efficiency. An urgent need exists to raise awareness and consideration of food allergies in children as an emergent difficulty for efficient nutrition intervention in disaster. Markedly few studies have examined effects of nutrition on child mental health in disaster. Consequently, future assessment in these areas is necessary.
This work was partly supported by JSPS KAKENHI Grant Number 17H00840, JP17H06108, and the Joint Usage / Research project of IRIDeS, Tohoku University; the Joint Usage / Research Center, “Research Center for Zoonosis Control, Hokkaido University” from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (MEXT).
The authors declare no conflict of interest.