Abstract
Insufficient data are available on comprehensive evaluation of demographics, symptoms or signs, laboratory findings, and disease course in patients with coronavirus disease 2019 (COVID-19) and chronic obstructive pulmonary disease (COPD). We aimed to evaluate whether COPD patients are more prone to severe COVID-19 compared with those without COPD. We also investigate the clinical characteristics and disease course of COVID-19 in patients with COPD versus those without COPD. Patients were selected from a Korean nationwide cohort of 5,628 patients with confirmed COVID-19 and who had completed treatment or quarantine by April 30, 2020; 3,673 patients aged 40 years or older were included in this study. COPD was diagnosed using patient reports of physician-diagnosed COPD. During the study period, all patients with COVID-19 in Korea were hospitalized following the national health policy. Of the study participants, 38 (1.0%) had COPD. Regarding initial symptoms, COPD patients with COVID-19 showed greater sputum production (50.0% vs. 29.8%, p < 0.01) and dyspnea (36.8% vs. 14.9%, p < 0.01) than those without COPD. In addition, patients with COPD were more likely to receive oxygen therapy or non-invasive ventilation (29.0% vs. 13.7%, p = 0.01) and had a higher mortality (21.1% vs. 6.4%, p < 0.01) than those without COPD. After adjusting for age, sex, body mass index, and comorbidities, COPD patients showed increased risk of severe COVID-19 compared with those without COPD. Our nationwide study showed that COVID-19 patients with COPD have higher symptomatic burden and more severe disease course than those without COPD.
Introduction
An ongoing severe acute respiratory syndrome caused by coronavirus 2 (SARS-CoV-2) that emerged in Wuhan, China, coronavirus disease 2019 (COVID-19), has spread across the world (Hu et al. 2020). Reports that describe the characteristics of COVID-19 suggest that the virus can progress to severe disease within a short time and has a high mortality rate (Chen et al. 2020; Phelan et al. 2020; Wu et al. 2020a; Zhou et al. 2020).
COVID-19 involves respiratory and systemic symptoms such as cough, sputum, dyspnea, myalgia, or febrile sensation (Hu et al. 2020; Zhou et al. 2020) as well as a devastating effect on the lungs. Accordingly, patients with chronic obstructive pulmonary disease (COPD), a representative respiratory disease, have higher susceptibility to severe presentation of COVID-19 (Alqahtani et al. 2020; Leung et al. 2020). Although COPD is only present in about 1.5-3.0% of the population, it is associated with a higher risk of severe presentation of COVID-19 according to the previous studies (Guan et al. 2020a; Lee et al. 2021). Other studies analyzing the association between COPD and the disease severity showed that the presence of COPD was associated with a more severe form of infection and death in patients with COVID-19 (Alqahtani et al. 2020; Attaway et al. 2020; Lippi and Henry 2020; Sanchez-Ramirez and Mackey 2020; Zhao et al. 2020b). However, there are insufficient data on the comprehensive evaluation of demographics, symptoms or signs, laboratory findings, and disease course in patients with COVID-19 according to the presence or absence of COPD.
Therefore, we aimed to evaluate whether COPD patients are more prone to severe COVID-19 compared with those without COPD. We also investigate the clinical characteristics and disease course of COVID-19 in patients with COPD versus those without COPD.
Methods
Study subjects and measurement
An anonymized nationwide cohort of 5,628 patients with confirmed COVID-19 infection and who had completed treatment or quarantine by April 30, 2020 was provided by the Korean Center for Disease Control (KCDC) for research purposes (KCDC database: http://ncov.mohw.go.kr/en/, accessed: April 30, 2020). Among the 5,628 patients diagnosed with SARS-CoV-2 infection, 3,673 aged 40 years or older were included in this study. During the study period, all patients with COVID-19 in Korea were hospitalized according to national health policy. The available data included demographics, respiratory and systemic symptoms, vital signs, patient-reported physician-diagnosed comorbidities, laboratory findings, highest level of disease severity [supplementary oxygen, non-invasive/invasive ventilation, extracorporeal membrane oxygenation (ECMO), and death]. As the highest level of disease severity was recorded, there were no available data regarding the highest level of treatment in patients who died.
SARS-CoV-2 infection was defined as a positive result on a real-time reverse-transcriptase polymerase chain reaction (PCR) assay of nasal or pharyngeal swabs according to the Guidelines for Laboratory Diagnosis of COVID-19 in Korea (Hong et al. 2020). COPD diagnosis was confirmed from patient reports of physician-diagnosed COPD in subjects of at least 40 years of age. Severe COVID-19 patients were defined as cases requiring supplemental oxygen therapy, non-invasive/invasive mechanical ventilation, or ECMO treatment in addition to those who died after confirmed COVID-19 diagnosis.
The Institutional Review Board of Hanyang University Hospital approved this study (IRB no. HYUN 2020-07-035). As the current COVID-19 cohort data were analyzed after anonymization, the need for informed consent was waived.
Statistical analysis
Data are presented as number (%) and are compared using the chi-square test or Mann-Whitney U test, as appropriate. To evaluate factors associated with severe COVID-19, we performed univariable and multivariable logistic regression analyses. In model 1, we adjusted for age, sex, and body mass index (BMI) group. In model 2, we adjusted for variables in model 1 and presence of asthma. In model 3, we adjusted for variables in model 2 and other meaningful comorbidities of heart failure, chronic kidney disease, and dementia (see Table 3). All data were analyzed using SAS® 9.4 (SAS Institute, Cary, NC, USA) and a two-sided p value < 0.05 was considered statistically significant.
Results
Baseline characteristics of the study population
Of 3,673 patients with COVID-19 enrolled in this study, 38 (1.0%) also had COPD. Compared with patients without COPD, those with COPD were older (p < 0.01), male-dominant (60.5% vs. 36.7%, p < 0.01), and had relatively lower BMI (p < 0.01). Regarding comorbidities, patients with COPD had more frequent asthma (23.7% vs. 2.3%, p < 0.01), heart failure (7.9% vs. 1.5%, p = 0.02), chronic kidney disease (13.2% vs. 1.3%, p < 0.01), and dementia (21.1% vs. 6.2%, p < 0.01) than those without COPD (Table 1).
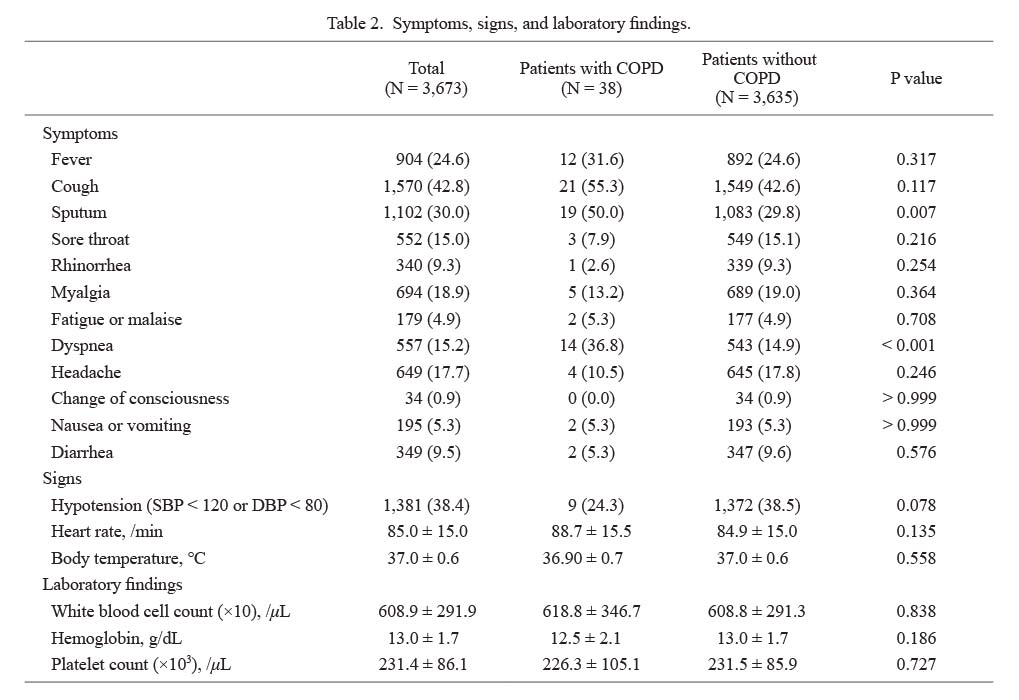
Symptoms, clinical signs, and laboratory tests
Regarding symptoms at the time of hospitalization, COPD patients with COVID-19 showed more frequent sputum (50.0% vs. 29.8%, p < 0.01) and dyspnea (36.8% vs. 14.9%, p < 0.01) than those without COPD (Table 2). However, in the clinical signs of systolic blood pressure, diastolic blood pressure, heart rate, and body temperature and laboratory findings of white blood cells (WBC), hemoglobin, and platelet count, there were no differences between patients with and without COPD (Table 2).
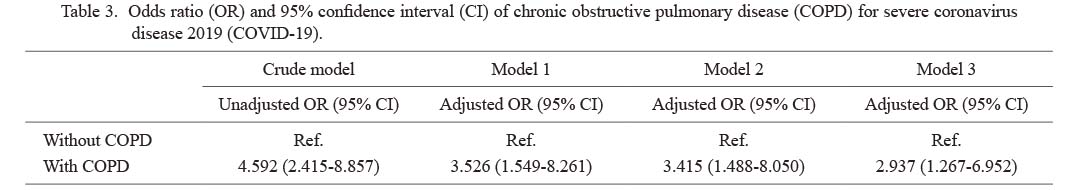
Severe COVID-19 infection
To evaluate whether the presence of COPD is associated with severe COVID-19, both univariable and multivariable logistic regression analyses were performed with models adjusting for age, sex, BMI, and co-morbidities such as asthma, heart failure, chronic kidney disease, and dementia. As shown in Table 3, COPD patients had a 2.94 (95% confidence interval, 1.27-6.95)-fold increased risk of severe COVID-19 compared with those without COPD.
The ICU admission rate and the highest level of disease severity according to COPD are shown in Fig. 1. Compared with patients without COPD, those with COPD were more likely to receive oxygen therapy or non-invasive ventilation (29.0% vs. 13.7%, p = 0.01). Additionally, patients with COPD had a higher risk of mortality than those without COPD (21.1% vs. 6.4%) (p < 0.01).
Discussion
Using a Korean nationwide database, we investigated the clinical aspects of COVID-19 in patients with COPD in comparison with those with COPD. We found that COPD patients with COVID-19 had clinical features making them more vulnerable to severe COVID-19, such as older age, male, and lower BMI, than those without COPD. Further, COPD patients had more frequent sputum production and dyspnea than those without COPD. Accordingly, COPD patients had a more severe presentation with higher mortality than those without COPD.
Considering that the first COVID-19 infection was detected from pneumonia of unknown origin (Zhao et al. 2020a) and that COVID-19 mainly accompanies various respiratory symptoms (Guan et al. 2020b), it is expected to have a serious effect on COPD, which is the most common chronic respiratory disease. However, the prevalence of COPD among patients with COVID-19 infection has been reported to be relatively lower (Alqahtani et al. 2020; Guan et al. 2020a; Olloquequi 2020) compared with that of other comorbidities such as hypertension and diabetes. In line with previous findings (Alqahtani et al. 2020; Guan et al. 2020a; Olloquequi 2020), the prevalence of COPD among COVID-19 patients was relatively low (only 1.0%) in our study. However, our results should be interpreted with caution. As we defined COPD based on patient self-report (recall bias) during a short period (selection bias), there is a possibility that the prevalence might have been underestimated. For example, a previous claim data-based study with almost the same population derived from the nationwide database in South Korea showed that the prevalence of COPD was 3% (Lee et al. 2021), which was higher than that of our results. However, despite this limitation, our study also has the advantage that we comprehensively evaluated the symptoms, signs, and treatment modality that could be hard to be evaluated using a claim-based study.
Despite the importance of knowledge regarding symptoms and signs to understand a disease, detailed clinical symptoms and signs of COVID-19 infection in COPD patients have not been well elucidated, perhaps because previous studies focused on prognosis (Alqahtani et al. 2020; Argenziano et al. 2020; Guan et al. 2020b; Kalyanaraman Marcello et al. 2020; Lee et al. 2021). Fortunately, a recent retrospective cohort study in China by Wu et al. (2020b) evaluated the clinical characteristics of COVID-19 in COPD patients. They found that COPD patients were more likely to have dyspnea and constitutional symptoms, such as diarrhea and fatigue than those without COPD (Wu et al. 2020b); however, that study did not use nationwide data. As such, our study has some advantages over this previous study. First, the data used in our study are from a nationwide database and were collected in a systematic, standardized method by the Korean Center for Disease Control. Second, as all patients diagnosed with COVID-19 in Korea are hospitalized due to national health policy, the disease progression of COVID-19 was observed closely. Similarly to the previous study, COPD patients had more frequent dyspnea than those without COPD. However, contrary to the findings in the previous study (Wu et al. 2020b), we saw no significant differences in constitutional symptoms between patients with and without COPD. The difference in health policy between China and Korea might be related to this difference. Since all Korean patients were hospitalized regardless of the severity of COVID-19 during the study period, our study is thought to include a larger number of less severe patients compared with the previous study.
There is increasing evidence that COPD is a major risk factor of severe COVID-19 (Alqahtani et al. 2020; Guan et al. 2020a). According to Guan et al. (2020a), patients with COPD as an underlying disease showed higher COVID-19 severity compared with patients without COPD (62.5% vs. 15.3%). Additionally, patients with COPD had an increased risk of ICU admission, mechanical ventilation, and death (Jain and Yuan 2020). However, most previous studies did not use a nationwide database or did not consider confounding factors to understand the relationship between COPD and COVID-19 severity. Overcoming this issue, our study showed that, even after adjusting for variables of age, sex, BMI, asthma heart failure, and other comorbidities, COPD is a risk factor associated with severe COVID-19 infection.
There are some limitations to our study. First, as COPD was defined as a patient-reported physician diagnosis during a relatively short duration, there might be a recall bias or selection bias that could have contributed to the underestimation of COPD. Second, as our database did not provide detailed information about smoking history, lung function, and treatment, we could not assess the impact of these variables on the symptoms, signs, and severity of COVID-19 in COPD patients. Third, as we used data that collected information during the early phase of COVID-19, the number of COPD patients was relatively small. However, unfortunately, a larger dataset that contains information after April 30, 2020 is not available. Accordingly, we could not validate our findings using a larger dataset. In addition, there is a possibility the relatively small volume of patients might have made an error in multivariable analyses. Fourth, our study was performed using a nationwide database of Korea. Thus, our results might not be generalizable to all ethnic groups. However, as analysis using a nationwide database minimized selection bias, this could be a major advantage of our study.
In conclusion, using a nationwide database, we showed that COVID-19 patients with COPD have a higher symptomatic burden compared with those without COPD. In addition, COPD patients had a more severe disease course than those without COPD even after adjusting for several important confounding factors.
Acknowledgments
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant No.: HI19C0218) and by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2019M3E5D1A01069363).
Author Contributions
Y. Kim and H. Lee contributed to the conception of the study, data collection, data analysis, and interpretation, and drafted the manuscript. S.K. Lee contributed to data collection, data analysis, and interpretation. B. Yang, H. Choi, D.W. Park, T.S. Park, J.Y. Moon, T.H. Kim, J.W. Sohn, and H.J. Yoon contributed to the data interpretation and revised the manuscript critically for important intellectual content. S.H. Kim contributed to the conception of the study, funding acquisition and data interpretation, and drafted the manuscript. All authors approved the final version of the manuscript.
Conflict of Interest
The authors declare no conflict of interest.
References
-
Alqahtani,
J.S.,
Oyelade,
T.,
Aldhahir,
A.M.,
Alghamdi,
S.M.,
Almehmadi,
M.,
Alqahtani,
A.S.,
Quaderi,
S.,
Mandal,
S. &
Hurst,
J.R.
(2020) Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PLoS One, 15, e0233147.
-
Argenziano,
M.G.,
Bruce,
S.L.,
Slater,
C.L.,
Tiao,
J.R.,
Baldwin,
M.R.,
Barr,
R.G.,
Chang,
B.P.,
Chau,
K.H.,
Choi,
J.J.,
Gavin,
N.,
Goyal,
P.,
Mills,
A.M.,
Patel,
A.A.,
Romney,
M.S.,
Safford,
M.M.,
et al.(2020) Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ, 369, m1996.
-
Attaway,
A.A.,
Zein,
J. &
Hatipoglu,
U.S.
(2020) SARS-CoV-2 infection in the COPD population is associated with increased healthcare utilization: an analysis of Cleveland clinic’s COVID-19 registry. EClinicalMedicine, 26, 100515.
-
Chen,
J.,
Qi,
T.,
Liu,
L.,
Ling,
Y.,
Qian,
Z.,
Li,
T.,
Li,
F.,
Xu,
Q.,
Zhang,
Y.,
Xu,
S.,
Song,
Z.,
Zeng,
Y.,
Shen,
Y.,
Shi,
Y.,
Zhu,
T.,
et al.(2020) Clinical progression of patients with COVID-19 in Shanghai, China. J. Infect., 80, e1-e6.
-
Guan,
W.J.,
Liang,
W.H.,
Zhao,
Y.,
Liang,
H.R.,
Chen,
Z.S.,
Li,
Y.M.,
Liu,
X.Q.,
Chen,
R.C.,
Tang,
C.L.,
Wang,
T.,
Ou,
C.Q.,
Li,
L.,
Chen,
P.Y.,
Sang,
L.,
Wang,
W.,
et al.(2020a) Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur. Respir. J., 55, 2000547.
-
Guan,
W.J.,
Ni,
Z.Y.,
Hu,
Y.,
Liang,
W.H.,
Ou,
C.Q.,
He,
J.X.,
Liu,
L.,
Shan,
H.,
Lei,
C.L.,
Hui,
D.S.C.,
Du,
B.,
Li,
L.J.,
Zeng,
G.,
Yuen,
K.Y.,
Chen,
R.C.,
et al.(2020b) Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med., 382, 1708-1720.
-
Hong,
K.H.,
Lee,
S.W.,
Kim,
T.S.,
Huh,
H.J.,
Lee,
J.,
Kim,
S.Y.,
Park,
J.S.,
Kim,
G.J.,
Sung,
H.,
Roh,
K.H.,
Kim,
J.S.,
Kim,
H.S.,
Lee,
S.T.,
Seong,
M.W.,
Ryoo,
N.,
et al.(2020) Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann. Lab. Med., 40, 351-360.
-
Hu,
X.,
Hu,
C.,
Yang,
Y.,
Chen,
J.,
Zhong,
P.,
Wen,
Y. &
Chen,
X.
(2020) Clinical characteristics and risk factors for severity of COVID-19 outside Wuhan: a double-center retrospective cohort study of 213 cases in Hunan, China. Ther. Adv. Respir. Dis., 14, 1753466620963035.
-
Jain,
V. &
Yuan,
J.M.
(2020) Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int. J. Public Health, 65, 533-546.
-
Kalyanaraman Marcello,
R.,
Dolle,
J.,
Grami,
S.,
Adule,
R.,
Li,
Z.,
Tatem,
K.,
Anyaogu,
C.,
Apfelroth,
S.,
Ayinla,
R.,
Boma,
N.,
Brady,
T.,
Cosme-Thormann,
B.F.,
Costarella,
R.,
Ford,
K.,
Gaither,
K.,
et al.(2020) Characteristics and outcomes of COVID-19 patients in New York City’s public hospital system. PloS One, 15, e0243027.
-
Lee,
S.C.,
Son,
K.J.,
Han,
C.H.,
Park,
S.C. &
Jung,
J.Y.
(2021) Impact of COPD on COVID-19 prognosis: a nationwide population-based study in South Korea. Sci. Rep., 11, 3735.
-
Leung,
J.M.,
Yang,
C.X.,
Tam,
A.,
Shaipanich,
T.,
Hackett,
T.L.,
Singhera,
G.K.,
Dorscheid,
D.R. &
Sin,
D.D.
(2020) ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur. Respir. J., 55, 2000688.
-
Lippi,
G. &
Henry,
B.M.
(2020) Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19). Respir. Med., 167, 105941.
-
Olloquequi,
J.
(2020) COVID-19 susceptibility in chronic obstructive pulmonary disease. Eur. J. Clin. Invest., 50, e13382.
-
Phelan,
A.L.,
Katz,
R. &
Gostin,
L.O.
(2020) The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA, 323, 709-710.
-
Sanchez-Ramirez,
D.C. &
Mackey,
D.
(2020) Underlying respiratory diseases, specifically COPD, and smoking are associated with severe COVID-19 outcomes: a systematic review and meta-analysis. Respir. Med., 171, 106096.
-
Wu,
C.,
Chen,
X.,
Cai,
Y.,
Xia,
J.,
Zhou,
X.,
Xu,
S.,
Huang,
H.,
Zhang,
L.,
Zhou,
X.,
Du,
C.,
Zhang,
Y.,
Song,
J.,
Wang,
S.,
Chao,
Y.,
Yang,
Z.,
et al.(2020a) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med., 180, 934-943.
-
Wu,
F.,
Zhou,
Y.,
Wang,
Z.,
Xie,
M.,
Shi,
Z.,
Tang,
Z.,
Li,
X.,
Li,
X.,
Lei,
C.,
Li,
Y.,
Ni,
Z.,
Hu,
Y.,
Liu,
X.,
Yin,
W.,
Cheng,
L.,
et al.(2020b) Clinical characteristics of COVID-19 infection in chronic obstructive pulmonary disease: a multicenter, retrospective, observational study. J. Thorac. Dis., 12, 1811-1823.
-
Zhao,
D.,
Yao,
F.,
Wang,
L.,
Zheng,
L.,
Gao,
Y.,
Ye,
J.,
Guo,
F.,
Zhao,
H. &
Gao,
R.
(2020a) A comparative study on the clinical features of coronavirus 2019 (COVID-19) pneumonia with other pneumonias. Clin. Infect. Dis., 71, 756-761.
-
Zhao,
Q.,
Meng,
M.,
Kumar,
R.,
Wu,
Y.,
Huang,
J.,
Lian,
N.,
Deng,
Y. &
Lin,
S.
(2020b) The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta-analysis. J. Med. Virol., 92, 1915-1921.
-
Zhou,
F.,
Yu,
T.,
Du,
R.,
Fan,
G.,
Liu,
Y.,
Liu,
Z.,
Xiang,
J.,
Wang,
Y.,
Song,
B.,
Gu,
X.,
Guan,
L.,
Wei,
Y.,
Li,
H.,
Wu,
X.,
Xu,
J.,
et al.(2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet, 395, 1054-1062.