2022 Volume 256 Issue 3 Pages 225-234
2022 Volume 256 Issue 3 Pages 225-234
The Tohoku University Hospital has been a clinical and research facility for all the related departments of Tohoku University. Medical-dental and interprofessional collaboration has resulted in special treatment teams, made up of members of departments such as the center for head and neck cancer, the center for dysphagia, and the cleft lip and palate center. Those treatment teams held conferences, case study meetings, reading sessions, and in-hospital seminars. The purpose of this study was to evaluate the outcomes of various medical-dental and the interprofessional collaboration at Tohoku University Hospital and training program to equip hospital dentists in higher medical institutions. The attainment targets are the acquisition of basic medical skills and knowledge under the guidance of supervising doctors. As a result, the hospital dentists could acquire their own specialized knowledge and skills certificated by each academic society. The smooth team treatment has been achieved, and the number of cases discussed by cancer boards and center for dysphagia has increased year by year due to the efficiency of their clinical pathways. On the dental care side as well, the wearing rates of maxillofacial prosthetic devices such as maxillofacial prostheses and palatal augmentation prostheses (PAP) have improved, which have contributed to improving patient’s stomatognathic function. Tohoku University Hospital has been practicing collaboration between medical and dental professionals and it has produced mutual benefits. Our interprofessional training system based on the medical-dental collaboration could develop professionals who have acquired cross-disciplinary knowledge and skills from experienced doctors.
Interprofessional approach may allow sharing of expertise and perspectives to form a common goal of restoring or maintaining an individual’s health and improving outcomes while combining resources. Interprofessional collaboration requires extensive and effective communication and teamwork, as well as knowledge and respect for the professions’ values, ethics, roles, and responsibilities. There have been various attempts in institutions of higher learning to meet this goal, with mixed results (Lumague et al. 2006; Bridges et al. 2011; De Los Santos et al. 2014; Fox et al. 2018).
Dentistry is no exception, and the establishment of consistent interprofessional collaboration on problems such as disease prevention and rehabilitation is an urgent issue for achieving patient quality of life (QOL). Treatments and rehabilitations for maxillofacial diseases are examples of where a team approach with interprofessional collaboration is needed, because treatment plans that consider the final prosthetic restoration to restore the patient’s oral function are desirable from the outset. For this purpose, it is necessary to establish a medical system where related medical fields cooperate and to practice comprehensive treatment, including rehabilitation. In particular, dental care at higher-order medical institutions such as university hospitals requires, not only dentists, dental hygienists, and dental technicians, but also a team approach that includes medical staff from other fields such as doctors, nurses, speech therapists, and community medicine. That is, it is essential to establish a “medical-dental and interprofessional collaboration” and to educate human resources staff about how they can support advanced medical care. However, most interprofessional training is collaboration among medicine and nursing or pharmacy staff (West et al. 2016). There are few higher-level medical institutions or hospitals that have medical-dental and interprofessional collaboration to treat maxillofacial diseases, nor dental resident education supported by the on-the-job training. Furthermore, the research has rarely been performed on the outcomes and effectiveness of the multidisciplinary approach for maxillofacial diseases (Jawad et al. 2015a, b; Epstein and Barasch 2018; Levi and Lalla 2018).
The Tohoku University Hospital has been a clinical and research facility for all the related departments of Tohoku University since 2009. Medical-dental and interprofessional collaboration have resulted in special treatment teams, made up of members of departments such as the head and neck cancer boards, the center for dysphagia, and the cleft lip and palate center. Therefore, the Tohoku University Hospital has been able to manage maxillofacial diseases using interprofessional collaboration of dentistry and medicine, and to educate professionals who have acquired cross-disciplinary knowledge and skills to practice high level and safe treatment.
The purpose of this study was to evaluate the outcomes of various medical-dental and the interprofessional collaboration at Tohoku University Hospital and training program to equip hospital dentists in higher medical institutions.
Examples of a team approach based on medical-dental cooperation and interprofessional collaboration at Tohoku University Hospital are described in Fig. 1.

Organizational framework of multi-professional collaboration and teams at Tohoku University Hospital.
PAP, palatal augmentation prosthesis; PLP, palatal lift prosthesis.
Recently, the use of cancer boards has become a valuable tool in the treatment of many kinds of cancers. A multidisciplinary cancer board has been accepted as best practice for the management of head and neck cancer. A dedicated multidisciplinary team caring for patients with head and neck cancer results in improved survival (Messing et al. 2019; Liu et al. 2020). At the Tohoku University Hospital, the cancer board was established in 2014. The head and neck cancer boards are discussion groups where all the disciplines involved in the treatment of a patient, such as head and neck surgery, therapeutic radiology, medical oncology, plastic and reconstructive surgery, oral and maxillofacial surgery, oral diagnosis, and maxillofacial prosthetic clinic, are brought together to determine the best course of treatment for that patient. Plastic surgeons and prosthodontists discuss mandibular reconstruction methods, such as the possibility of bony reconstruction, surgical simulation using computer aided design/computer aided manufacturing (CAD-CAM), surgical guide fabrication, and surgical application (van Baar et al. 2019). They also make a diagnosis of maxillary denture adaptation for postoperative or radiological maxillary defects. The head and neck cancer board plays an important role in these discussions because of the important issues surrounding the patient’s quality of survival (QOS), such as dysphagia, dysphonia, visual and hearing impairment, dysosmia, dyspepsia, and disturbance of movement of extremities after treatment. It is very important to take QOS into consideration in addition to the goal of better disease prognosis.
At the Tohoku University Hospital, the head and neck cancer board has met every week since July 2014 and has discussed over 1,200 cases involving head and neck cancer. New treatment options are also discussed, such as robotic surgery, proton and carbon beam radiotherapy, and immune checkpoint inhibitors. These detailed discussions result in tailor-made treatment plans for our patients.
Center for dysphagiaIn patients with advanced oral cancer, treatments often significantly impair life functions such as appearance, speech, chewing, and swallowing. Outcomes of dysphagia care using an established multidisciplinary team have been good. This pathway has provided patients with access to regular supportive care and has provided staff opportunities to provide early and ongoing dysphagia monitoring and management (Messing et al. 2019).
Treatment for dysphagia at Tohoku University Hospital started in 2012 and has mainly dealt with dysphagia caused by head and neck tumors with medical-dental collaboration. The center for dysphagia at Tohoku University Hospital was established in July 2019. The center was formed using a multidisciplinary team approach and consists of doctors of otolaryngology-head and neck surgery, oral and maxillofacial surgery, rehabilitation physicians, maxillofacial prosthodontists, speech therapists, nurses, and dental hygienists. To minimize post-treatment dysphagia in patients with advanced oral cancer, functional reconstructive surgery, rehabilitation, and prosthetic treatment must be planned and comprehensive. The multidisciplinary team begins to involve patients with advanced oral cancer before the surgery. The center serves as a starting point for the medical examinations and treatment of these patients, and seeks to improve the efficiency of cooperation between each discipline related to treatment. Thus, the center aims to improve the patient’s mastication and swallowing, prevent aspiration pneumonia, and facilitate early discharge. The main roles of dentistry are to evaluate oral function, promote oral care, and fabricate dentures, as well as to restore oral function with oral devices such as palatal augmentation prosthesis (PAP). This allows for comprehensive treatment and maximal maintenance of swallowing function after surgery.
Cleft lip and palate centerThe cleft lip and palate center at Tohoku University Hospital was established in July 2012. The cleft lip and palate center provides consistent treatment of congenital craniofacial disorders such as cleft lip and palate from birth to adulthood. The center uses a multidisciplinary team approach, with staff from plastic and reconstructive surgery, obstetrics, pediatrics, otolaryngology-head and neck surgery, orthodontics and speech therapy for craniofacial anomalies, maxillofacial prosthetic clinic, and oral and maxillofacial surgery. Outpatients are mainly treated by staff from plastic and reconstructive surgery, which performs surgical treatment, and staff from orthodontics and speech therapy for craniofacial anomalies, which performs orthodontic treatment. The inclusion of prenatal care and counseling and language therapy in the multifaceted approach is also essential for the treatment of cleft lip and palate. The maxillofacial prosthetic clinic is responsible for prosthetic treatment such as palatal lifting plate (PLP), maxillofacial prostheses, and dental implants. The wide-range jawbone-supporting prosthesis is a reconstructive treatment using dental implants. In 2012, National Health Insurance began paying for this treatment, which is used for patients with congenital disease of the cleft lip and palate with single or consecutive tooth defects or alveolar dysplasia of jawbone. These prosthetic treatments contribute to the completion of the patient’s final dentition and their recovery of oral function and QOL.
Maxillofacial prosthetic clinicThe maxillofacial prosthetic clinic at Tohoku University Hospital is responsible for the reconstruction of maxillofacial morphology and functional rehabilitation. The clinic was established in 2005 to specifically promote cooperation and interprofessional collaboration between the medical and dentistry departments when the Medical Hospital and Dental Hospital of Tohoku University were integrated. Since then, it has actively promoted cooperation between departments, such as otolaryngology, plastic surgery, and radiation therapy. The purpose of the clinic is to help patients using a prosthetic prosthesis recover from aesthetic disorders and issues with mastication, swallowing, and pronunciation. This is done with preoperative treatment planning, perioperative oral management, and subsequent rehabilitation. In order to fully achieve this purpose, reconstruction of the maxillofacial morphology and functional rehabilitation are essential. In particular, the combination of surgical reconstruction and rehabilitation for maxillofacial morphology defects, deformations, and deviations is important to functional recovery because the maxillofacial prosthesis alone cannot completely compensate for defects and reconstruct features. For these reasons, the maxillofacial prosthetic clinic works closely with the three centers mentioned above.
Digital dentistry, which is dental care based on digital technology, has also played an important role in maxillofacial reconstruction (van der Zande et al. 2015). The digital workflow and platforms for dentistry are as follows. First, computer-aided design (CAD), the shape data, are digitized, and the data are processed on a computer for imaging. Next, milling is performed, imaging is performed as a real model by computer-aided manufacturing (CAM), such as three-dimensional (3D) printing, and finally postoperative simulation (imaging) is performed (Fig. 2). This feedback allows further investigation. The greatest advantage of digitizing the workflow is that it enables multi-professional collaboration on the digitized platform.
The procedure for mandibular reconstruction using 3D models considering postoperative prosthesis is an example of a team approach to using the digital work platform before surgery. In other words, plastic surgeons and prosthodontists could work together with CAD software in the laboratory and clinical practice. The digitization will further strengthen collaboration.
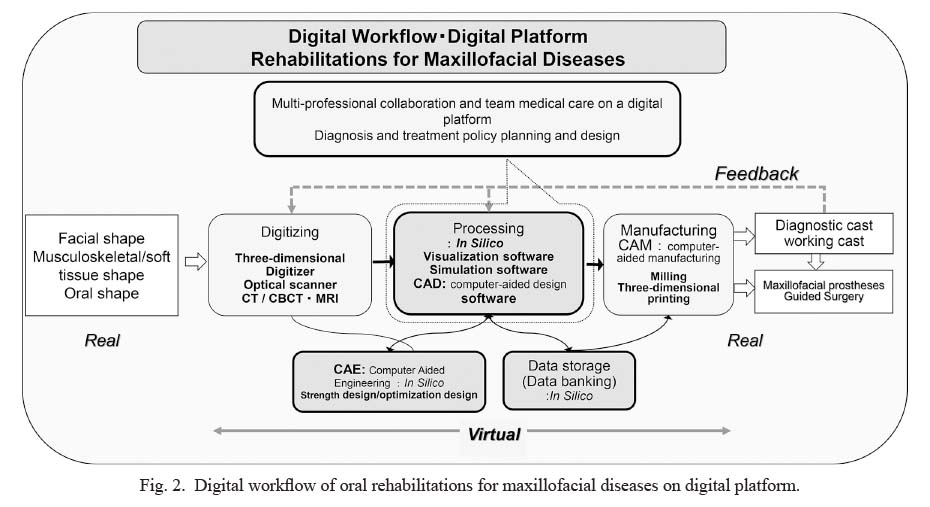
Digital workflow of oral rehabilitations for maxillofacial diseases on digital platform.
CT, computed tomography; CBCT, cone beam computed tomography; MRI, magnetic resonance imaging.
Attainment targets are the acquisition of basic medical skills and basic knowledge of maxillofacial diseases under the guidance of supervising doctors. Hospital dentists can acquire their own specialized knowledge and skills through participation in regularly held conferences, case study meetings, reading sessions, in-hospital seminars, and they can learn about specific treatments and patient management.
Definition of the outcomes and how to collect the outcome dataNumerical changes in number of wearing dentures or PAP, and number of cases videoendoscopic examination of swallowing (VE) and videofluoroscopic examination of swallowing (VF) examination was defined as the outcome of medical-dental collaboration and interprofessional training. Those outcome data were collected from the electronic medical database of Medical IT Center, which manages patient information from shared electronic medical records of the medical and dental departments at Tohoku University Hospital.
Statistical analysesLinear regression analysis was used to detect correlation between by year and number of wearing dentures or PAP, and number of cases VE and VF examination. Spearman’s correlation coefficient by rank test was used to detect correlation. The data were examined with the SPSS version 18.0 (IBM). P < 0.05 was considered statistically significant.
Ethical considerationsThis study was approved by the Tohoku University Hospital Institutional Review Board (IRB protocol number: 2019-3-6). This study was performed according to the Declaration of Helsinki, and all participants provided signed informed consent when wearing the maxillofacial prosthetic devices. The manuscript was drafted based on the STROBE statement.
Meetings of the head and neck cancer board have been held every week since July 2014, and members discussed and treated over 145 cases in the second half of 2014, 320 cases in 2015, 375 cases in 2016, 438 patients in 2017, 407 cases in 2018, and 520 patients in 2019 involving head and neck cancer. Of these, the average number of mandibular tumor cases before and after the start of the cancer board were similar, with 21 cases during a 3-year period (2011 to 2013) and 20 cases during a 5-year period (2014 to 2019). However, there was an increase in mandible reconstruction, from 41.9% (2011 to 2013) to 64.3% (2014 to 2019). Highly reproducible reconstruction of the mandible with correct occlusion was possible, and the mandible denture using rate improved from 46% before medical-dental cooperation to 78% after cooperation (Fig. 3). Regression analysis showed that number of wearing dentures increased linearly by year (r = 0.86, p < 0.05) (Fig. 4).
The outcomes that hospital dentists learned at head and neck cancer board are shown below. 1) Hospital dentists could learn about standard treatment of head and neck tumors (surgical therapy, radiation therapy, and chemotherapy) and advanced medical treatment decisions based on the latest treatment guidelines. 2) Hospital dentists could learn about CAD-CAM planning methods and procedure for mandibular reconstruction with the use of 3D models and an alignment tray manufactured in-house. 3) Hospital dentists could learn about the evaluation of oral and occlusal function after CAD-CAM reconstruction.
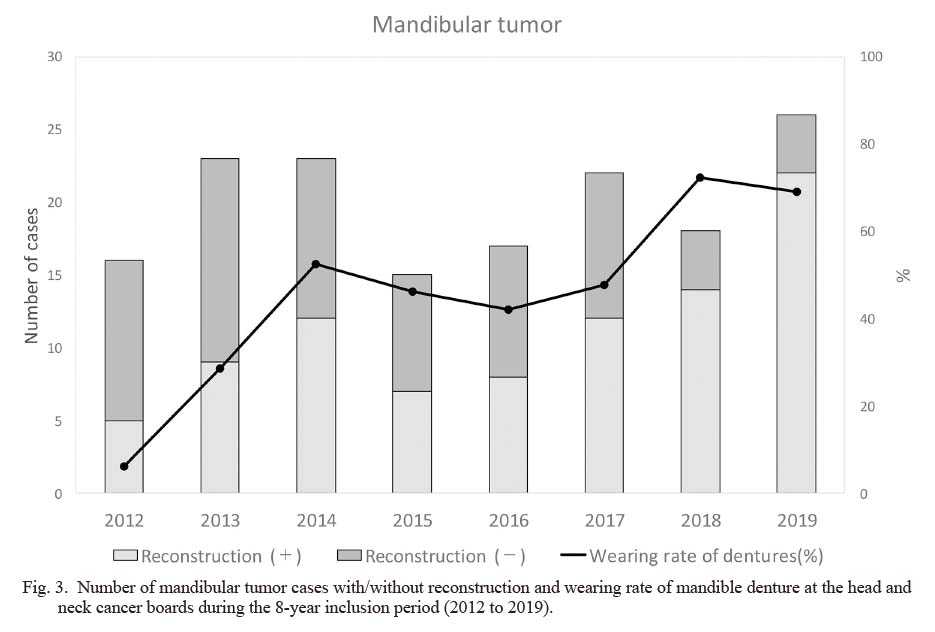
Number of mandibular tumor cases with/without reconstruction and wearing rate of mandible denture at the head and neck cancer boards during the 8-year inclusion period (2012 to 2019).
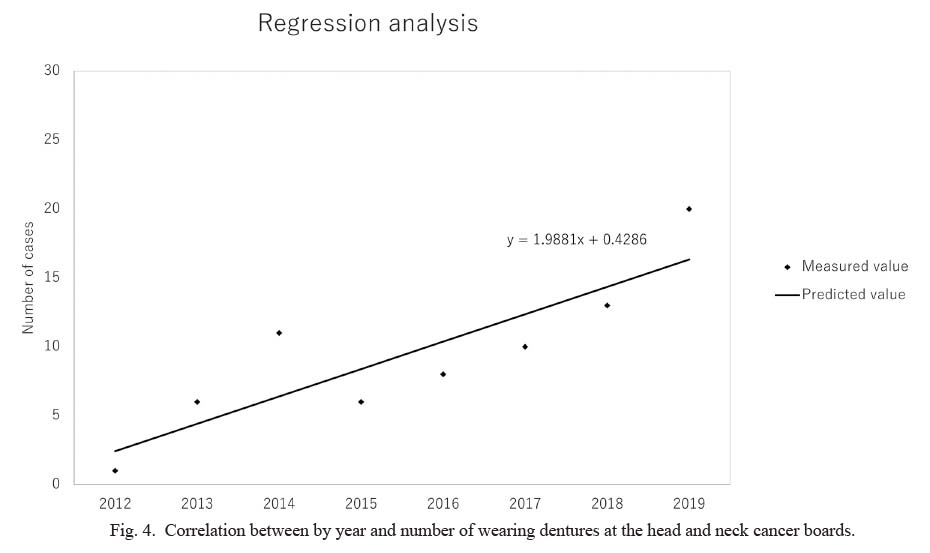
Correlation between by year and number of wearing dentures at the head and neck cancer boards.
Meetings of the center for dysphagia have been held every week since July 2012, and members discussed 294 cases in 2015, 421 cases in 2016, 456 patients in 2017, 560 cases in 2018, and 605 patients in 2019. As the number of patients has increased, the number of VE and VF tests has also increased significantly (Fig. 5). There was positive correlation by year and number of cases with VE (r = 0.97, p < 0.05) and VF (r = 0.94, p = 0.071), showing linear trends (Fig. 6).
Of these, the average number of tongue tumor cases before and after the start of the center for dysphagia have increased, with 25 cases during a 5-year period (2012 to 2016) and 47 cases during a 3-year period (2017 to 2019). However, the proportion of tongue reconstruction has remained stable. Preoperative involvement of prosthodontists makes it possible to perform dysphagia treatment for the oral stage of swallowing, and the PAP usage rate improved from 33.6% before medical-dental cooperation to 53.3% after cooperation (Fig. 7). Regression analysis showed that rate of wearing PAP increased linearly by year (r = 0.96, p < 0.05) (Fig. 8).
In recognition of this achievement, the center for dysphagia (dentistry) was started in 2021 as a branch of the center for dysphagia at Tohoku University Hospital for referrals from regional dental clinics. As the result, the network of hospitals and local clinics has been enhanced, and it has been possible to contribute to regional dental care.
The outcomes that hospital dentists learned at the center for dysphagia are shown below. 1) Hospital dentists could learn about VE, VF, swallowing function evaluation methods, oral function evaluation methods (oral cleaning status confirmation, oral QOL evaluation, oral dryness measurement, repeated saliva swallowing test, tongue pressure measurement, eat10, swallowing rehabilitation method, determination of swallowing food, and confirmation method of nutritional status). 2) Hospital dentists could learn about treatment decisions for new patients such as prosthetic devices (dentures, PAP) and swallowing surgery.
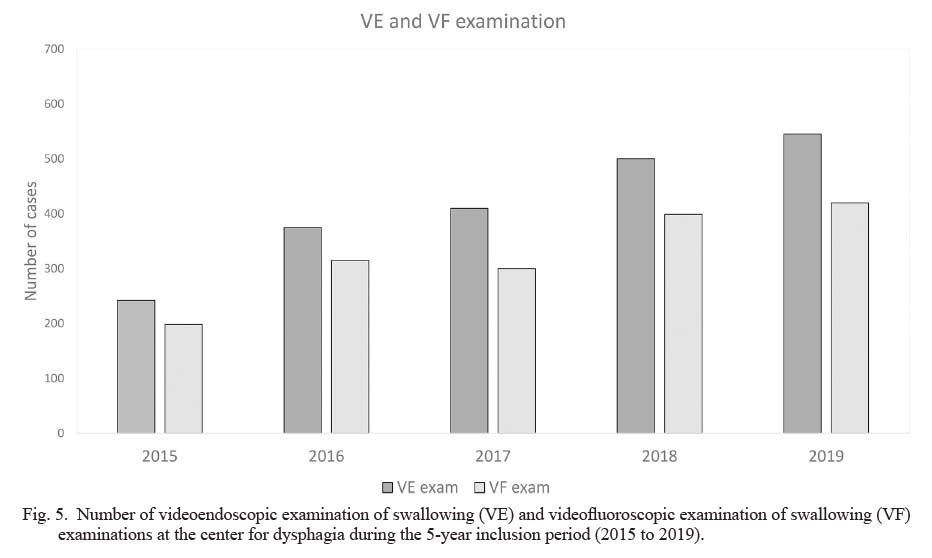
Number of videoendoscopic examination of swallowing (VE) and videofluoroscopic examination of swallowing (VF) examinations at the center for dysphagia during the 5-year inclusion period (2015 to 2019).
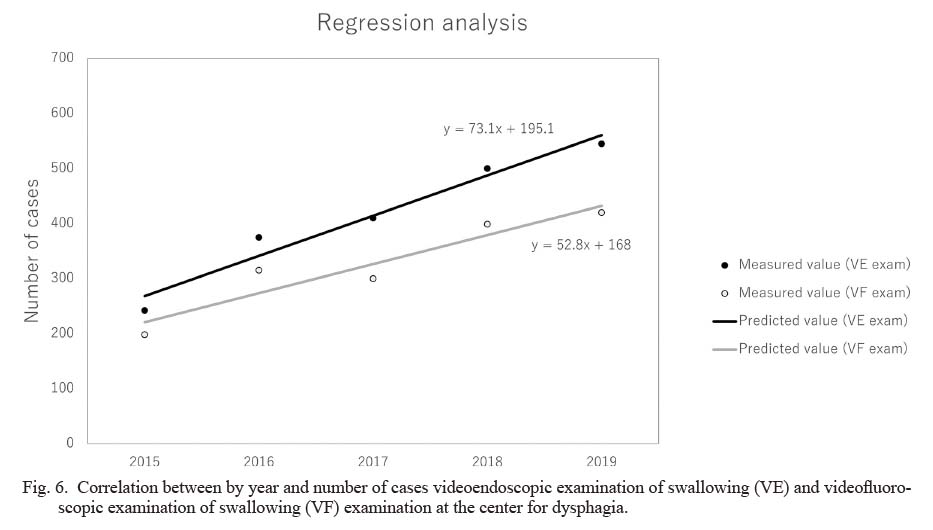
Correlation between by year and number of cases videoendoscopic examination of swallowing (VE) and videofluoroscopic examination of swallowing (VF) examination at the center for dysphagia.

Number of tongue tumor cases with/without reconstruction and wearing rate of palatal augmentation prosthesis (PAP) at the center for dysphagia during the 8-year inclusion period (2012 to 2019).
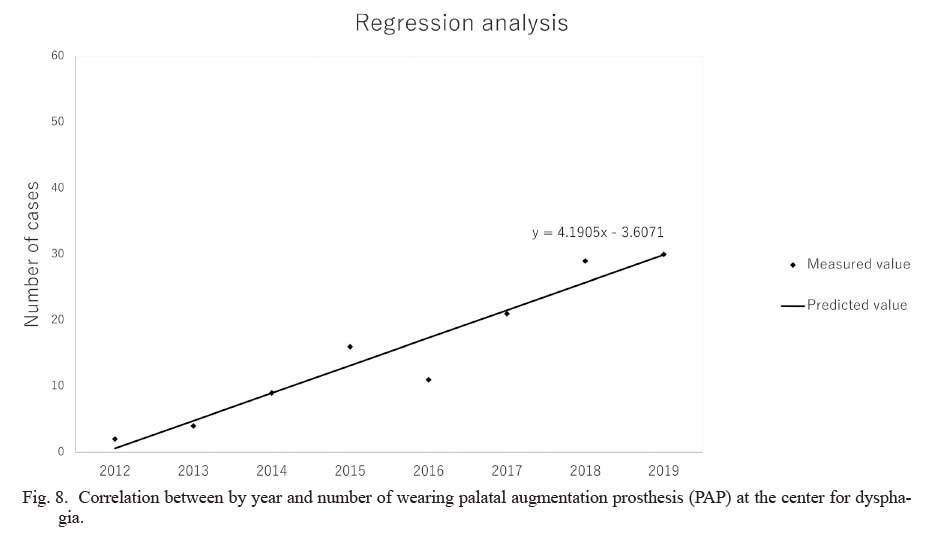
Correlation between by year and number of wearing palatal augmentation prosthesis (PAP) at the center for dysphagia.
1) Hospital dentists could learn about deciding the treatment policy for new patients and presenting computed tomography (CT) scan of the jawbone (1 month, and 6 months after surgery), evaluation of otitis media from an otolaryngologist, and speech evaluation from speech therapists (5 years old). 2) Hospital dentists could learn about cleft lip psychology clinic reports, lip and nose evaluation from a plastic surgeon, a cephalo analysis report of an osteotomy case, a 5-year index evaluation of jaw growth and occlusion from an orthodontist, and PLP device application criteria and evaluation methods from a maxillofacial prosthodontist at the expanded conference.
Outcome of maxillofacial prosthetic clinic at the dental implant center conference (held every week)1) Hospital dentists could learn about the possibility of dental implants for maxillofacial prosthetic treatment from oral surgeons, periodontists, prosthodontic specialists, and diagnostic imaging doctors. 2) Hospital dentists could learn how to simulate and determine the implant position prosthetically by matching the Standard Template Library (STL) and Digital Imaging and Communications in Medicine (DICOM) data of CT image of the wax up model at a conference on matching. Based on the final treatment plan, a surgical procedure guide can be fabricated after determining the manufacturer, size, surgical procedure, and so forth. 3) Hospital dentists could learn about the latest technology of dental implant treatments and the importance of cooperation through participation in these conferences.
Various medical-dental and the interprofessional collaboration have been established at Tohoku University Hospital, thereby the training has been provided through joint conferences and practice. As a result, the hospital dentists could acquire their own specialized knowledge and skills certificated by each academic society. The smooth team treatment has been achieved, and the number of cases discussed by center for head and neck cancer and center for dysphagia has increased year by year due to the efficiency of their clinical pathways. On the dental care side as well, the wearing rates of maxillofacial prosthetic devices such as maxillofacial prostheses and PAPs have improved, which have contributed to improving patient’s stomatognathic function.
Comparing the results before and after 2015 when medical-dental collaboration was established in earnest, the number of patients with head and neck tumors, the number of treatments, and the number of prosthetic treatments significantly increased in both the medical and dental departments. These have demonstrated the output and effectiveness of the diversified medical-dental and interprofessional collaboration at Tohoku University Hospital. The level of the hospital dentist side has improved year by year according to the accumulation of training and cooperation. Therefore, the hospital doctors’ understanding and trust in the hospital dentists has increased. This seems to have appeared as a numerical change, which can be regarded as the result of correlations. Consequently, dentists at Tohoku University Hospital have come to play an important role in collaboration.
However, for further development of this medical-dentistry collaboration, there are certain issues that are essential to solve, such as mutual understanding between occupations, sharing of medical information, meeting continuously and regularly to deepen mutual understanding, and respect for each other’s expertise. To solve these issues, hospital dentists in higher medical institutions must contribute as a member of the medical care team, and they must have training that allows them to practice multidisciplinary cooperation and provide appropriate support for other occupations after deepening their understanding of the systemic condition. The collaboration between professionals can work smoothly if participants learn professional skills that can be distinguished from other professionals, common skills required by all professionals, and collaborative skills required to collaborate with other professionals (World Health Organization 2010). The skills of collaboration, communication, and teamwork, as well as an understanding of the roles of the different healthcare professions, are essential for tomorrow’s healthcare professionals (Sabato et al. 2020). However, there are still few facilities that have established medical-dental collaboration. No matter how much professional skills improve, the dentists, excluding oral surgery specialists, lack cooperation skills, knowledge of medicine and systemic management, and understanding of others’ occupations. This might be due to the emphasis on only professional dental skills in undergraduate and postgraduate training.
In order to provide qualitatively guaranteed treatment and rehabilitation for maxillofacial diseases that can be trusted by society, appropriate training to develop the leaders of this collaboration is essential. It is necessary to have a medical service provision system in cooperation with related medical fields to realize practical training. Tohoku University Hospital, which has been established as a medical system that cooperates with related medical fields to practice comprehensive treatment, including rehabilitation, meets this requirement. The advantages of the Tohoku University medical-dental and interprofessional collaboration are 1) organization of a systematic curriculum consisting of multiple medical departments that cross medicine and dentistry, 2) development and expansion of the program based on existing medical-dental and interprofessional collaboration, and 3) effective training such as cross-professional lectures, practical training, and conferences based on the practice of team medical care. The training portion of the medical-dental cooperation and interprofessional collaboration at Tohoku University has become a comprehensive integrated approach aiming to build an advanced training system. This has happened because we were able to organically collaborate with each medical department of the hospital. 1) Basic medical skills, knowledge, and attitudes required for interprofessional collaboration, 2) coordination management and the ability to communicate with related medical fields, 3) the ability to develop an appropriate medical care plan, including the medical examination required for treatment, 4) the ability to formulate treatment plans for team medical treatments that correspond to individual patient conditions, 5) the ability to collaborate with multiple occupations to improve and maintain patient QOL, 6) the ability to understand lifelong learning habits, the need for team medical care, and the importance of acting as a team member, 7) advanced dental skills and knowledge of digital dentistry were acquired.
According to those acquirements, the ability to apply to actual diagnosis and treatment have been become possible. Furthermore, it has become possible to formulate a treatment plan that considers the final prosthodontic restoration from the outset to restore the oral function of the patient. Dentists have learned to treat maxillofacial disorders based on a multidisciplinary approach and team medical care. The hospital dentists, thus, would acquire the knowledge and medical terms that are essential for cooperation with the medical department. If these common skills could be acquired, it would help medical staff to understand the importance of the unique abilities that dental professionals have. Then, not only will collaboration skills develop, but also a smooth and equal relationship between dentists and medical staff. It would be challenges for the future to connect each specialized medical team or center and standardize a series of medical treatment plans and implementation processes from diagnosis, treatment and rehabilitation in order to improve the medical-dental and interprofessional collaboration and the quality of training.
The limitation of this study is that it has been able to show changes in quantity, such as the number of patients, however not in quality, such as improving medical treatment levels. Further research should examine the increase in the number of dentists who have acquired board certified specialist in this field and the improvements of outcome in each treatment as the results of medical-dental collaboration and interprofessional training. Furthermore, the number of cases as outcome might include other bias than the multidisciplinary approach such as patient’s condition or social situation. In this study, the data results up to 2019 were shown and analyzed because there were restrictions on medical treatment at Tohoku University Hospital due to Coronavirus diseases 2019 pandemic in 2020, in particular, refraining from VE examinations.
In conclusion, Tohoku University Hospital has been practicing collaboration between medical and dental professionals and it has produced mutual benefits. Our interprofessional training system based on the medical-dental collaboration could develop professionals who have acquired cross-disciplinary knowledge and skills from experienced doctors.
The authors thanks Prof. Yukio Katori of Department of Otolaryngology and Head and Neck Surgery, Tohoku University Graduate School of Medicine and Prof. Masahiro Tachi of Department of Plastic and Reconstructive Surgery, Tohoku University Graduate School of Medicine, for their support in accomplishing this study.
The authors declare no conflict of interest.