Abstract
Cholesterol granuloma is a benign, tumor-like lesion with an accumulation of cholesterol crystals in the tissue and is a consequence of a chronic inflammatory reaction. It commonly occurs in the middle ear but rarely in the liver. There is only one previous case report of cholesterol granuloma of the liver, which was caused by cholesterol hepatolithiasis. We report a case of cholesterol granuloma of the liver in a patient with no intrahepatic cholesterol stones; it was difficult to rule out malignant liver tumor preoperatively. The patient was a 79-year-old woman in whom a lesion in the liver was detected on abdominal ultrasonography. She was referred to our hospital for detailed examination and treatment. Abdominal contrast-enhanced computed tomography showed a 20 mm lesion with ring enhancement in the lateral segment of the liver during the arterial and delayed phases. Since a malignant tumor could not be ruled out radiologically, laparoscopic lateral segment hepatectomy was performed for definitive diagnosis and treatment. The resection specimen showed a yellowish-white lesion measuring 15 mm in diameter. Pathological examination showed a granulomatous lesion with cholesterol crystals surrounded by foreign body giant cells. The lesion was diagnosed as cholesterol granuloma of the liver. The postoperative course was good, and the patient was discharged on postoperative day 5. She was healthy, and no recurrence of the cholesterol granuloma was detected at the 5-month follow-up. This is the first case report of cholesterol granuloma of the liver mimicking a malignant liver tumor in a patient with no intrahepatic cholesterol stones.
Introduction
Liver tumors are often detected accidentally on abdominal ultrasonography, computed tomography (CT), or magnetic resonance imaging (MRI). These tumors might include neoplasms like hepatocellular carcinoma, intrahepatic cholangiocarcinoma, and metastatic tumor. Clinically, the detection of malignant liver tumors is particularly important because such patients have a poor prognosis. Cholesterol granuloma is a benign tumor-like lesion resulting from a chronic inflammatory reaction with an accumulation of cholesterol crystals in the tissue. It is often observed in the middle ear (Sagnic et al. 2021), but rarely occurs in the liver. There is only a single case report of cholesterol granuloma of the liver, which was caused by cholesterol hepatolithiasis (Saito et al. 1990). However, cholesterol granuloma in the absence of cholesterol hepatolithiasis has not yet been reported. In this report, we present a case of cholesterol granuloma of the liver, which occurred in the absence of intrahepatic cholesterol stones and mimicked a malignant liver tumor.
Case Presentation
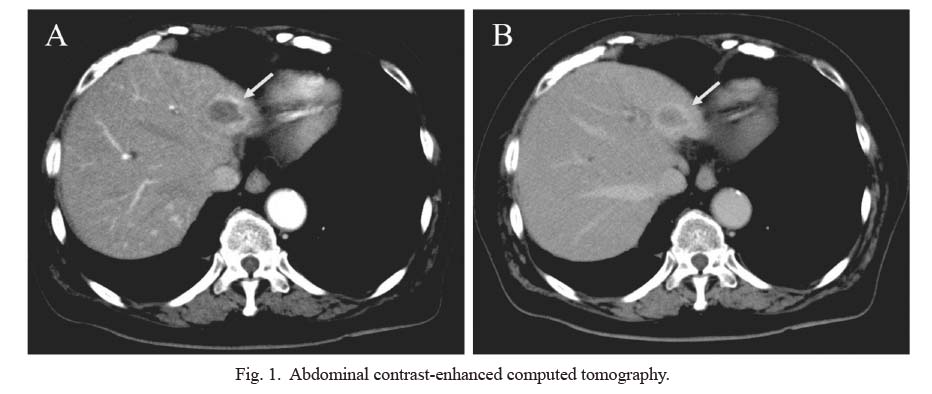
A 79-year-old woman was found to have a lesion in the liver on abdominal ultrasonography performed for screening and was thus referred to our hospital for detailed examination and treatment. She had no symptoms such as fever or abdominal pain and no history of abdominal trauma. She had a history of acute hepatitis approximately a year and a half before the liver lesion was detected and was hospitalized for a week and spontaneously recovered. She also underwent laparoscopic cholecystectomy for cholecystitis approximately 10 years ago and is receiving medical treatment for hyperlipidemia. Laboratory test results were as follows: white blood cell count, 6,200/μL (reference range 3,300-8,600/μL); C-reactive protein level, 0.02 mg/dL (reference range < 0.14 mg/dL); triglyceride level, 133 mg/dL (reference range < 149 mg/dL); total cholesterol level, 166 mg/dL (reference range < 219 mg/dL); LDL cholesterol level, 93 mg/dL (reference range < 139 mg/dL); HDL cholesterol level, 45 mg/dL (reference range > 40 mg/dL); and normal hepatobiliary enzymes levels. Alpha-fetoprotein level was 2.4 ng/mL (reference range < 10 ng/mL); protein induced by lack of vitamin K or antagonist-II level, 28 mAU/mL (reference range < 40 mAU/mL); carcinoembryonic antigen level, 3.0 ng/mL (reference range < 5.0 ng/mL); and carbohydrate antigen 19-9 level, 28.3 U/mL (reference range < 37 U/mL). Hepatitis B and C virus markers were negative. Anti-nuclear antibody was negative (1:40, reference range < 1:80), serum IgG concentration level was 1,324 mg/dL (reference range: 861-1,747 mg/dL), and anti-mitochondrial antibody was positive (32.9 index, reference range < 7.0). Abdominal contrast-enhanced CT showed a lesion measuring 20 mm in diameter with ring enhancement in the lateral segment of the liver during the arterial and delayed phases (Fig. 1). MRI revealed a lesion in the liver with low-signal intensity on the T1 weighted image (T1WI) and pale high-signal intensity on T2 weighted image (T2WI). Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced (EOB) -MRI showed isoenhancement of the lesion in the arterial phase and hypoenhancement in the hepatobiliary phase (Fig. 2). No bile duct lesion was found on magnetic resonance cholangiopancreatography. Positron emission tomography (PET)/CT showed uptake of 18F-fluorodeoxyglucose (FDG) in the lateral segment of the liver (a maximum standardized uptake value of 7.3) (Fig. 3). Based on these findings, hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma (ICC), metastatic liver tumor, or hepatic inflammatory pseudotumor was suspected, and surgical resection was planned accordingly.
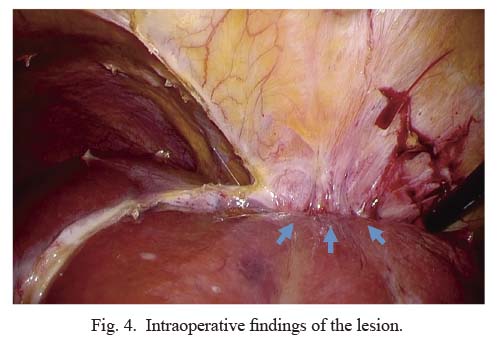
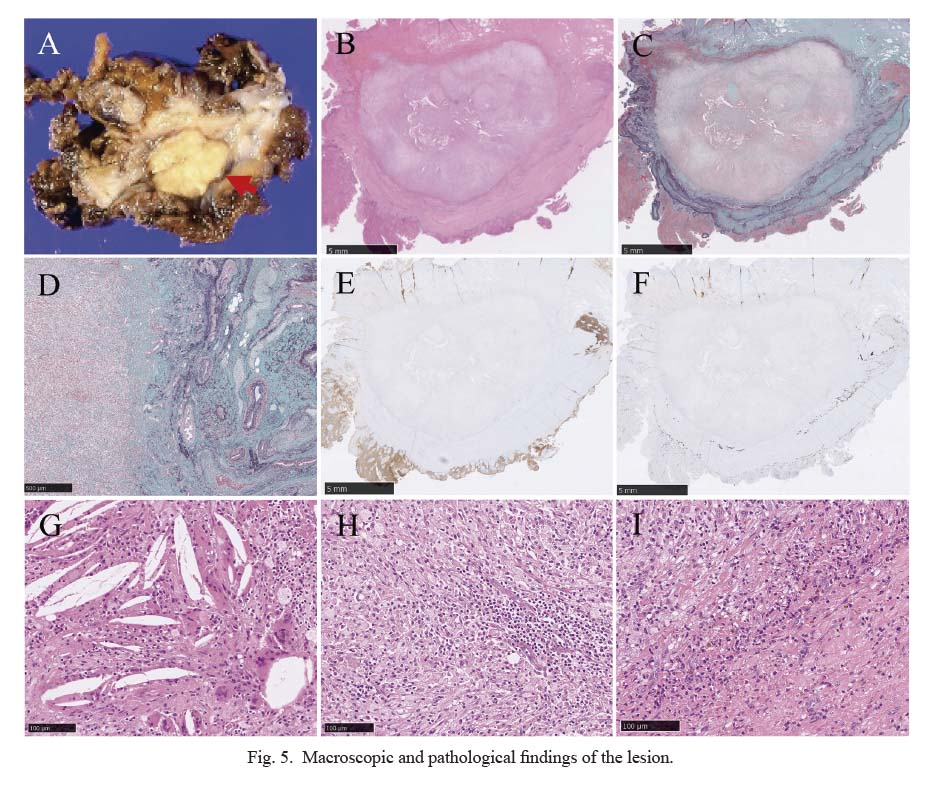
Laparoscopic lateral segment hepatectomy was performed in order to obtain a definitive diagnosis. Intraoperatively, the greater omentum was adherent to the abdominal wall, and the lesion was located in the lateral segment of the liver. Contrast-enhanced ultrasonography with Sonazoid® (GE Healthcare, Tokyo, Japan) showed a hypoechoic lesion measuring 20 mm in diameter in contact with the lateral superior branch of Glisson but not the umbilical portion. Liver dissection was difficult due to the adhesions between the lesion and the diaphragm (Fig. 4). Macroscopically, the resection specimen appeared as a yellowish-white lesion measuring 15 mm in diameter (Fig. 5A). Pathological examination revealed a granulomatous lesion with cholesterol crystals and fibrous capsule (Fig. 5B-I). Elastica-Masson staining showed that the lesion was located in a connective tissue containing bile ducts, portal veins, and hepatic arteries (Fig. 5C, D). Immunohistochemically, the lesion and surrounding tissue were negative for hepatocyte paraffin 1 (Fig. 5E), and the liver parenchyma was destroyed near the lesion. The tissue surrounding the lesion contained biliary epithelial cells that were positive for CK7 (Fig. 5F). Based on these findings, we decided that the lesion was located in a portal tract. Inflammatory cells, foreign body giant cells, and foamy macrophages were observed in the lesion (Fig. 5G, H); however, neutrophil infiltration and necrosis were unremarkable. Hemorrhage and bile were observed in the fibrous capsule of the lesion (Fig. 5I). In the rest of the hepatic tissue surrounding the lesion, liver fibrosis was unremarkable; however, inflammatory cell infiltration into the portal tracts and ductular reaction were observed (Fig. 5H). Based on these findings, we diagnosed the lesion as cholesterol granuloma of the liver. The postoperative course was good according to our enhanced recovery after surgery protocol (Fujio et al. 2020; Nakanishi et al. 2020), and the patient was discharged on postoperative day 5 with no complications. She was healthy, and no cholesterol granuloma recurrence was detected at the 5-month follow-up. She was to continue her follow-up at another hospital.
Informed consent was obtained from the patient for this case report.
Discussion
Cholesterol granuloma was first described by Manasse in 1894 (Manabe et al. 2020). It occurs commonly in the middle ear, but rarely in other organs such as the ovaries, breast, thyroid, kidney, pancreas, and liver (Kim 2017; Kim and Chang 2017; Sagnic et al. 2021). Although pathological examination shows a foreign body reaction to cholesterol crystals, the pathogenesis of cholesterol granuloma is not clear. Several hypotheses have been proposed, and one major hypothesis is that local hemorrhage due to inflammatory reactions causes degeneration of the cells, which develop cholesterol crystals. These crystals then induce a foreign body giant cell reaction, resulting in granuloma formation (Manabe et al. 2020). In the current case, it was clear that inflammation was involved, as the PET/CT scan showed increased FDG uptake in the cholesterol granuloma and there was intraoperative adhesion between the granuloma and adjacent organs.
In the liver, only one case report of cholesterol granuloma was previously reported (Saito et al. 1990). In this first case, the patient was diagnosed with hepatolithiasis preoperatively, and pathological examination revealed the cholesterol granuloma. Therefore, the researchers had suspected that cholesterol hepatolithiasis was the cause of the cholesterol granuloma. They proposed that cholesterol stone formation was associated with cholestasis, and hepatic bile was more associated with cholesterol stone formation than gallbladder bile. In our case, based on hemorrhage and bile observed in the fibrous capsule of the lesion, the formation of cholesterol granuloma could be related to the inflammation caused by bile cholestasis. Although no intrahepatic cholesterol stones were found in our case, it is possible that the cause of cholesterol granuloma was obstruction of biliary outflow owing to the lesion located in a portal tract. In addition, our patient had a history of acute hepatitis, and it was likely associated with this pathogenesis because of inflammation in the portal tract.
Hyperlipidemia may also be one possible hypothesis in the formation of cholesterol granuloma. There are reported cases of cholesterol granuloma in which patients were diagnosed with familial hypercholesterolemia (Albakheet et al. 2019). Furthermore, it is suspected that an elevated serum lipid level might contribute to increased lipid content in mammary secretions leading to cholesterol granuloma formation in the breast (Nam et al. 2019). Although preoperative serum lipid levels were within the normal range due to the intake of anti-lipidemic agents in our patient, she has been hyperlipidemic for an extended period. Thus, it was speculated that increased cholesterol content of the bile might have led to the cholesterol granuloma formation in our patient.
Hepatic inflammatory pseudotumor is a disease with similar pathogenesis to cholesterol granuloma in which inflammation is involved. There are several types of hepatic inflammatory pseudotumor with xanthogranuloma being one of them. There was a case of hepatic inflammatory pseudotumor associated with xanthogranulomatous cholangitis, in which the pathogenesis was suspected to involve an inflammatory response to exudated bile (Bae et al. 2015). Although characteristic pathological findings of xanthoguranuloma, such as foamy macrophages, were found in the current case, we diagnosed this patient with cholesterol granuloma due to the presence of cholesterol crystals. However, cholesterol granuloma of the liver may be a part of xanthoguranuloma due to similarities in the hypothesis of pathogenesis.
Although preoperative diagnosis of a cholesterol granuloma of the liver is as important as that of other tumors, it was difficult in our case. Because abdominal contrast-enhanced CT showed the lesion with ring enhancement, ICC, metastatic liver tumor, and hepatic inflammatory pseudotumor were suspected. Furthermore, findings of increased FDG uptake in the lesion on PET/CT supported this suspicion. However, based on EOB-MRI findings, HCC was also suspected, and thus, diagnosis could not be made according to radiological findings.
Since cholesterol granuloma is a benign lesion, a preoperative diagnosis might prevent unnecessary surgery. However, a case of an enlarging cholesterol granuloma of the breast following biopsy (Kim 2019) and another case of cholesterol granuloma of the pancreas accompanied by peritoneal dissemination (Imai et al. 2011) have been reported. In addition, a case of cholesterol granuloma of the breast accompanied by cancer was also reported (Furuhira et al. 2004). Therefore, in most cases, including ours, surgical resection is performed for diagnosis and to safely rule out malignancy. Since laparoscopic hepatectomy is feasible, and good postoperative outcomes can be expected, it could be considered instead of biopsy, resulting in more meaningful diagnosis and treatment in cases of cholesterol granuloma of the liver. Additional reports are necessary to fully elucidate the pathology and clinical significance of cholesterol granuloma of the liver.
In conclusion, this is the first report of cholesterol granuloma of the liver which occurred in the absence of intrahepatic cholesterol stones and mimics a malignant tumor. A malignant tumor could not be ruled out completely, and laparoscopic hepatectomy was performed. This case suggests that although a preoperative diagnosis may be difficult, cholesterol granuloma should be considered in the differential diagnosis of liver tumors.
Acknowledgments
We would like to thank Editage (https://www.editage.com) for English language editing. We would like to thank Dr. Hiroyuki Kumata (Japan Community Health Care Organization Sendai Hospital) for the patient data.
Conflict of Interest
The authors declare no conflict of interest.
References
-
Albakheet,
N.,
Al-Shawi,
Y.,
Bafaqeeh,
M.,
Fatani,
H.,
Orz,
Y. &
Shami,
I.
(2019) Familial hypercholesterolemia with bilateral cholesterol granuloma: a case series. Int. J. Surg. Case Rep., 62, 135-139.
-
Bae,
S.K.,
Abiru,
S.,
Kamohara,
Y.,
Hashimoto,
S.,
Otani,
M.,
Saeki,
A.,
Nagaoka,
S.,
Yamasaki,
K.,
Komori,
A.,
Ito,
M.,
Fujioka,
H. &
Yatsuhashi,
H.
(2015) Hepatic inflammatory pseudotumor associated with xanthogranulomatous cholangitis mimicking cholangiocarcinoma. Intern. Med., 54, 771-775.
-
Fujio,
A.,
Miyagi,
S.,
Tokodai,
K.,
Nakanishi,
W.,
Nishimura,
R.,
Mitsui,
K.,
Unno,
M. &
Kamei,
T.
(2020) Effects of a new perioperative enhanced recovery after surgery protocol in hepatectomy for hepatocellular carcinoma. Surg. Today, 50, 615-622.
-
Furuhira,
C.,
Ohshima,
A.,
Shimada,
K.,
Kuroki,
S.,
Nakano,
K.,
Ishikawa,
M.,
Yamamoto,
H. &
Tanaka,
M.
(2004) A case of breast cholesterol granuloma accompanied by cancer. Breast Cancer, 11, 210-213.
-
Imai,
H.,
Osada,
S.,
Sasaki,
Y.,
Ikawa,
A.,
Tanaka,
Y.,
Okumura,
N.,
Nonaka,
K.,
Takahashi,
T.,
Yamaguchi,
K.,
Yoshida,
K.,
Nakashima,
M. &
Hirose,
Y.
(2011) Cholesterol granuloma in the pancreas accompanied by peritoneal disseminated lesions. Pancreas, 40, 795-796.
-
Kim,
S.J.
(2019) Increasing size of cholesterol granuloma of the breast in the vicinity of a previous breast biopsy: imaging features and review of the literature. Am. J. Case Rep., 20, 370-376.
-
Kim,
W.W.
(2017) Cholesterol granuloma of the thyroid mimicking malignancy. OTO Open, 1, 2473974x17701092.
-
Kim,
Y.S. &
Chang,
J.M.
(2017) Sonographic appearance of a cholesterol granuloma mimicking breast cancer. J. Clin. Ultrasound, 45, 608-611.
-
Manabe,
T.,
Oka,
S. &
Ono,
K.
(2020) Multifocal cholesterol granulomas of the anterior mediastinum. Surg. Case Rep., 6, 182.
-
Nakanishi,
W.,
Miyagi,
S.,
Tokodai,
K.,
Fujio,
A.,
Sasaki,
K.,
Shono,
Y.,
Unno,
M. &
Kamei,
T.
(2020) Effect of enhanced recovery after surgery protocol on recovery after open hepatectomy: a randomized clinical trial. Ann. Surg. Treat. Res., 99, 320-328.
-
Nam,
G.,
Singer,
T.M.,
Lourenco,
A.P. &
Wang,
Y.
(2019) Cholesteroloma of the breast: a 10 year retrospective review of 79 cases with radiology correlation. Breast J., 25, 1177-1181.
-
Sagnic,
S.,
Bakir,
M.S.,
Birge,
Ö.,
Karadag,
C.,
Boduroglu,
A.,
Tuncer,
H.A. &
Simsek,
T.
(2021) Cholesterol granuloma mimicking ovarian cancer. Int. J. Clin. Exp. Pathol., 14, 741-745.
-
Saito,
K.,
Nakanuma,
Y.,
Ohta,
T.,
Ueda,
N.,
Higashino,
Y.,
Yamamichi,
N. &
Kidani,
E.
(1990) Morphological study of cholesterol hepatolithiasis. Report of three cases. J. Clin. Gastroenterol., 12, 585-590.