2022 Volume 257 Issue 1 Pages 77-84
2022 Volume 257 Issue 1 Pages 77-84
A Nankai Trough earthquake is highly likely to occur in near future, and perinatal medical resources and care in Kochi Prefecture may be insufficient after such an event. Therefore, we evaluated the medical and public health measures needed to prepare for caring for pregnant women in Kochi Prefecture in the aftermath of such an earthquake and the potential action plans for the prefecture. We estimated that immediately after an earthquake, approximately 30 pregnant women will require urgent medical treatment, most of whom will be in the prefectural capital, Kochi City, and perinatal medical care in Kochi City may be insufficient. Therefore, we used the projected flooding areas to divide Kochi City and its surrounding areas into 3 areas and allocated at least one Disaster Liaison for Pediatrics and Perinatal Medicine (DLPPM) to each disaster base hospital in those 3 areas. In a disaster, the DLPPMs will serve as key individuals in their respective areas and coordinate the allocation of medical care. A DLPPM will be allocated also within the Disaster Medical Response Headquarters of Kochi Prefecture and be responsible for overseeing perinatal care in the whole of Kochi Prefecture. Our study shows that estimating the number of affected pregnant women and requirement for perinatal medical care is an effective way to prepare realistic disaster measures and to enable a specific plan to be formulated for effective allocation and management of DLPPMs. We believe that our system can serve as a model in perinatal disaster medicine.
In recent years, many large-scale natural disasters have occurred in Japan, such as the Great East Japan Earthquake and tsunami in 2011 (Cabinet Office, Government of Japan: http://www.bousai.go.jp/updates/). In the immediate aftermath of a large-scale disaster, demands for medical care and public health measures are increased dramatically compared with ordinary times. In a disaster, vulnerable groups need special consideration and a lot of medical support; such groups include older people, disabled people, and infants, as well as pregnant women (Cabinet Office, Government of Japan 2016). To date, the situation and actions of a large-scale disaster for pregnant women are not well known (Sugawara et al. 2016), and past experience has been pointed out that the support for pregnant women was inadequate during disasters because their specific medical care and public health needs were not understood well. In addition, information about perinatal care was previously shared only with medical institutions for perinatal care and among people working at these institutions (MHLW 2016b) and not with the whole disaster medical management system, and this lack of information sharing was identified as a reason why support for pregnant women was delayed in previous disasters (MHLW 2019).
Learning from these lessons, in 2016, the Japanese Ministry of Health, Labour and Welfare (MHLW) began training obstetricians, pediatricians, midwives, nurses, and local government staff as Pediatric and Perinatal Medical Disaster Liaisons (DLPPMs). The DLPPMs are taught basic knowledge about disaster medicine, and they learn about the roles and tasks of a DLPPM through lectures, hands-on exercises, and drills simulating disaster situations (Wada 2018). During a disaster, the responsible DLPPM is expected to collect information on pediatric and perinatal care in areas affected by the disaster, provide advice, coordinate the necessary support and specific measures, and assist the Disaster Medical Coordinators at the Disaster Medical Response Headquarters (a Disaster Medical Coordinator is an individual who evaluates medical needs in affected areas and supports the dispatch of emergency medical teams so that the prefectural government or local healthcare centers can provide efficient overall coordination of healthcare activities during a disaster) (MHLW 2019). However, detailed measures have not yet been finalized on how best to use DLPPMs after they are trained.
According to The Headquarters for Earthquake Research Promotion (2020), in near future a Nankai Trough earthquake is expected to occur in the area that includes Kochi Prefecture and to cause enormous damage (Fig. 1). In case of a mega-earthquake, Kochi Prefecture estimates that there will be approximately 42,000 deaths and approximately 36,000 seriously injured people in the prefecture (Kochi Prefecture 2013a). It also expects that a significant number of pregnant women will be affected; however, the number of pregnant women and requirement for perinatal medical resources have not been estimated. If disaster preparedness measures for pregnant women are not taken, these women will not receive even the most minimal medical care or public health support when the next large-scale disaster occurs.
Because of the lack of information on the expected number of pregnant women who would require perinatal care after a Nankai Trough earthquake, we estimated the number of pregnant women and requirement for perinatal medical care in Kochi Prefecture. We then used the estimate to prepare a plan for providing medical care and public health measures for pregnant women and to propose a method for how DLPPMs can act effectively in disaster situations.
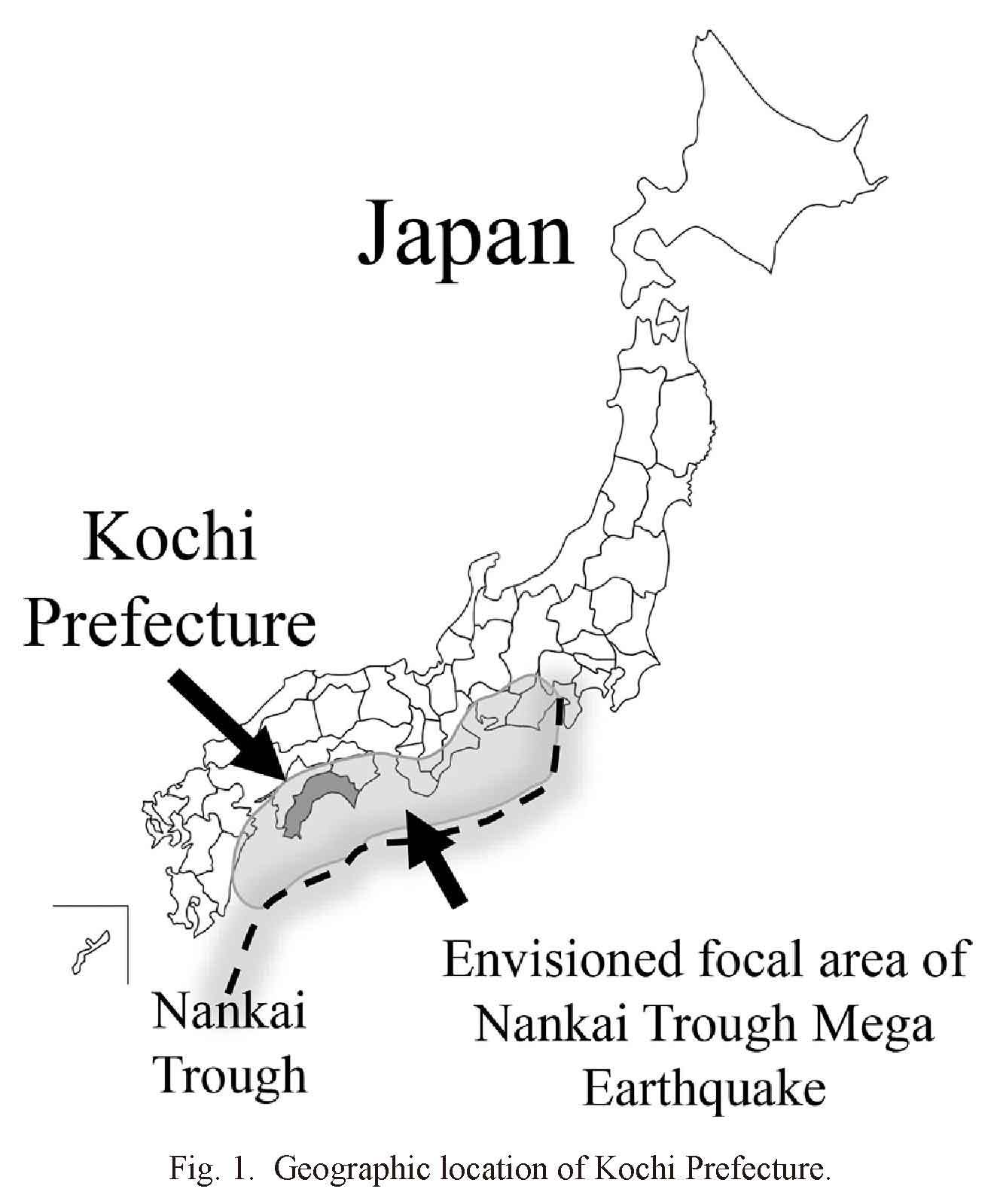
Geographic location of Kochi Prefecture.
Kochi Prefecture is located within the potential epicentral area of a Nankai Trough earthquake.
In the following, we describe the steps we took to estimate the number of pregnant women who would be affected by a large-scale disaster in Kochi Prefecture.
Current status in Kochi PrefectureMedical care plan, facilities for delivery: First, we referred to the Kochi Prefectural Medical Support Plan to assess the current status of the perinatal medical care plan and disaster medical care plan in the prefecture (Kochi Prefecture 2018a).
Population, number of births: Then, we used the Vital Statistics of Japan (Statistics Bureau of Japan 2019) to gather information on the population and the number of births per municipal unit in Kochi Prefecture.
Estimating the number of seriously injured and displaced pregnant women and the number of available beds for obstetrics and gynecologyTo obtain objective data, we calculated the number of pregnant women who would be affected and the number of requirement for perinatal medical care in case of a Nankai Trough earthquake. Specifically, we estimated the number of affected pregnant women as the number of seriously injured pregnant women and the number of displaced pregnant women. The requirement for perinatal medical care was estimated as the number of available obstetrics and gynecology beds during a disaster.
Estimating the number of seriously injured and displaced pregnant women: To estimate the number of seriously injured and displaced pregnant women, we used the estimate of the number of seriously injured and displaced people per municipal unit in Kochi Prefecture (Kochi Prefecture 2013b). The estimates for Kochi Prefecture were for 2013, so we calculated new estimates on the basis of the population and number of births in 2018. We also assumed that no progress had been made in disaster medical measures in the last five years. For this calculation, the number of seriously injured pregnant women was defined as the number of pregnant women who were injured as a direct effect of the disaster.
No data on the number of pregnant women have been published by the prefectural government or Kochi Prefecture. Therefore, we calculated the expected number of pregnant women by using a standard pregnancy period of 40 weeks and the following formula [the number of annual births was obtained from the 2018 Vital Statistics of Japan (Statistics Bureau of Japan 2019)]: Expected number of pregnant women = 40 weeks / 52 weeks × Annual number of births
In addition, we used the disaster estimate calculation method released by the Cabinet Office (Cabinet Office, Government of Japan 2013) to calculate the number of seriously injured and displaced pregnant women with the following formula: Number of seriously injured or displaced pregnant women per municipal unit = Number of seriously injured or displaced persons per municipal unit × (Number of pregnant women per municipal unit / Total number of people in each municipal unit).
The estimated number of affected pregnant women was calculated for each secondary medical area because, during disasters, the national government requires that the medical response system is organized on the basis of the disaster base hospitals in each secondary medical area (MHLW 2020).
Estimating the number of available beds for obstetrics and gynecology: In the aftermath of the Great East Japan Earthquake, the majority of maternity clinics and midwifery homes were unable to reopen (Sugawara et al. 2016). Therefore, we assumed that maternity clinics and midwifery homes in Kochi Prefecture will not be able to reopen after a Nankai Trough earthquake and that maternity beds will be available only in hospitals, which will handle all deliveries of babies and management of seriously injured pregnant women during disasters.
First, we calculated the mean daily bed vacancy rate at each hospital (Kochi Prefecture 2018b), as follows: Mean bed vacancy rate at each hospital = 1 − (Mean number of daily hospitalized patients / Number of beds at each hospital).
Next, we calculated the number of available maternity beds, as follows: Number of available maternity beds = Mean bed vacancy rate at each hospital × Number of maternity beds at each hospital.
During a disaster, hospitals may be able to provide medical care at only 60% of their normal level (Cabinet Office, Government of Japan 2013). Therefore, we calculated the number of available maternity beds during a disaster, as follows: Number of available maternity beds during a disaster = Number of available maternity beds × 0.6
We performed these calculations for each medical area and summed the results.
Establishing an action plan for perinatal disaster medical care in Kochi PrefectureBy using the above results and the tsunami hazard map (Kochi City 2012), we suggested perinatal disaster measures for Kochi Prefecture. In 2018, a working group was established to explore disaster measures for perinatal medical care in Kochi Prefecture. Since then, healthcare experts and local government staff have jointly investigated disaster preparedness for perinatal care by referring to our proposals.
Medical care plan, facilities for delivery: Kochi Prefecture is divided into 4 secondary medical areas: the Aki Medical Area in the east, the Chuo Medical Area in the center, and the Koban and Hata Medical Areas in the west; Kochi City is located in the Chuo Medical Area (Fig. 2). Kochi Prefecture has a total of 14 facilities for delivering babies, 11 of which are in Kochi City or the nearby Nankoku City; all 11 facilities are in the Chuo Medical Area (Table 1). In contrast, the Koban Medical Area has no such facilities, so patients from that area who require perinatal medical care need to be treated by a hospital in the Chuo or Hata Medical Area. As mentioned above, during disasters, the medical response system is organized on the basis of disaster base hospitals in each secondary medical area (MHLW 2020). However, the system is intended for standard medical care and not for specialized medical services, including perinatal care. Because the Koban Medical Area does not have a disaster base hospital with delivery capabilities, that area may not be able to determine the medical statuses of pregnant women or provide the necessary care in case of a large-scale disaster.
Population, number of births: In 2018, the population of Kochi Prefecture was approximately 725,000 people. Approximately 532,000 (73.4%) of the population was in the Chuo Medical Area, and approximately 332,000 of those people lived in Kochi City. Thus, the population of Kochi City represented 45.8% of the entire prefecture (Table 2). The number of births in each secondary medical area is shown in Table 2. The Chuo Medical Area has the highest number of births (3,803 births), and the mean number of daily births is approximately 10, more than half of which are in Kochi City (2,604 births; Table 2).
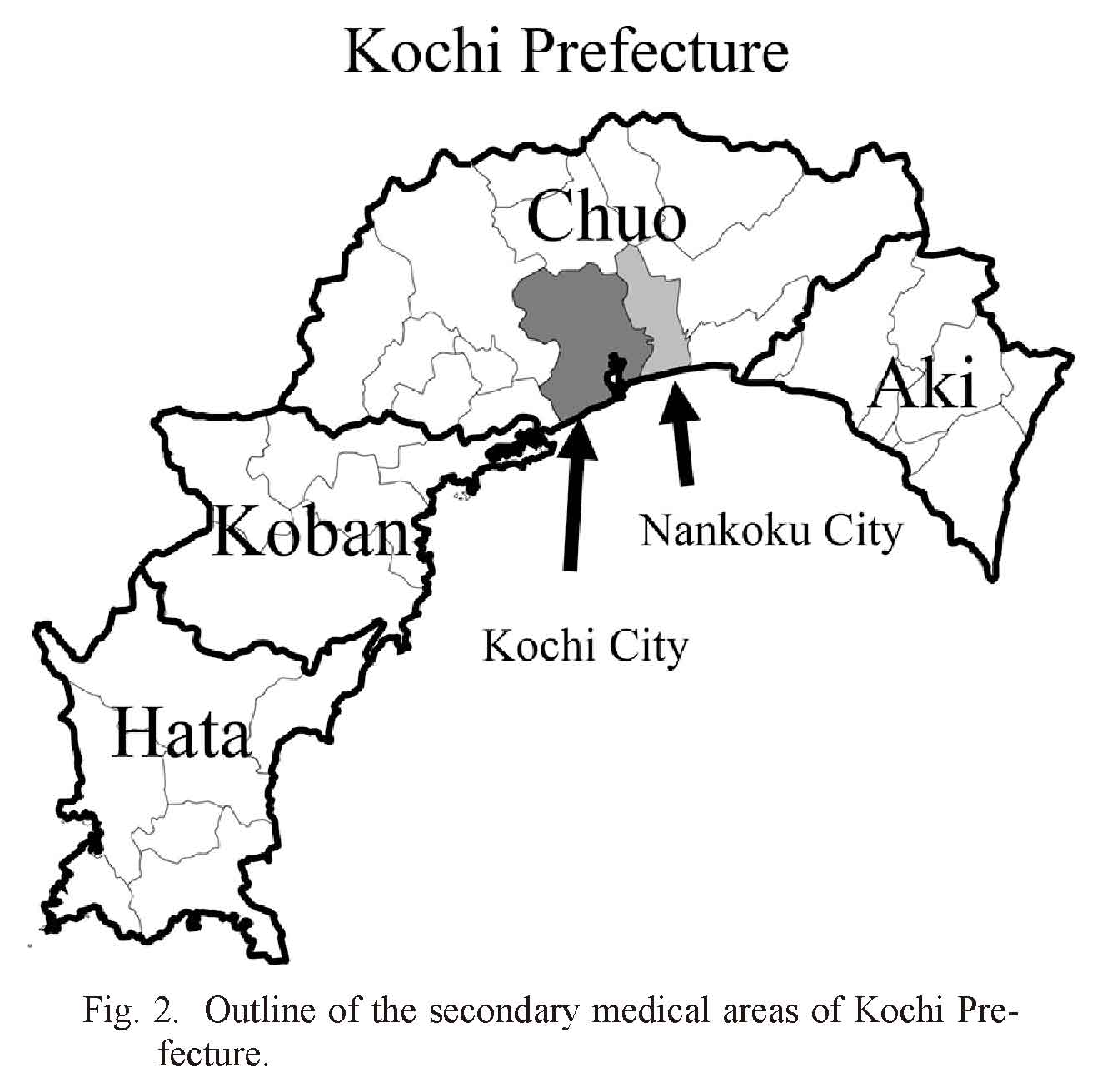
Outline of the secondary medical areas of Kochi Prefecture.
Kochi Prefecture is divided into 4 secondary medical areas. Kochi City (the prefectural capital) is located in the Chuo Medical Area.

Number of delivery facilities in the 4 secondary medical areas in Kochi Prefecture, including in Kochi City (which is located in the Chuo Medical Area).
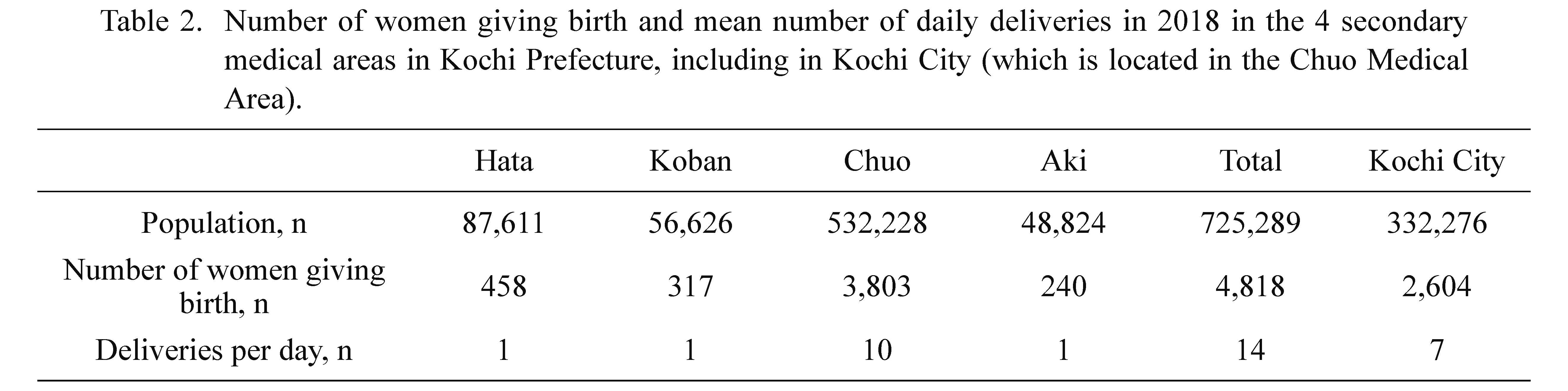
Number of women giving birth and mean number of daily deliveries in 2018 in the 4 secondary medical areas in Kochi Prefecture, including in Kochi City (which is located in the Chuo Medical Area).
1. Table shows means rounded to the nearest whole number.
2. Pregnant women in the Koban Medical Area give birth at delivery facilities in other medical areas.
Estimating the number of seriously injured and displaced pregnant women: The estimated number of pregnant women and seriously injured and displaced pregnant women is shown in Table 3. We estimated that in the entire Kochi Prefecture, there will be 32 seriously injured and 821 displaced pregnant women, the majority of whom will be in the Chuo Medical Area (23 seriously injured pregnant women and 685 displaced pregnant women). Most of the seriously injured and displaced pregnant women in the Chuo Medical Area will be in Kochi City.
Estimating the number of available beds for obstetrics and gynecology: The estimated number of available maternity beds is shown in Table 4. Immediately after an earthquake, the Chuo Medical Area is estimated to have 21 available maternity beds. That means that if 23 pregnant women are seriously injured, some may not be accepted in the hospital.

Estimated number of pregnant women and number of seriously injured and displaced pregnant women in the 4 secondary medical areas in Kochi Prefecture, including in Kochi City (which is located in the Chuo Medical Area; estimates are based on numbers from 2018).
Table shows means rounded to the nearest whole number.

Estimated number of available maternity beds in the 4 secondary medical areas in Kochi Prefecture, including in Kochi City (which is located in the Chuo Medical Area; estimates are based on numbers from 2018).
Our estimates showed that priority should be given to Kochi City and its surrounding areas because that is where the majority of seriously injured and displaced pregnant women will be located. Furthermore, after an earthquake, tsunamis may make it difficult to take the injured to medical institutions because of flooding in Kochi City and its surrounding areas (Fig. 3). Therefore, we subdivided Kochi City and the surrounding areas into 3 areas on the basis of how likely they are to be affected by tsunamis and the location of disaster base hospitals with delivery capabilities. We decided that pregnant women living in each of those areas will be allowed to visit a nearby disaster base hospital with delivery capabilities within the affected area, even if it is not their usual obstetrics and gynecology facility.

Tsunami flooding area and locations of delivery facilities in Kochi City and surrounding areas.
Kochi City and its surrounding areas are divided into 3 medical regions based on the location of disaster base hospitals and projected tsunami flooding areas. DLPPMs are allocated to disaster base hospitals in each area and also to the Disaster Medical Response Headquarters of Kochi Prefecture located in the prefecture government. The Kochi City tsunami hazard map and related data are available from Kochi City (https://kochi-kia.or.jp/wp-content/uploads/2020/03/aa326e3d3a6f4e01e0a644f6be2e3d7f.pdf).
Because a disaster such as a Nankai Trough earthquake is expected to cause enormous damage, cooperation and information-sharing among medical institutions may be delayed. Therefore, we designed the following system that will enable smooth cooperation between medical institutions: We asked at least one obstetrician or neonatal physician at the disaster base hospitals to complete DLPPM training for perinatal care during a disaster so that they can serve as key individuals in their respective area and coordinate the allocation of medical care (Fig. 3). Communication between Kochi City and the surrounding 3 areas, each secondary medical area, and the prefectural government will be coordinated by the DLPPM at the Kochi prefectural government, where the Disaster Medical Response Headquarters is located (Fig. 4). The DLPPM at the Kochi prefectural government will work closely with the disaster base hospital in the Koban Medical Area to collect information on pediatric and perinatal care in areas affected by a disaster, coordinate the necessary support, and make arrangements for transporting patients. The current DLPPM was commissioned by the prefectural governor to receive compensation for disaster-related activities.
Immediately after the onset of a disaster, medical care may be provided more slowly than usual. Therefore, we prepared a Disaster Management Manual and Action Cards for all facilities and distributed them so that these facilities can promptly handle situations according to their capabilities. This manual can be accessed on the internet (Kochi Prefecture 2020). After we established this plan, all facilities with delivery capabilities and the local government jointly conducted an on-site drill. Reviewing the issues identified during this drill allowed us to further improve our disaster preparedness with regard to perinatal care.

Disaster Medical Management System in Kochi Prefecture.
A liaison who supports the Disaster Medical Coordinator is allocated to the Disaster Medical Response Headquarters of Kochi Prefecture.
An earlier report discussed the necessity of building an area-wide medical care system in case of a disaster in Japan (Takahashi et al. 2018). However, no study has focused on the necessity of establishing an area-wide medical care system in case of disaster for post-disaster care of pregnant women. Perinatal care has limited medical resources, so area-wide disaster preparedness is needed to ensure effective support in large-scale disasters (Egawa et al. 2017). We estimated the number of affected pregnant women and requirement for perinatal medical care resources in each secondary medical area and then estimated the potential damage within the overall area, which enabled us to effectively design a detailed disaster response system. In addition, healthcare professionals and local governments discussed matters in collaboration, which helped speed up the process of improving disaster preparedness with regard to this population. Despite these successful efforts, we consider it important to repeat on-site disaster drills and have further discussions to fine tune disaster preparedness for perinatal care.
Discussion of the current status in Kochi Prefecture and our estimatesThe Chuo Medical Area is well equipped for providing perinatal care in ordinary times. However, immediately after a disaster, even the Chuo Medical Area is projected to have too few available beds for pregnant women. Shortly after the onset of a Nankai Trough earthquake, support will become extremely difficult across medical areas within the prefecture and between prefectures (Kochi Prefecture 2019). The lack of available maternity beds will mean that pregnant women, including those who are close to delivery, may need to be moved outside the prefecture. However, transporting patients outside the prefecture will cause significant economic burden and mental stress for family members (MHLW 2016a). Therefore, the ideal situation would be to provide medical care within the prefectural boundary.
The stress caused by disasters increases the rates of hypertensive disorders of pregnancy in the subsequent days and weeks compared with ordinary times (Kyozuka et al. 2020). Furthermore, pregnant women who are exposed to a disaster in their first trimester have a higher rate of preterm births (Torche and Kleinhaus 2012; Oyarzo et al. 2012). Both hypertensive disorders of pregnancy and preterm births require immediate attention, and we should assume that demand for treatment of these conditions may persist over a long period in the months after a Nankai Trough earthquake.
The current disaster preparedness measures alone are not sufficient to ensure that perinatal medical care is provided within Kochi Prefecture during a disaster. To increase the surge capacity of perinatal care, we believe that the best approach is to divide the roles among the facilities in the area. In the aftermath of the Great East Japan Earthquake, obstetric departments at disaster base hospitals and acceptable hospitals shortened the length of stay after deliveries and cesarean sections and accepted as many pregnant women as possible. The majority of maternity clinics and midwifery homes were unable to perform deliveries (Sugawara et al. 2016), but they were able to provide postpartum care (MHLW 2016b). If the length of stay after deliveries are shortened, we can assume that many postpartum mothers would not be able to receive guidance on childcare and would have higher anxiety levels after evacuation. To avoid this problem, we believe that disaster base hospitals with delivery capabilities should provide deliveries and perform cesarean sections and that mothers should be transferred to maternity clinics and midwifery homes for postpartum care. In addition, to achieve self-sufficiency within the prefecture, we need to secure additional healthcare staff for perinatal care, provide material support to delivery facilities (including stockpiling of emergency equipment), and locate facilities in earthquake-resistant buildings. Moreover, we need to prepare a system for accepting both material and human resources to ensure early recovery and long-term support in the case of a disaster.
Establishment of a disaster medical management system in the Chuo Medical Area based on estimates of damage and use of DLPPMsIn past disasters, information about perinatal care was not shared across an overall disaster medical system, which resulted in delays in providing medical support (MHLW 2016b). Therefore, in 2016, the MHLW established the position of a DLPPM. However, detailed measures have not yet been finalized on how best to deploy the DLPPMs after they are trained.
On the basis of our estimates, we subdivided Kochi City and the surrounding areas into 3 areas by considering the likelihood that the areas would be affected by tsunamis and the location of disaster base hospitals with delivery capabilities. Furthermore, we considered that obstetricians or pediatricians with DLPPM training who normally work in the disaster base hospitals will act as DLPPMs in case of a disaster. A DLPPM will be present in a disaster base hospital in each area and in the Disaster Medical Response Headquarters of Kochi Prefecture (Fig. 3). Thus, information about pregnant women will be effectively collected and shared through the overall disaster medical management system. We believe that we have formulated a specific plan for effective allocation and management of DLPPMs. In 2019, the MHLW notified each prefectural government in Japan about nominating DLPPMs and implementing activities similar to those in Kochi Prefecture (MHLW 2019). We anticipate that this notification, together with the present report, will encourage additional prefectures to implement a system for supporting pregnant women during a disaster.
This study has some limitations. The previous Nankai Trough earthquake occurred in Kochi Prefecture in 1946, and the medical system has greatly evolved since then, making it difficult to prepare for future disasters on the basis of the situation and actions taken at that time. Moreover, we made projections and conducted a drill for putative disasters, but these measures have not been validated through actual disasters. This report focuses on pregnant women; however, we need to consider also a comprehensive support system for other vulnerable groups that need special consideration during disasters, such as children who require constant medical care and a parenting support system, as well as older and disabled people.
In conclusion, we found it quite challenging to plan our disaster preparedness measures because we were preparing for events that have not yet occurred. Nevertheless, estimating the expected number of seriously injured and displaced pregnant women together with the number of available maternity beds is an effective way to prepare realistic disaster measures. These estimations enabled us to formulate a specific plan for effective allocation and management of DLPPMs. We believe that our system can be an initiative model in perinatal disaster medicine.
The authors sincerely thank the healthcare professionals who were involved in the preparation of these disaster preparedness measures for perinatal care in Kochi Prefecture and the local government staff.
The authors declare no conflict of interest.