2022 Volume 257 Issue 1 Pages 65-71
2022 Volume 257 Issue 1 Pages 65-71
Disruption of cancer screening programs and diagnoses of gastrointestinal cancers by the COVID-19 pandemic has been reported; however, little attention has been paid to the situation in depopulated areas with low infection rates. Akita Prefecture is one of the most depopulated areas of Japan and has the lowest COVID-19 infection rate per capita; at the same time, the prefecture has been top-ranked for mortality due to gastrointestinal cancer for years. In this population-based study in Akita Prefecture, we investigated the occurrence of gastrointestinal cancers and the number of cancer screening procedures over the five-year period of 2016-2020, employing a database from the collaborative Akita Prefecture hospital-based registration system of cancers. The occurrence of gastrointestinal cancers, especially esophago-gastric cancers, declined by 11.0% in 2020, when the COVID-19 pandemic affected the overall healthcare system, compared with the average of 2016-2019. Nonetheless, the occurrence of advanced-stage (stage IV) esophago-gastric cancers increased by 7.2% in 2020. The decrease in the gastrointestinal cancer diagnosis rate in 2020 coincided with a 30% decline in the total number of regular population-based screening programs. Under the ongoing COVID-19 pandemic, cancer screening was uniformly suspended throughout Japan. Accordingly, the COVID-19 pandemic has substantially disrupted the cancer screening system, leading to delays in diagnoses of gastrointestinal cancer, even in depopulated areas (Akita Prefecture) of Japan with a low prevalence of infection. Suspension of cancer screening procedures during an infectious disease pandemic should be thoroughly considered for each region based on the cancer incidence and infection status in that area.
Coronavirus disease-2019 (COVID-19) was first identified in December 2019 in Wuhan, China and has subsequently spread worldwide, leading to an ongoing global pandemic. The COVID-19 pandemic has placed a serious burden on the overall healthcare system, not just the resources for directly treating COVID-19. For example, the pandemic has been associated with decreased diagnostic rates of some life-threatening diseases, such as acute heart failure and stroke, probably due to policies prioritizing COVID19-related treatment over other issues (Siegler et al. 2020; Colivicchi et al. 2020). Furthermore, recent studies have shown that the COVID-19 pandemic has resulted in a substantial decrease in diagnoses of gastrointestinal (GI) cancer in association with a decreased number of endo scopic procedures (Lui et al. 2020; Dinmohamed et al. 2020; Khan et al. 2021; Rutter et al. 2021).
In Japan, the first state of emergency to prevent the spread of COVID-19 infection was declared on April 7, 2020, in seven prefectures, mainly densely populated areas with a high number of infected patients. On April 16, 2020, the state of emergency was expanded to the whole country (47 prefectures) and lasted for approximately 1 month, until May 14, 2020, when the state of emergency was lifted in 39 prefectures, followed by total cancelation of the state of emergency for the whole country on May 25, 2020. Since then, another two states of emergency have been declared (second from January 7 to March 18, 2021; third from April 23 to September 28, 2021) for up to 21 prefectures, again mainly in densely populated areas. In general, the infection rates are higher in densely populated areas than in depopulated ones in Japan, probably due to more close contact with residents in the more densely populated areas.
During the state of emergency, especially the first one, Japan’s Ministry of Health, Labour and Welfare encouraged the suspension of cancer screenings under the principle of prioritizing COVID-19-related treatment and preventing the spread of the infection (The Japanese Society of Gastrointestinal Cancer Screening 2020). Thus, cancer screening was uniformly suspended throughout the country, regardless of regional infection status. Notably, some studies from a single or a few institutes in Japan reported a decreased incidence of GI cancer diagnoses during the pandemic in densely populated areas with highly prevalent infection (Mizuno et al. 2020; Kuzuu et al. 2021). Furthermore, a recent nationwide survey also demonstrated a decreased incidence of GI cancer diagnoses in Japan during the pandemic (National Cancer Center Japan 2021a); however, little attention has been paid to the situation in depopulated areas with relatively low COVID-19 infection rates.
Akita Prefecture is located in the northern region of Honshu, the main island of Japan, and has a population of approximately 1 million. The economy of Akita Prefecture is dominated by traditional industries, such as agriculture, fishing, and forestry. Thus far, Akita Prefecture has shown the lowest COVID-19 infection rate per population among all 47 prefectures (NHK 2021) and has not been an area subject to a state of emergency aside from the first instance that covered the whole country. Noticeably, at the same time, Akita Prefecture has been ranked top in mortality due to the three major GI cancers (esophageal, gastric, and colorectal) in Japan for a number of years (National Cancer Center Japan 2021b).
To clarify the effect of the COVID-19 pandemic on the diagnosis of GI cancers in a depopulated region like Akita Prefecture, we investigated the occurrence of GI cancers and the numbers of cancer screening procedure in the overall population of the area over the five-year period between 2016 and 2020.
In this analysis, we used the database from the collaborative Akita Prefecture hospital-based registration system of cancers, in which all 11 cancer treatment base hospitals located in Akita Prefecture participated (Koizumi et al. 2018a, b). Overall, these 11 hospitals cover 81.0% of treatments for cancers occurring in the prefecture (National Cancer Center Japan 2021c). Using this registration system, we examined the occurrence and stage of GI cancers (e.g., esophageal, gastric, and colorectal cancer) in 2016- 2020 in Akita Prefecture. As a reference, we also examined the occurrence of hepato-biliary-pancreatic (HBP) cancers using the same registration system during the same period. In addition, data on the number of esophagogastroduodenoscopies and colonoscopies performed at the 11 hospitals were collected.
With the aid of two exclusive institutes managing cancer screening procedures in Akita Prefecture (Akita Foundation for Healthcare, and The Akita Prefectural Federation of Agricultural Cooperatives for Health and Welfare), we collected data on the number of GI cancer screening procedures (upper GI series with barium meal and fecal occult blood test) performed in 2019 and 2020 in Akita Prefecture. Since endoscopic screening for gastric cancers in place of radiological screening started in 2021 in Akita Prefecture, the introduction of the new screening approach did not affect the current outcomes.
The data from 2020 (during COVID-19 pandemic) were compared with the previous four-year (2016-2019) average and expressed as a percent change in cancer occurrence. In the analysis, the occurrence of esophageal and gastric cancers was combined as esophago-gastric cancer, as both cancers are detected by the same screening procedure (upper GI series with barium meal) and the subsequent detailed examination (esophagogastroduodenoscopy). Because the number of stage II and III cases for each cancer was relatively small, these were summed for stage-specific comparisons. Regarding the detection process, the proportions of esophago-gastric and colorectal cancers detected through screening procedures (official cancer-screening programs plus private health checkups) were determined. The subject age was expressed as the mean and standard deviation (SD) and compared using Student’s t-test. Sex was expressed as the number and proportion and compared using the chi-square test. P values of < 0.05 were considered statistically significant. This analysis was approved by the Akita University School of Medicine Ethics Committee (2796).
All cases with neoplasias newly identified during the study period were extracted from the database according to the occurrence sites. For each site of neoplasia, the mean age at the diagnosis was significantly older in 2020 than in 2016-2019 [73.4 (9.1) vs. 71.6 (9.1) years old, P < 0.01 for esophagus; 74.5 (10.1) vs. 73.3 (10.3) years old, P < 0.01 for stomach; 71.9 (11.4) vs. 71.1 (11.5) years old, P < 0.02 for colorectum; and 76.3 (11.2) vs. 75.3 (10.5) years old, P < 0.02 for liver, bile duct, and pancreas; mean (SD)], probably due to the aging of the population in the area. However, the sex ratio did not change significantly between 2016-2019 and 2020 for any sites (Table 1). The vast majority of these cases (more than 97%) were cancers for each site, and further analyses were performed using data of cancers alone.
Annual changes in the numbers of each cancer in 2016-2020 are shown in Table 2. Overall, the annual occurrence of GI plus HBP cancers was 3,873 in Akita Prefecture in 2016-2019 on average, slightly decreasing by 3.5% to 3,739 in 2020. However, the change in the occurrences in 2020 varied depending on the cancer site, as described below (Table 3).
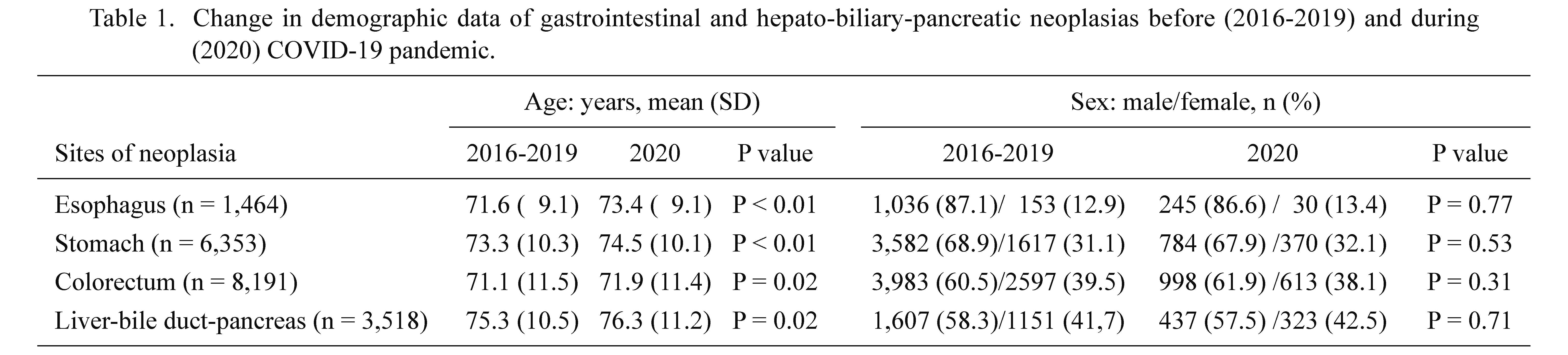
Change in demographic data of gastrointestinal and hepato-biliary-pancreatic neoplasias before (2016-2019) and during (2020) COVID-19 pandemic.

Annual changes in the numbers of diagnosed gastrointestinal and hepato-biliarypancreatic cancers in 2016-2020.

Change in the numbers of diagnosed gastrointestinal and hepato-biliary-pancreatic cancers before (2016-2019) and during (2020) COVID-19 pandemic.
The occurrence of diagnosed esophago-gastric cancers declined by 11.0% from an average of 1,569 in 2016-2019 to 1,396 in 2020. The decrease in the occurrence was particularly marked for early- (stage 0 or I) and middle-stage (stage II or III) esophago-gastric cancers, declining by 13.0% and 26.2% in 2020 compared with the respective average of 2016-2019. However, of note, the occurrence of advanced-stage (stage IV) esophago-gastric cancers in 2020 was increased by 7.2% compared with the average of 2016- 2019. The proportion of esophago-gastric cancers detected through screening procedure was 15.4% in 2016-2019, decreasing to 13.3% in 2020.
Colorectal cancersThe annual occurrence of colorectal cancers in 2020 also declined, but to a lesser extent (only 2.0%), from an average of 1616 in 2016-2019 to 1585 in 2020. Regarding stage-specific comparisons, the greatest decline in 2020 was observed for early-stage (stage 0 or I) cancer (by 5.3%). The proportion of colorectal cancers detected through screening procedures was 16.5% in 2016-2019, increasing slightly to 17.1% in 2020.
HBP cancersIn contrast with the above-mentioned GI cancers, the annual occurrence of HBP cancers actually increased by 9.0%, from an average of 687 in 2016-2019 to 758 in 2020. Regarding stage-specific comparison, the occurrence of HBP cancers increased in 2020 both at the early stage (stage 0 or I) and most advanced stage (stage IV) — by 7.3% and 8.8%, respectively.
Cancer screeningThe numbers of both GI cancer screening procedures (upper GI series with barium meal and fecal occult blood test) performed in Akita Prefecture were lower in 2020 than in 2019. The number of upper GI series declined by 30.3%, from 64,055 in 2019 to 44,670 in 2020. Similarly, the number of fecal occult blood test decreased by 29.1%, from 86,181 in 2019 to 61,099 in 2020 (Fig. 1). As reference data, the recall rates (number of subjects instructed close examination by endoscopy) for upper GI series performed by Akita Foundation for Healthcare were 6.5% (n = 48,883) in 2019 and 6.8% (n = 40,661) in 2020, respectively.

Change in the number of gastrointestinal cancer screening procedures performed in Akita Prefecture before (2019) and during (2020) COVID-19 pandemic.
The total numbers of both esophagogastroduodenoscopy and colonoscopies performed at the 11 cancer treatment base hospitals in Akita Prefecture were lower in 2020 than in 2019, and the magnitude was more pronounced in the esophagogastroduodenoscopies than in the colonoscopies. The number of esophagogastroduodenoscopies decreased by 18.0% (from 42,433 to 34,793), while the number of colonoscopies decreased by 7.8% (from 19,362 to 17,844) (Fig. 2).

Change in the total number of endoscopic examinations performed at the 11 cancer treatment base hospitals located in Akita Prefecture before (2019) and during (2020) the COVID-19 pandemic.
This population-based study in Akita Prefecture demonstrated that the occurrence of GI cancers, especially esophago-gastric cancers, declined in 2020, when the COVID-19 pandemic affected the overall healthcare system, compared with 2016-2019 (pre-COVID-19 era). Furthermore, the decrease in the GI cancers in 2020 coincided with a decline in the total number of regular population- based screening programs provided by the local governments in the same area. Thus, since cancer-screening programs are executed for the early detection of GI cancers in asymptomatic residents, the decreased number of screening procedures may be at least partly responsible for the decline in the occurrence of GI cancer diagnoses, especially for earlier-stage GI cancers, in Akita Prefecture. The potential causal relationship between the decrease in occurrence of GI cancers and the decrease in cancer screening procedures may also be supported by a lack of a decrease in the occurrence of HBP cancers in 2020, for which there is no approved screening program.
A recent nationwide survey in Japan demonstrated that the occurrence of GI cancer diagnoses decreased in 2020 due to the COVID-19 pandemic, especially for gastric cancers. Indeed, the occurrence of gastric cancer decreased by 11.3% in men and 12.5% in women in 2020 compared with the average for the last 4 years (2016-2020), while that of colorectal cancers decreased by 6.8% in men and 5.5% in women in 2020 (National Cancer Center Japan 2021a). Consistently, using the same average (2016-2019) as a reference, the occurrence of esophago-gastric cancers decreased by 11.0% and that of colorectal cancers by 2.0% in the current population-based survey in Akita Prefecture. However, recent studies in Japan have shown little to no effect of the COVID-19 pandemic on the occurrence of HBP cancer diagnoses (Kuzuu et al 2021; National Cancer Center Japan 2021b). Consistently, the current study also revealed that the occurrence of HBP cancers did not decrease at all (and actually increased, by 9.0%) in 2020. Unlike GI cancers, many of which are detected by screening examinations for asymptomatic subjects, HBP cancers are generally detected on the appearance of symptoms, such as abdominal pain, jaundice, weight loss, and new-onset diabetes. The temporal increasing trend observed in HBP cancers (Table 2) may be responsible for the relative increase in 2020 compared with 2016-2019.
Initially, the Japan Cancer Association reported that the number of population-based cancer screenings in May 2020 sharply decreased to approximately 10% of that in May 2019 (Toyoda et al. 2021). This massive decrease was caused by the encouragement of the Ministry of Health, Labour and Welfare to suspend cancer screening activities, especially during the first state of emergency, throughout the country. Subsequently, although the number of screening procedures was gradually restored in the second half of 2020, it was difficult to compensate for the previous decrease, and the Association eventually reported an annual overall 30% decrease in cancer screening in 2020 compared with the previous year (2019) (Japan Cancer Society 2021). Consistently, we found an approximately 30% of decrease in the total number of stomach and colorectum cancer screening examinations performed in 2020 in Akita Prefecture. The small reduction in GI cancer diagnoses relative to corresponding cancer screening examinations (e.g., 10% vs. 30% in esophagogastric cancers) may be explained by the fact that only a small portion (approximately 10%- 15%) of GI cancers are detected by screening programs.
Utilizing the data on the occurrence of GI cancers as well as the number of screening procedures for the overall population of the defined area, the current study demonstrated that while the number of screening procedures for esophago-gastric and colorectal cancers decreased by the same degree (approximately 30%), the decrease in the occurrence of cancers was more pronounced for esophagogastric cancers than for colorectal cancers. The predominant decrease in esophago-gastric cancers relative to colorectal cancers is consistent with the above-mentioned nation-wide survey (National Cancer Center Japan 2021a). The temporal declining trend in gastric cancer in contrast to that of colorectal cancers in Japan (Table 2) may partly explain the somewhat discordant outcomes between the two types of cancers. Alternatively, although endoscopic examinations (esophagogastroduodenoscopy or colonoscopy) with a biopsy are the ultimate modality for diagnosing GI cancers, irrespective of the prior execution of a cancer screening program, such examinations were also recommended to be suspended during the pandemic (Irisawa et al. 2020). In Japan, esophagogastroduodenoscopy is performed several times more frequently than colonoscopy (Furuta et al. 2016); therefore, the suspension of endoscopic examinations during the pandemic may more profoundly affect the diagnoses of esophago-gastric cancer than of colorectal cancer. In addition, this study showed that the number of esophagogastroduodenoscopies performed in the 11 participating hospitals decreased more markedly during the pandemic (2020) than did colonoscopies (18.0% vs. 7.8%). Although COVID-19 is considered to be transmitted mainly through aerosol contamination, esophagogastroduodenoscopy, which involves passing an instrument through the nasal and oral cavities, is more likely to induce coughing and subsequent emission of droplets and thereby increase the risk of exposure of medical staff to aerosol contamination than colonoscopy (Irisawa et al. 2020). This may have contributed to the more marked suspension of esophagogastroduodenoscopy than colonoscopy during the pandemic.
These disruptions of the healthcare system for detecting GI cancers due to the pandemic are expected to cause similar delays in the diagnosis of such cancers, ultimately resulting in an excess of advanced cancer diagnoses and deaths in the coming years (Dinmohamed et al. 2020; Maide 2020). Of note, such concerns may have already manifested in 2020, since the current study indicated that the number of esophago-gastric cancers diagnosed at the most advanced stage (stage IV) increased in 2020 by 7.2%, while the total number of cancer diagnoses declined by 11.0%. A recent study using a simulation model found that 4.6% of patients with gastric cancer will have a higher stage at their diagnosis, shifting in response to the 6-month delay due to the COVID-19 pandemic (Lui et al. 2020). Thus, the severe disruption of the healthcare system in the first half of 2020 may be responsible for the increase in stage IV esophago- gastric cancers in 2020 as a whole. We need to watch this trend carefully in the coming years, when the impact of delayed diagnoses is likely to become more apparent.
The strength of this study is its population-based nature and inclusion of the total number of GI cancer diagnoses and cancer screening procedures executed in Akita Prefecture. Such a study is important for investigating temporal trends in diseases, as the extent of the disturbance of the healthcare system by the pandemic may differ among hospitals, so the number of cancer occurrences would fluctuate in a hospital-based study (Mizuno et al. 2020; Kuzuu et al. 2021).
Several limitations associated with the present study warrant mention. First, although the number of endoscopic examinations performed at the 11 cancer treatment base hospitals was counted in this study, it did not include procedures performed in other medium-sized hospitals and clinics. The precise total number of such examinations performed in our area therefore could not be determined. Although this study demonstrated a more pronounced decrease in the number of esophagogastroduodenoacopies than in colonoscopies during the pandemic, which may be partly responsible for the more pronounced decrease in esophagogastric cancer diagnoses than colorectal cancer diagnoses, these findings need to be confirmed in a nationwide study. Second, although this study showed the proportion of cancers detected through screening procedures, it included official cancer-screening programs as well as private health checkups, which may have offered screening endoscopy. Thus, we were unable to precisely estimate the contribution of cancer-screening programs to the diagnosis of cancers.
Under the COVID-19 pandemic, cancer screening was uniformly suspended all over Japan, especially during the first state of emergency. However, when considering the suspension of cancer screening during infectious disease pandemics in the future, we may need to consider the merits and demerits of such a notion. While the suspension of screening may help prevent the spread of the infectious disease (merit), the suspension can negatively affect the diagnosis of GI cancers (demerit). In this study, we found that the disruption of cancer screening programs and diagnosing GI cancers in a depopulated area as Akita Prefecture, findings similar to a recent nation-wide survey in Japan (National Cancer Center Japan 2021a; Japan Cancer Society 2021). Nonetheless, the current findings provide additional implications, derived from two unique characteristics of Akita Prefecture.
First, since Akita Prefecture has always been topranked for mortality due to the three evaluated GI cancers (esophageal, gastric, and colorectal cancers) (National Cancer Center Japan 2021b), the demerits of suspending GI cancer screening should be considered to have greater weight than in other areas. Second, the rate of COVID-19 infection tends to be lower in depopulated areas, and this is true for Akita Prefecture, one of the least populated areas of Japan. Indeed, the number of new COVID-19 infections per capita was the lowest in the country in Akita Prefecture (NHK 2021). Consequently, the merits of suspending cancer screening to prevent the spread of infection are likely to have very little weight in this area. Given these characteristics of this prefecture, the ratio of demerits relative to merits associated with the suspension of cancer screening is expected to be extremely high in Akita Prefecture. Although cancer screening has been uniformly suspended throughout the country during the current COVID-19 pandemic, we propose that suspending cancer screening during an infectious disease pandemic should be decided on a region-by-region basis, depending on the cancer incidence and infection status in that area. Furthermore, in addition to the decision of the screening facility itself, the behavior of screenees is important to consider in order to ensure uninterrupted cancer screening procedures during a pandemic (Toyoda et al. 2021). Local governments should therefore recommend that their residents receive cancer screening properly, even during a pandemic.
In conclusion, the COVID-19 pandemic substantially disrupted the cancer screening system, leading to delays in diagnosing GI cancers, even in depopulated areas of Japan with a low prevalence of infection. Deciding whether or not cancer screening procedures should be suspended during an infectious disease pandemic should be made on a region-by-region basis, depending on the cancer incidence and infection status in that area. In addition, to what extent the decreased number of endoscopies during the pandemic contributed to the decreased number of gastrointestinal cancer diagnoses in Japan needs to be clarified by a nationwide survey.
We appreciate the following collaborators in Akita, Japan for collecting the clinical data. Kiyonori Yamai (Odate Municipal General Hospital), Yuko Fujishima (Noshiro Kosei Medical Center), Takuma Ajimine (Northern Akita Municipal Hospital), Hidehiko Tsuda (Akita Kousei Medical Center), Tsuyotoshi Tsuji (Akita City Hospital), Hiro-o Matsushita (Akita Red Cross Hospital), Kengo Onochi (Omagari Kosei Medical Center), Yohei Horikawa (Hiraka General Hospital), Takahiro Dohmen (Yuri Kumiai General Hospital).
The authors declare no conflict of interest.