2022 年 257 巻 2 号 p. 153-156
2022 年 257 巻 2 号 p. 153-156
Eosinophilic gastrointestinal disorders (EGIDs) cause various gastrointestinal symptoms due to infiltration of eosinophils into the gastrointestinal tract. Helicobacter pylori (H. pylori) is a microorganism that is associated with various diseases such as autoimmune diseases. In recent years, H. pylori is considered protective in inflammatory bowel diseases and gastrointestinal autoimmune disorders but is not known to be protective in EGIDs. A 14-year-old boy presented with epigastric pain and nausea, without diarrhea. His symptoms were not associated with meals. Blood examination showed an eosinophil count of 1,666 cells/µL (17.0%) and an interleukin-5 (IL-5) level of less than 3.9 pg/mL. Esophagogastroduodenoscopy showed chronic gastritis and duodenal ulcers. Capsule endoscopy and colonoscopy showed no abnormal findings. The patient was diagnosed with chronic gastritis due to H. pylori infection and eosinophilic duodenal ulcers. H. pylori eradication was performed. However, the abdominal pain worsened with elevated peripheral eosinophil count [2,314/µL (26%)] and serum IL-5 level (8.0 pg/mL). Montelukast administration improved the symptoms and laboratory findings [peripheral eosinophil count, 330/µL (5.9%); IL-5, < 3.9 pg/mL]. EGIDs should be considered as a cause of duodenal ulcers. H. pylori may be protective in EGIDs. Montelukast monotherapy may be considered as a first line treatment for eosinophilic duodenal lesions.
Eosinophilic gastrointestinal disorders (EGIDs) cause various gastrointestinal symptoms, such as abdominal pain, due to infiltration of eosinophils into the gastrointestinal tract. EGIDs have been classified into eosinophilic esophagitis and eosinophilic gastroenteritis (Kinoshita et al. 2019). Helicobacter pylori (H. pylori) is a microorganism that is associated with various diseases such as malignant and autoimmune diseases. Herein, we describe a pediatric case of eosinophilic duodenal ulcer exacerbation after H. pylori eradication.
A 14-year-old boy presented with epigastric pain and nausea for 4 months, without diarrhea or weight loss. His symptoms were not associated with meals. He had bronchial asthma and allergic rhinitis. He had no atopic dermatitis or food allergies. Blood examination showed a white blood cell count, 9,800 cells/µL; eosinophil count, 1,666 cells/µL (17.0%); serum levels of albumin, 4.7 g/dL; C-reactive protein, < 0.01 mg/dL; immunoglobulin (Ig) G, 1,280 mg/dL; IgA, 139.6 mg/dL, IgM, 104.4 mg/dL, total IgE, 347 IU/L (reference range < 173 IU/mL); specific IgE antibody to the following: egg white, 2.09 IU/L; milk, 0.56 IU/L; wheat, 0.30 IU/L; soy, 15.4 IU/L; rice, 0.14 IU/L; peanut, 1.32 IU/L; shrimp, 5.05 IU/L; and salmon, 0.17 IU/L; thymus and activation-regulated chemokine, 1,076 pg/mL (reference range < 743 pg/mL); and negative for myeloperoxidase- and proteinase3-antineutrophil cytoplasmic antibodies. Fecal examination was negative for the fecal immunochemical test, eosinophils, and parasite eggs. Abdominal ultrasonography showed no abnormal findings.
Esophagogastroduodenoscopy (EGD) showed superficial gastritis and multiple duodenal ulcers (Fig. 1A, B), but no abnormal findings in the esophagus. A rapid urease test was positive. Pathological examination showed up to 65 cells per high-power field of eosinophil infiltration into the duodenum (Fig. 1C). The degree of eosinophil infiltration in the esophagus and the stomach was insufficient to meet the diagnostic criteria for an EGID. Colonoscopy showed no endoscopic or pathological findings from the terminal ileum to the rectum. Capsule endoscopy revealed no abnormal findings in the jejunum and ileum. The patient was diagnosed with chronic gastritis due to H. pylori infection and eosinophilic duodenal ulcers.
Clarithromycin, amoxicillin, and proton pump inhibitors (PPIs) were administered for H. pylori eradication at week 0 (Fig. 2). Histamine 1 receptor antagonist (H1RA) was administered at week 1 because the patient had Japanese cedar pollinosis symptoms. Epigastric pain worsened at week 2; the peripheral eosinophil count was elevated further (2,312 cells/µL, 26%). Montelukast was added at week 3, and there was improvement in epigastric pain at week 4. PPI was discontinued at week 11, and urea breath test results were negative at week 12. However, nausea reappeared at week 12, and PPI was recommenced. The peripheral eosinophil count decreased to 330 cells/µL (5.9%) at week 19. EGD revealed no abnormal findings in the stomach but scarring of the duodenal ulcers were present (Fig. 1D).
Serum interleukin (IL)-5, an eosinophil-inducing cytokine, was measured at the time of diagnosis, after H. pylori eradication, and upon administration of montelukast (Fig. 2). Serum IL-5 increased to 8 pg/mL (reference range < 3.9 pg/mL) after H. pylori eradication although serum IL-5 was not detected at the time of diagnosis. Serum IL-5 improved to < 3.9 pg/mL with an improvement in peripheral eosinophil count after treatment.
Informed consent to publish this case report was obtained from the patient’s parent.
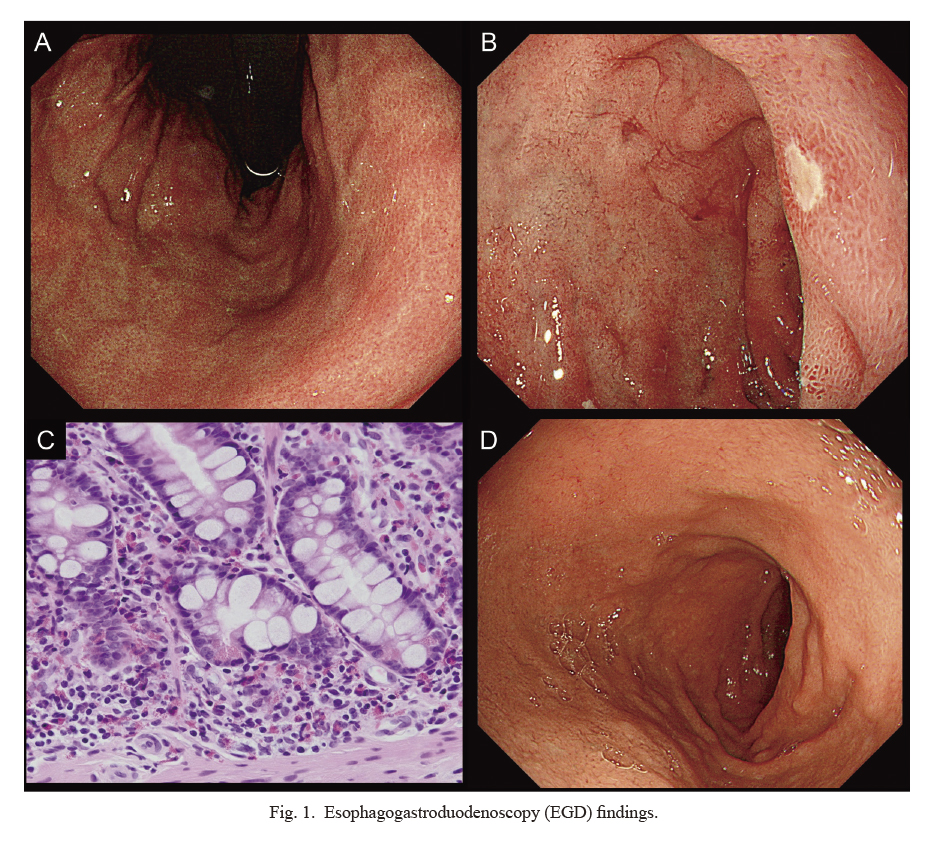
Esophagogastroduodenoscopy (EGD) findings.
At the time of diagnosis, EGD revealed superficial gastritis (A) and a duodenal ulcer (B). Pathological examination showed eosinophil infiltration of 65 cells per high power field in duodenum (original magnification, × 400) (C). After H. pylori eradication and EGID treatment, EGD revealed scarring of the duodenal ulcer (D).
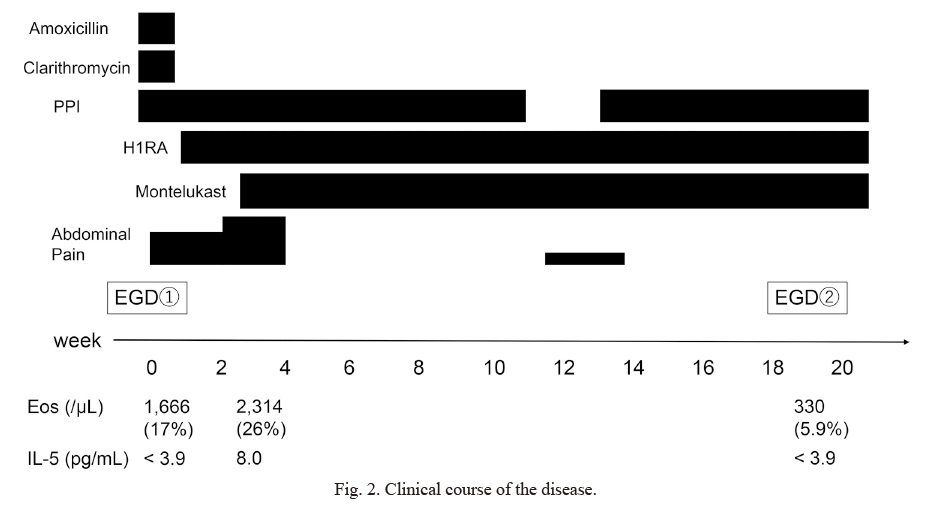
Clinical course of the disease.
H. pylori eradication worsened the abdominal pain and increased the proportion of eosinophils and serum interleukin-5. Montelukast improved the clinical symptoms, laboratory findings, and endoscopic findings.
EGD, esophagogastroduodenoscopy; Eos, eosinophil; H1RA, histamine 1 receptor antagonist; IL-5, interleukin-5; PPI, proton pump inhibitor.
EGIDs presenting with duodenal ulcers are rare, especially in children (Markowitz et al. 2000; Kubo et al. 2020), and may cause perforations (Deslandres et al. 1997; Riggle et al. 2015). In this patient, the duodenal ulcers were considered to have been caused by H. pylori infection, but the symptoms did not improve even after H. pylori eradication, and the peripheral blood eosinophil level remained high. The duodenal ulcers were thought to be caused by EGID. Pediatricians should, therefore, also consider EGIDs as a differential diagnosis of duodenal ulcers.
There are few reports regarding EGIDs complicated by H. pylori infection (Papadopoulos et al. 2005; Nakamura et al. 2014). H. pylori eradication may or may not be effective for EGIDs, and effectiveness is not consistent. Patients with EGIDs have a significantly lower proportion of H. pylori than individuals without EGIDs, suggesting that H. pylori may be protective for EGIDs (Furuta et al. 2013). The same has also been reported in inflammatory bowel diseases (IBD) such as ulcerative colitis (UC) and Crohn’s disease (Sonnenberg and Genta 2012; Castano-Rodriguez et al. 2017). We reported a pediatric case with UC that relapsed after H. pylori eradication, indicating that H. pylori may also be protective in IBD (Fujita et al. 2021). Zhang et al. (2018) reported that H. pylori had a protective role in mice with chronic experimental colitis; H. pylori colonization increased regulatory T cells and IL-10 whilst suppressing IL-17-producing effector T-helper cells.
Whether to start with H. pylori eradication or treatment for EGIDs in these patients is unclear. In our patient, abdominal pain worsened after H. pylori eradication. As previously mentioned, H. pylori may be protective for EGIDs, and thus, eradication may have caused aggravation. However, H. pylori reduces gastric acid secretion (El-Omar et al. 1997), and it is possible that the increase in gastric acid secretion due to eradication exacerbated his abdominal pain attributed to the duodenal ulcer. Generally, if a duodenal ulcer due to H. pylori infection is diagnosed, we firstly treat it with medication, such as PPI, and proceed to H. pylori eradication therapy after the ulcer is healed. Even in cases for which the diagnosis is a duodenal ulcer due to eosinophilic infiltration, as in our patient, it appears optimal to procede with standard treatment for an eosinophilic duodenal ulcer.
Systemic corticosteroids are generally considered effective as a treatment for EGIDs, but long-term use leads to various adverse events. Systemic corticosteroids must be used appropriately, especially in children, considering disease severity. Various drug therapies have been tried, including immunosuppressants (other than corticosteroids), antihistamines, leukotriene receptor antagonists, antacids, and biological agents.
The effectiveness of montelukast, a leukotriene receptor antagonist, for EGIDs with duodenal lesions was shown in a double-blind, randomized, placebo-controlled cross-over study (Friesen et al. 2004). In addition, there are several case reports in which montelukast monotherapy was effective as a first line treatment (Neustrom and Friesen 1999; El-Alali et al. 2021). Montelukast is a medication associated with few adverse events and may be considered for use before corticosteroids, especially in cases with duodenal lesions. Montelukast was considered effective in this patient because the symptoms improved promptly after its initiation, and peripheral blood eosinophil count also decreased. Although the symptoms and peripheral blood eosinophil count increased with the eradication of H. pylori, PPI use is thought to have some effect considering the slight worsening in abdominal pain after its discontinuation. It is not clear whether this is the effect of PPI alone or the effect of using it in combination with montelukast or H1RA.
IL-5 is one of the most important cytokines in EGIDs (Hogan et al. 2001). Serum IL-5 was measured at three points in this patient: at the time of diagnosis, after H. pylori eradication, and after montelukast treatment. IL-5 levels were beneath measurement sensitivity at the time of diagnosis but elevated after H. pylori eradication; the eosinophil count was also elevated.
This case report has some limitations. We did not perform endoscopy at the time of worsening in abdominal pain after eradication, and the biopsy was not taken from the duodenum after the healing of the ulcer. Further, we were unable to make a histological evaluation of whether the eosinophil infiltration exacerbated or improved. This case report included only one pediatric case, and thus, it is unclear whether the symptoms and laboratory findings (peripheral eosinophils and serum IL-5) are due to increased gastric acid secretion by H. pylori eradication or immunological effects. Further research on the role of H. pylori in EGID is needed.
In conclusion, EGIDs should be considered as a cause of duodenal ulcers, even with H. pylori infection. H. pylori eradication should be carefully considered if EGID is complicated. Montelukast may be used before corticosteroids, especially in EGIDs with duodenal lesions.
We would like to thank Editage (https://www.editage.com) for English language editing.
Dr. Fujita collected and analyzed the data, and drafted and revised the initial manuscript. Dr. Tominaga, Dr. Tanaka, Prof. Ishida, and Prof. Yoshihara interpreted all the data and critically revised the manuscript for important intellectual content. All the authors approved the final manuscript and agreed to be accountable for all aspects of the work.
The authors declare no conflict of interest.