2023 Volume 260 Issue 2 Pages 127-133
2023 Volume 260 Issue 2 Pages 127-133
Acute pulmonary embolism (PE) and coronavirus disease ‐2019 (COVID‐19) are life-threatening diseases associated with significant morbidity and mortality. Yet little is known about their co-existence.This study explored clinical and laboratory differences between PE patients who tested positive with real‐time reverse‐transcription polymerase chain reaction (PCR+) and those who tested negative (PCR−) for SARS-CoV-2. Also, to determine whether ferritin D-dimer ratio (FDR) and platelet D-dimer ratio (PDR) can be used to predict COVID-19 in patients with PE. Files of 556 patients who underwent a computed tomography pulmonary angography (CTPA) examination were retrospectively investigated. Out of them, 197 were tested positive and 188 negative for SARS-CoV-2. One hundred thirteen patients (57.36%) in the PCR+ group and 113 (60.11%) in the PCR− group had a diagnosis of PE. Complaints, respiratory rate, and oxygen saturation level in the blood (SpO2) were recorded at the first admission. Monocyte and eosinophil levels remained low, whereas FDR and PDR were higher in the PCR+ group. No difference was detected in ferritin, D-dimer levels, comorbidities, SpO2, and death rates between the two groups. Cough, fever, joint pain, and higher respiratory rate were more common in the PCR+ group. A decrease in white blood cell, monocyte, and eosinophil levels, whereas an increase in FDR and PDR levels may predict COVID-19 in patients with PE. PE patients complaining of cough, fever, and fatigue should undergo PCR testing as common symptoms. COVID-19 does not seem to increase the risk of mortality in patients with PE.
Acute pulmonary embolism (PE) in patients with coronavirus disease-2019 (COVID-19) is emerging as an essential sequela associated with significant morbidity and mortality (Bikdeli et al. 2020). COVID-19, caused by the severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2), has been a cause of illness and death for millions since its identification in December 2019 presenting with various signs and symptoms (Qin et al. 2021; Baykal et al. 2022). The gold standard diagnostic tool tests nasopharyngeal swab samples by real-time reverse-transcription polymerase chain reaction (PCR). In most cases, computed tomography with pulmonary angiography (CTPA) is the preferred test to confirm or exclude the diagnosis of PE. However, neither CTPA nor PCR is available in every clinic. Simpler and cheaper methods are needed to help diagnose and assist doctors in which patients must undergo CTPA scanning or PCR testing. Biomarkers derived from the peripheral blood, hemogram parameters such as white blood cell (WBC) count, eosinophil levels, monocyte levels, neutrophil-lymphocyte ratio (NLR), and platelet lymphocyte ratio (PLR) have been investigated for the diagnosis, prognosis, and severity of COVID-19 patients (Yang et al. 2020; Seyit et al. 2021). Platelet distribution width (PDW) is a direct measure of platelet size variation and a marker of platelet activation. High levels of PDW have been associated with COVID-19 mortality (Lorente et al. 2021). D-dimer, ferritin, and C-reactive protein (CRP) are important markers and predictors of prognosis in patients with COVID-19 (Alroomi et al. 2021; Poudel et al. 2021). In this study, we hypothesized that these parameters or the ratios of essential parameters in terms of disease severity and prognosis in COVID-19 might help in predicting COVID-19 disease in patients with PE. The present study aimed to explore clinical and laboratory-based differences or similarities between patients with PE tested positively (PCR+) and negatively for SARS-CoV-2 (PCR−). Else to determine whether WBC, monocyte levels, eosinophil levels, PDW, PLR, ferritin D-dimer ratio (FDR), ferritin CRP ratio (FCR), ferritin neutrophil ratio (FNR), platelet neutrophil ratio (PNR), and platelet D-dimer ratio (PDR) can be used as biomarkers in the diagnosis of COVID-19 in patients with PE as well as to explore the most useful diagnostic biomarkers and optimal cut-off values.
After obtaining the ethics committee approval from the Clinical Research Ethics Committee of Bursa City Hospital (Ethics Committee Approval No:2021-3/4), files of those patients admitted to a tertiary city hospital in Turkey between April and September 2020 with complaints compatible with COVID-19 were investigated. The demographic and clinical data of all patients are shown in Table 1. Patients diagnosed with pulmonary embolism were divided into two groups those with positive SARS-CoV-2 PCR results (PCR+) and those with negative SARS-CoV-2 PCR results (PCR−). The PCR− group consists of patients with no pathology other than embolism and patients with additional diseases shown in Table 1. Two patient groups were compared by examining the laboratory parameters obtained on the same admission day before the medical treatment was started in the hospital. Complaints, respiratory rate, and the percent saturation of oxygen in the blood (SpO2) were recorded for each patient at the first admission. CTPA, PCR testing, and consultation with the relevant specialist were performed during their initial access to the COVID-19 emergency department and COVID-19 outpatient clinics.
Combined oropharyngeal and nasopharyngeal samples from patients were obtained by physicians and sent to the laboratory in a virus transport medium (Bio-Speedy vNAT Transfer Tubes) at 4°C to be analyzed by geneticists. After undergoing nucleic acid extraction, samples were tested using the Bio-Speedy severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) kit (Bioeksen, Turkey) in a real-time Rotor-Gene Q PCR device (Qiagen, Düsseldorf, Germany), following the manufacturer’s instructions. The Bio-Speedy SARS-CoV-2 targets the SARS-CoV-2-specific ORF1ab gene and human RNase P gene. According to national guideline (2021): Turkish Thoracic Society Pulmonary Thromboembolism Diagnosis And Treatment Consensus Report, patients who had a Wells score above 6 (high risk) or 2-6 (moderate risk) but had shortness of breath and/or desaturation that could not be explained by chest X-ray along with high D-dimer levels above 0.5 μg FEU/ml at admission underwent a CTPA scan. Partial or complete intraluminal filling defects, which have an interface with intravascular contrast material were considered pulmonary embolism (Fig. 1). Although CTPAs were initially evaluated by different radiologists, the CTPAs included in the present study were re-evaluated by a radiologist with 19 years of experience in radiology. We excluded from the study patients with limited respiratory motion or poor contrast, and patients with insufficient clinical, laboratory and radiological information (Fig. 2). PLR, PNR, and PDR values were calculated by dividing platelet levels by lymphocyte, neutrophil, and D-dimer levels, respectively. FDR, FCR, and FNR values were calculated by dividing ferritin levels by D-dimer, C-reactive protein, and neutrophil levels, respectively.
All the statistical analyses were carried out using IBM SPSS (Statistical Package for the Social Sciences) statistical software program 25.0 software. A Kolmogorov-Smirnov test was performed for the normality of the sample data, and the continuous variables were defined by the mean ± standard deviation, median (interquartile range 25%-75%), while the categorical variables were expressed as frequency and percent. To compare the independent groups, a Student’s t-test for parametric assumptions and a Mann-Whitney U test for non-parametric assumptions were used. The receiver operating characteristic (ROC) curve was performed for optimal cut-off values to predict SARS-CoV-2 positivity. We exploited Youden Index values to identify the optimal cut-off values. Pearson’s correlation coefficient (r) was used to analyze associations between investigated parameters. In addition, a p-value less than 0.05 was set as the statistical significance level.

Demographic and clinical data of SARS-CoV-2 positive and negative patients with acute pulmonary embolism.
COPD, chronic obstructive pulmonary disease; SpO2, the percent saturation of oxygen in the blood.
*p < 0.05, statistically significant.

Filling defects compatible with pulmonary embolism in the left main pulmonary artery (A), right main pulmonary artery (B, D), and in the lobar arteries of the upper lobe and lower lobe of the right lung (C).
Case A and C are negative while case B and D with positive PCR test results for SARS-CoV-2.

Flowchart of patients underwent a computed tomography with pulmonary angiography (CTPA).
PE, acute pulmonary embolism.
Five hundred and fifty-six CTPA performed from April 01, 2020 to September 30, 2020. Forty-three patients were excluded from the study due to limited respiratory motion or poor contrast, and 128 patients were excluded due to insufficient clinical, laboratory and radiological information. Finally 197 patients with COVID-19 (PCR+) and 188 without COVID-19 (PCR−) were studied, and 113 PCR+ and 113 PCR− patients had a diagnosis of PE (Fig. 2). There was no statistical difference between the age of the groups (p = 0.296). Although the sex distribution in the PCR+ group was 45 women (39.8%) and 68 men (60.2%), it was 52 women (46%) and 61 men (52%) in the PCR− patients (Table 1). No difference was detected regarding chronic obstructive pulmonary disease (COPD), bronchial asthma, diabetes mellitus (DM), hypertension (HT), coronary artery disease (CAD), malignancy rates, SpO2 levels at hospital admission, hospital stay, and death rates. PCR+ group had a higher respiratory rate at first hospital admission; more frequent complaints were cough, fatigue, joint pain, and fever (Table 1).
WBC, monocyte, and eosinophil levels were significantly lower in the PCR+ group, whereas FDR, FCR, FNR, PNR, and PDR levels were higher. No difference was detected in platelets, PDW, D-dimer, CRP, ferritin, and PLR values between the two groups (Table 2). To predict COVID-19 disease in patients diagnosed with PE, optimal cut-off values were calculated for FDR, FCR, and FNR (Fig. 3). When PCR+ patients were compared to that PCR−, the areas under the curve (AUC) of FDR, FCR, and FNR were found as 0.75 (p < 0.001), 0.66 (p < 0.001), and 0.66 (p < 0.001), respectively (Table 3). The correlation analysis is shown in Table 4. A negative correlation was detected between WBC and PNR (r = −0.544, p = 0.001), D-dimer and PDR (r = −0.905, p = 0.001) whereas a positive correlation was detected between FDR and FCR (r = 0.554, p = 0.001), and FDR and FNR (r = 0.677, p = 0.001).

Laboratory findings of SARS-CoV-2 positive and negative patients with acute pulmonary embolism.
WBC, white blood cells; PDW, platelet distribution width; FEU, fibrinogen equivalent unit; CRP, C-reactive protein; PLR, platelets lymphocyte ratio; FDR, ferritin D-dimer ratio; FCR, ferritin CRP ratio; FNR, ferritin neutrophil ratio; PNR, platelet neutrophil ratio; PDR, platelet D-dimer ratio.
*p < 0.05, statistically significant.

The receiver operating characteristic (ROC) curve of ferritin D-dimer ratio (FDR), ferritin C-reactive protein ratio (FCR), and ferritin neutrophil ratio (FNR) for prediction of COVID-19 in patients with pulmonary thromboembolism.
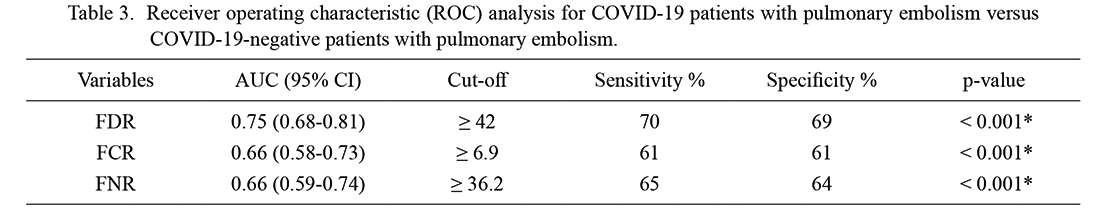
Receiver operating characteristic (ROC) analysis for COVID-19 patients with pulmonary embolism versus COVID-19-negative patients with pulmonary embolism.
AUC, area under ROC curve; CI, confidence interval; FDR, ferritin D-dimer ratio; FCR, ferritin C-reactive protein ratio; FNR, ferritin neutrophil ratio.
*p < 0.05, statistically significant.

Spearman’s correlations between laboratory findings of COVID-19 patients with acute pulmonary embolism.
WBC, white blood cells; EOS, eosinophil; FDR, ferritin D-dimer ratio; FCR, ferritin C-reactive protein ratio; FNR, ferritin neutrophil ratio; PNR, platelet neutrophil ratio; PDR, platelet D-dimer ratio.
*p < 0.05, statistically significant.
Pulmonary thromboembolism is an important and sometimes life-threatening condition. There is limited information available about PE patients infected with SARS-CoV-2. In suspicious cases of COVID-19, PCR is used in the diagnosis and still is the gold standard. Yet PCR is not available in every healthcare institution or is available in limited numbers. Therefore, there is a need for more straightforward and more practical methods to detect COVID-19 cases or increase the suspicion of using limited PCR tests. COVID-19 and PE are diseases in which patients may suffer from shortness of breath. Fever and cough were reported to be more frequent complaints among COVID-19 patients (Qin et al. 2021). Yet symptom frequency in the co-existence of PE and COVID-19 is not well studied, and there is a need for more information in this field. In the present study, in the PCR+ group, cough, fatigue, joint pain, and fever were more common symptoms. The percent oxygen saturation in the blood is undoubtedly a vital parameter that indicates well-being. No difference was detected between SpO2 levels at first admission in the present study, but the respiratory rate was higher in the PCR+ group. Both PE and COVID-19 are sometimes life-threatening conditions; according to recent reports, PE does not increase the mortality rate in COVID-19 patients (Miro et al. 2021; Riyahi et al. 2021). In the present study, we also aimed to explore if COVID-19 increases the mortality risk of patients with PE, but no difference was found.
Evidence suggests an association of WBC with adverse outcomes in patients with cardiovascular diseases via vascular plugging, direct injury to myocytes, and the coronary endothelium (Whiteley et al. 2011). Yet their role is uncertain in PE patients with COVID-19. Previously Venetz et al. (2013) reported that WBC count was an independent predictor of short-term mortality and hospital readmission. In a study, Galland et al. (2021) analyzed 88 patients who tested positive for SARS-CoV-2 and reported WBC ≥ 12.0 G/L independently associated with the PE diagnosis. In the present study, WBC remained lower in the PCR+ group, which might be due to the effects of SARS-CoV-2.
Eosinophils are circulating leukocytes that have the potential for pro-inflammatory effects and have been shown to have various other functions like immunoregulation and anti-viral activity. But their role in COVID-19 is not well known. Xie et al. (2021) reported that COVID-19 patients had low circulating eosinophil counts compared to other types of pneumonia patients. Zhang et al. (2020) have previously reported eosinopenia in patients with acute respiratory deterioration during infection with SARS-CoV-2. The present study has demonstrated that circulating eosinophil counts decrease in the PCR+ group (p = 0.015), which might reflect the inflammation derived from SARS-CoV-2.
Monocytes and macrophages are the most enriched immune cell types in the lungs of COVID-19 patients and appear to have a central role in the pathogenicity of the disease (Bost et al. 2020). Current data suggest a preeminent role for monocyte-macrophage activation in the development of immunopathology of COVID-19 (Gomez-Rial et al. 2020). This study found low monocyte levels in the PCR+ group compared to PCR− (p = 0.013). In a study, Zhang et al. (2021) reported morphological and inflammation-related phenotypic changes in peripheral blood monocytes that correlate with the patient’s outcome during SARS-CoV-2 infection. Zhang et al. (2021) did not detect significant differences in the number of monocytes between patients with COVID-19 and normal healthy individuals. In the light of the obtained results and the studies mentioned above, investigating reasons for monocytopenia may help deal with COVID-19, including those with pulmonary embolism.
COVID-19 causes a spectrum of diseases; some patients develop thrombocytopenia, a severe pro-inflammatory state which can be associated with a unique coagulopathy and procoagulant endothelial phenotype. One of the most challenging situations is when PE accompanies COVID-19. The difficulty is choosing the appropriate anticoagulant while thrombocytopenia is on the other side. Previously, Huang et al. (2015) reported that higher PDW levels were noticed in patients with PE. In this study, no difference was found in PDW and platelet levels between the two groups. The discrepancy between studies might be due to patient characteristics, heterogeneity of COVID-19, and/or inflammation derived by COVID-19 and PE.
In recent years, researchers have been investigating ratios. Some of these are neutrophil/lymphocyte, platelet/lymphocyte, and lymphocyte/monocyte ratio in diagnosing and prognosis of many inflammatory conditions. (Kurtul et al. 2020; Piotrowski et al. 2020) Seyit et al. (2021) reported high NLR and PLR in patients who tested positive for SARS-CoV-2 compared to controls. A study by Yang et al. (2020) from Wuhan, China reported elevated NLR is significantly associated with illness severity. In this study, there was no difference between the PLR of PCR+ and PCR− patients. The difference between the present study and the study conducted by Seyit et al. (2021) might be due to patient characteristics, heterogeneity of COVID-19, or pulmonary thromboembolism itself. Ferritin and CRP are essential biomarkers in patients with COVID-19, and high levels have been associated with poor prognosis (Bost et al. 2020). D-dimer is an essential marker in which high levels raise suspicion for PE. In the present study, we hypothesized that the ratios of biomarkers such as CRP and ferritin, D-dimer, and platelets could be helpful in the diagnosis of patients with COVID-19 and PE. In the present study, FDR, FCR, FNR, PNR, and PDR were higher in the PCR+ group. FDR had an area under the curve (AUC) of 0.75 (p < 0.001) with a cut-off value of 42 for predicting COVID-19 in patients with PE. PDR was strongly negatively correlated with D-dimer levels. Even though no statistically significant difference was detected, D-dimer levels interestingly remained lower in the PCR+ group. Lower levels of D-dimer and negative correlation with PDR might be due to the effects of SARS-CoV-2 or the co-existence of COVID-19 and PE.
This study has some limitations; laboratory parameters used in the study may have been affected by comorbid diseases such as malignancy. Even though all laboratory parameters belong to the time before using an in-hospital treatment, medications used for comorbid conditions such as coronary artery disease, hypertension, and diabetes mellitus may affect blood parameters.
In conclusion, decrease in WBC and eosinophil levels, whereas an increase in FDR and PDR levels may predict COVID-19 in patients with pulmonary embolism. Prospective studies consisting of patients without comorbidities will further clarify the issue. PE patients complaining of cough, fever, joint pain, and fatigue should undergo PCR testing as common symptoms. COVID-19 does not seem to increase the risk of mortality in patients with PE.
The authors declare no conflict of Interest.