2023 Volume 261 Issue 4 Pages 309-315
2023 Volume 261 Issue 4 Pages 309-315
When disasters occur, affected people in evacuation shelters may experience health problems, such as exacerbation of chronic diseases or development of new diseases. This study examined the factors contributing to sudden illness in evacuation shelters used for the 2016 Kumamoto Earthquake. The subjects were evacuees of the Kumamoto Earthquake who were transported to hospitals from evacuation shelters by ambulance. Data on patients transported from evacuation shelters were obtained from emergency transport records at the Kumamoto City Fire Department and from medical institutions. The assessment of the living conditions in the shelter was obtained from the Emergency Medical Information System. A total of 576 patients were transported by ambulance from evacuation shelters in Kumamoto City. Of these, 300 patients for whom detailed information was obtained from medical institutions were included in the analysis. The median age was 71 years, and 213 patients (71%) were over 60 years old. There were 235 patients (78%) with pre-existing medical conditions. The most common reasons for emergency transport were falls and dyspnea, followed by fever, disturbance of consciousness, and abdominal pain. The most common final diagnosis at the medical institutions was trauma due to falls, followed by cardiovascular disease, infectious disease, and cerebral neurological disease. A survey of living conditions in the shelters identified problems with scarcity of space and provision of medical care and food. In order to prevent adverse health outcomes in evacuation shelters, the provision of appropriate living conditions and medical care is important from the acute phase of a disaster.
When disasters occur, affected people in evacuation shelters may experience health problems, such as exacerbation of chronic diseases or development of new diseases. A review of the number of deaths caused by the Hanshin-Awaji Earthquake, the Great East Japan Earthquake, and the 2016 Kumamoto Earthquake, the most recent large-scale earthquakes in Japan, indicates that a large number of indirect deaths occurred in these disasters (Sueta et al. 2019; Naito et al. 2020). It was reported that affected people who escaped dying directly due to major earthquakes but died indirectly did so as a result of worsening health conditions due to the evacuation (Kondo et al. 2019a). The causes of adverse health outcomes in evacuation shelters during disasters may vary depending on the type of disaster.
In Japan, when a sudden illness occurs in an evacuation shelter, the patient is usually transported by ambulance to an emergency hospital. However, there are few studies on patients transported by ambulance from evacuation shelters in Japan. The objective of this study was to examine the factors contributing to sudden illness in evacuation shelters used for the 2016 Kumamoto Earthquake.
The subjects were evacuees of the 2016 Kumamoto Earthquake who were transported to hospitals from evacuation shelters by ambulance. Data from the Kumamoto City Fire Department’s emergency transport records regarding cases transported from evacuation shelters during the period from the occurrence of the 2016 Kumamoto Earthquake to the closure of all evacuation shelters were obtained. Shelters were opened on April 15, 2016, and all shelters were closed on September 15, 2016. The emergency transport record included the date, time, and place of occurrence, age and sex of patient, name of injury or illness, pre-existing illness, severity, and name of the medical institution to which the patient was transported. Based on the emergency transport record, patients transported from facilities designated as evacuation shelters were extracted. In addition, information on final diagnosis and outcome was obtained from the medical institutions to which the patients were transported. A letter of request stating that the research was approved by the Ethical Review Committee of Kumamoto University Hospital was sent to the medical institutions to which the patients were transported. Medical institutions that responded that they would cooperate were sent a survey form. The survey form did not contain any personal information about the patients. Fire department transport record numbers were used to extract patient data at medical institutions. In this study, only patients transported from evacuation shelters in Kumamoto City under the jurisdiction of the Kumamoto City Fire Department were included. Patients from Mashiki Town and Aso City, which are closer to the epicenter, were not included in the study.
Regarding the living conditions in evacuation shelters, the materials of the Kumamoto City Disaster Countermeasures Headquarters Meeting and the evacuation shelter assessment data entered in the Emergency Medical Information System were examined. Factors contributing to health problems in shelters were examined through a comprehensive analysis of patient data and information on the living conditions of the shelters.
Statistical analysis was performed using IBM SPSS Statistics version 28.0 (Chicago, IL, USA). We analyzed the correlation between the number of emergency patients and the number of evacuees in shelters by simple regression analysis. Chi-square test was used to compare proportions between groups. A p < 0.05 was considered statistically significant.
The protocol of this study was approved by the Institutional Review Boards of Kumamoto University Hospitals (Approval No. Rinri 1794).
A total of 576 patients were transported by ambulance from evacuation shelters in Kumamoto City. Fig. 1 shows daily changes in the number of patients transported from evacuation shelters in Kumamoto City. The maximum number of patients in one day was 72, on April 17, 2016. The number of patients during the first 10 days after the earthquake was 309 (54%).
A detailed analysis was conducted on 300 patients for whom detailed information was available from the medical institutions. These 300 patients were transported from 119 shelters to 17 emergency hospitals. Of these, 119 were male and 181 were female. The median age was 71 years, and 213 patients (71%) were over 60 years old (Fig. 2A). Fig. 2B shows the population distribution by sex and age group in Kumamoto City in 2015 Census. Kumamoto City has more older females than males.
In the paramedics’ assessment of severity, 157 patients were mildly ill, 138 were moderately ill, and 5 were severely ill. Moderate and severe cases required inpatient care. Table 1 shows the main reasons for emergency transport from the shelters. Falls and dyspnea were the most common, followed by sudden illnesses, such as fever, disturbance of consciousness, and abdominal pain. Table 2 shows the main pre-existing medical conditions for the patients. Hypertension was the most common, followed by cardiovascular disease, diabetes, and psychiatric disorders. Only 22% of the patients had no pre-existing illness.
Fig. 3 shows the number of evacuation shelters to the number of emergency patients. In 62 of the 119 evacuation shelters, only one patient was transported to an emergency hospital. Table 3 shows the number of patients transported to medical institutions. A total of 261 patients were transported to five major emergency hospitals in Kumamoto City. The other 12 hospitals each received fewer than 10 patients.
After arrival and treatment in the emergency room, 209 patients were discharged, 130 of whom returned to their shelter. Sixteen patients returned to their homes; 63 patients had no known destination. One patient who was transported from the evacuation shelter with cardiopulmonary arrest was pronounced dead in the emergency room, and the final diagnosis was acute myocardial infarction. Two of the 86 patients admitted to the hospital died. The final diagnoses for these patients were colorectal cancer and heart failure, respectively. It was not known whether deaths were related to the disaster.
The most common final diagnosis at the medical institutions was trauma due to falls (Table 4). Head injury was the most common site of trauma (17 of the 42 patients). The most common acute illnesses were cardiovascular disease, infectious diseases, and cerebral neurological disease which include brain and nervous system diseases other than stroke.
Fig. 4 shows the correlation between the number of emergency patients and the number of evacuees in shelters with five or more emergency transports. There was no statistically significant correlation between the number of emergency patients and the number of evacuees for each shelter.
Fig. 5 shows the living conditions of 14 evacuation shelters where the number of emergency patients was five or more. Electricity, air-conditioning, toilet, and drinking water were adequate in more than half of the shelters. On the other hand, space density, medical care provision, and providing meals were inadequate in more than half of the shelters.

Daily changes in the number of patients transported by ambulance from evacuation shelters in Kumamoto City.
On the horizontal axis of the graph, 4/14 means April 14, 2016.

Number of patients transported by age and sex (A), and population distribution by sex and age group in Kumamoto City in 2015 Census (B).

Main reasons for emergency transport from the shelters.

Pre-existing medical conditions of the transported patients.

Number of shelters by number of emergency patients.
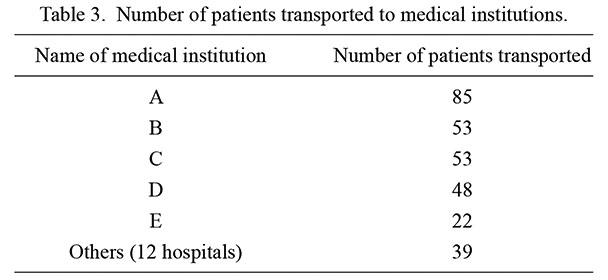
Number of patients transported to medical institutions.

Final diagnosis at medical institutions.

Correlation between the number of emergency patients and evacuees for each shelter.

Living conditions in evacuation shelters.
These data are of 14 shelters with five or more emergency transportations.
Health problems may occur in evacuation shelters and lead to related deaths, however, there are still insufficient studies that investigate the actual situation in detail. In addition, different disasters may have different factors causing health problems. We believe that this study is significant because there have been no sufficient studies on health problems in evacuation shelters in the Kumamoto Earthquake. This study examined the contributing factors to the health problems of patients transported by ambulance from evacuation shelters following the Kumamoto Earthquake. These patients showed the following characteristics: 1) more than half of the patients were transported during the first 10 days after the earthquake; 2) many patients were elderly and had pre-existing medical conditions; 3) many head injuries due to falls were observed; 4) fatal diseases, including as acute myocardial infarction and stroke, were also observed; and 5) inadequate medical care and food provision in shelters.
A magnitude 6.5 earthquake struck the Kumamoto region of Kumamoto Prefecture at 9:26 p.m. on April 14, 2016, followed by a magnitude 7.3 earthquake at 1:25 a.m. on April 16 also in the region of Kumamoto Prefecture. The occurrence of two major earthquakes in a short period of time, along with their numerous aftershocks, had a negative impact on the physical and mental health of those in this area. Table 5 shows the number of direct and indirect deaths in the Great East Japan Earthquake, the Hanshin-Awaji Earthquake, and the Kumamoto Earthquake based on reports from the national and local governments. The percentage of indirect deaths is significantly higher in the Kumamoto Earthquake than in the other two earthquakes (p < 0.001), suggesting the importance of preventing health problems during evacuation.
In this study, emergency patients from evacuation shelters were more common in the acute phase following the earthquake, suggesting that stress from the earthquake and problems with the living condition in the evacuation shelters may have contributed to the deterioration of the patients’ health conditions. Prevention of falls in evacuation shelters and the continuation of medication for chronic illnesses are important to prevent health problems. It is also important to establish a system for detecting fatal diseases, such as myocardial infarction and stroke at an early stage, and connect them to medical treatment. Two of the three fatal cases were due to aggravation of a chronic illness at the evacuation shelter, which resulted in emergency hospitalization, but they died without effect of treatment. The other was a sudden death due to acute myocardial infarction. Although the stress of the evacuation is thought to have affected all of these cases, it is unlikely that the death could have been prevented.
Kondo et al. (2019a) reported that prolonged stays at the evacuation shelter produce several public health problems, such as increased numbers of deep vein thrombosis patients, increased risk for infectious disease, and increased incidence of heat-related illness. A rapid response by a specialized medical relief team was considered important. Tsuboi et al. (2022) reported that during the Great East Japan Earthquake, the risk of disaster-related death was significantly higher for those requiring nursing care than for those who were living independently, indicating the need for measures to be taken for the elderly and those requiring nursing care soon after the disaster. Tokumaru et al. (2022) conducted a study of medical problems in evacuation shelters following a major earthquake in Japan and reported that inadequate living conditions in evacuation shelters led to worsening nutritional status and exacerbation of chronic disease. These reports suggest the importance of providing medical care in the early stages of a disaster.
Epidemiological surveys of diseases following the 2016 Kumamoto Earthquake indicated an increased incidence of heart failure and deep vein thrombosis, as well as poor blood glucose control in diabetic patients (Sueta et al. 2017; Matsukawa et al. 2018; Hokimoto 2018; Sato et al. 2019; Kondo et al. 2019b; Nagayoshi et al. 2021; Onishi et al. 2022). It is important to continue medical care for patients with chronic diseases, as well as providing a supportive their living environment. Furthermore, the importance of dental care, including oral care, in preventing aspiration pneumonia after a disaster has been reported (Kato et al. 2019; Yamazoe and Naito 2022).
A study of trends among evacuees who visited clinics in evacuation shelters after the 2016 Kumamoto Earthquake reported that most experienced mild injuries and common diseases (Yorifuji et al. 2018). Because our study included patients transported by ambulance from shelters, some patients had fatal illnesses. In our study, the absolute number of evacuees and length of stay in shelters were not directly related to the occurrence of emergency patients. The shelter environment may have improved over time after the disaster, but further research is needed.
This study had several limitations. First, patients for whom detailed information was not available from the hospitals were excluded from the analysis. Second, the date of the survey of living conditions in the shelters were not always the same as at the time the patient was transported by ambulance. Third, information on the living conditions in some evacuation shelters was not accessible. Fourth, patients who visited a shelter first-aid station or a hospital on their own for a sudden illness were not included. However, it is highly significant to conduct a survey of patients transported to emergency rooms with serious illnesses in order to prevent disaster-related deaths in evacuation shelters.
In conclusion, many of the patients who were transported to emergency rooms from evacuation shelters in the 2016 Kumamoto Earthquake were elderly and had pre-existing medical conditions, many of which occurred in the acute phase after the earthquake. Furthermore, the living conditions and medical care provided in the evacuation shelters were inadequate. In order to prevent adverse health outcomes in evacuation shelters, the provision of appropriate living conditions and medical care is important from the acute phase of a disaster.

Comparison of direct and indirect fatalities in the Great East Japan Earthquake, the Hanshin-Awaji Earthquake, and the Kumamoto Earthquake.
We hereby express our deep gratitude to the Kumamoto City Fire Department for providing the emergency transport record data and to the hospitals for providing the patient information. This study was funded by the Japanese Ministry of Health, Labour and Welfare (Grant no. 19K10535).
The authors declare no conflict of interest.