2024 年 262 巻 2 号 p. 115-124
2024 年 262 巻 2 号 p. 115-124
Bivalirudin as an anticoagulant reduces bleeding after percutaneous coronary intervention (PCI), while its impact in elderly Chinese patients treated with PCI needs more evidence. This study aimed to compare the clinical outcomes between bivalirudin and heparin in elderly Chinese patients treated with PCI. This cohort study retrieved data of 1,286 elderly patients treated with PCI who used bivalirudin (bivalirudin group, N = 493) or heparin (heparin group, N = 793) as anticoagulants. Net adverse clinical events (NACEs) (primary endpoint), major adverse cardiac and cerebral events (MACCEs), bleeding, and major bleeding within 30 days after PCI treatment were recorded for analysis. Our study illustrated that NACEs (12.4% vs. 17.4%, P = 0.015), bleeding (6.7% vs. 12.1%, P = 0.002), and major bleeding (2.2% vs. 6.6%, P < 0.001) were fewer in bivalirudin group compared to heparin group. No difference was found in MACCEs (7.5% vs. 9.6%,P = 0.200), and incidences of all-cause mortality (P = 0.257), cardiac mortality (P = 0.504), recurrent myocardial infarction (P = 0.423), ischemia-driven revascularization (P = 0.509), and stroke (P = 0.467), between bivalirudin group and heparin group. According to univariate logistic regression analyses, bivalirudin (vs. heparin) correlated with fewer NACEs (P = 0.016), bleeding (P = 0.002), and major bleeding (P = 0.001) in elderly patients treated with PCI, but not MACCEs (P = 0.202). After adjustment, bivalirudin (vs. heparin) was an independent factor for fewer NACEs [odds ratio (OR): 0.619, P = 0.009], bleeding (OR: 0.499, P = 0.003), and major bleeding (OR: 0.342, P = 0.003) in these patients. In summary, bivalirudin achieves fewer NACEs, bleeding, and major bleeding, but not MACCEs, versus heparin in elderly patients treated with PCI, which is verified in the multivariate model.
Percutaneous coronary intervention (PCI) is a crucial treatment for revascularization in cardiovascular diseases, such as acute coronary syndromes (ACS), ST segment elevation myocardial infarction (STEMI), acute myocardial infarction (AMI), etc. (Lawton et al. 2022). PCI unblocks stenotic or even occluded coronary arteries to improve myocardial perfusion, alleviate angina, and reduce acute death in these patients (Siontis et al. 2016; Al-Lamee et al. 2019; Otaki et al. 2020; Akbari and Al-Lamee 2022). Nevertheless, elderly patients (age ≥ 65 years) may experience more extensive acute coronary disease, heightened ischemic burden, increased cardiovascular event risks, frailty, and enhanced prevalence of other chronic diseases, and therefore, they may have elevated surgical difficulties during PCI and increased adverse events after PCI (Guo et al. 2020). In-stent restenosis (ISR) is a major adverse outcome caused by post-PCI thrombotic events; and elderly patients, especially those with metabolic disease, frequently receive repeat PCI and commonly have poor prognosis possibly due to ISR (Moussa et al. 2020; Kawai et al. 2022; Duband et al. 2023). Anticoagulants, including thrombin inhibitors, vitamin K antagonists, novel oral anticoagulants, and antiplatelet drugs, are thus recommended for thrombosis prevention and ISR reduction following PCI (Robertson et al. 2012). However, using anticoagulants possibly increases the risk of bleeding, which is associated with post-PCI mortality in elderly patients (Rao et al. 2012; Nair et al. 2022). Thus, it is critical to find anticoagulants that strike a balance between treatment efficacy and bleeding risk in elderly patients treated with PCI (Bhatty et al. 2014). Heparin is one of the most popular anticoagulants to reduce the risk of thrombosis in surgical settings (Lee and Kong 2015). It complexes with antithrombin Ⅲ to inhibit thrombin and suppress coagulation factor Xa, resulting in a potent anticoagulant effect (Lee and Kong 2015; Beurskens et al. 2020). Due to the good efficacy in reducing the risk of thrombotic complications, heparin has been recommended for PCI, usually in combination with glycoprotein IIb/IIIa inhibitors (GPIs) in elderly patients (Lawton et al. 2022). In contrast, heparin has some shortcomings, including the nonlinear pharmacokinetic characteristics, and inducing bleeding-associated thrombocytopenia and other adverse events (Lee and Kong 2015; Pishko et al. 2019; Beurskens et al. 2020).
Bivalirudin is a direct thrombin inhibitor (DTI) with a relatively wider therapeutic index property than heparin and reversible binding to thrombin, which is approved as an anticoagulant for PCI (James et al. 2021; Zhang et al. 2021; Capodanno et al. 2022; Lawton et al. 2022; Montinari and Minelli 2022). For instance, one study indicates that bivalirudin reduces stent thrombosis in STEMI patients with PCI compared to heparin (James et al. 2021). Another study elucidates that bivalirudin exhibits comparative efficacy compared to unfractionated heparin (UFH) in chronic total occlusion (CTO) patients undergoing PCI (Zhang et al. 2021). Notably, bivalirudin also reduces incidence of bleeding in patients with PCI according to many studies (Stone et al. 2008; Koeth et al. 2013; Fach et al. 2017; Gargiulo et al. 2018). For example, a cohort study shows that using bivalirudin is associated with less bleedings compared to heparin in STEMI patients with PCI (Fach et al. 2017). According to a randomized controlled study, bivalirudin decreases 30-day rate of major bleeding compared with heparin plus GPIs in STEMI patients with primary PCI (Stone et al. 2008). Another clinical study indicates that bivalirudin realized fewer bleeding complications in elderly patients undergoing PCI versus (vs.) heparin (Koeth et al. 2013). Nonetheless, few study has investigated the role of bivalirudin in elderly Chinese patients treated with PCI.
This study aimed to comprehensively compare the impact between bivalirudin and heparin on net adverse clinical events (NACEs), major adverse cardiac and cerebral events (MACCEs), and bleeding events in elderly Chinese patients treated with PCI.
This cohort study retrospectively retrieved 1,286 elderly patients treated with PCI using bivalirudin or heparin [low molecular weight heparin (LMWH) or UFH] as anticoagulants at our hospital from April 2019 to March 2023. The screening criteria were: i) aged more than 65 years old (Li et al. 2016); ii) underwent primary PCI using bivalirudin or heparin (LMWH or UFH) as anticoagulants; iii) had complete clinical data for study analysis. The exclusion criteria were: i) had cancers or hematological malignant diseases; ii) had histories of bleeding diathesis, coagulopathy, or heparin-induced thrombocytopenia; iii) had histories of intracerebral mass, aneurysm, arteriovenous malformation, or hemorrhagic stroke. The Ethics Committee of The Affiliated Hospital, Southwest Medical University gave their approval to this study. Patients or their families provided informed consent.
Data collectionAge, sex, body mass index (BMI), hypertension, diabetes mellitus, cardiac surgery, clinical manifestation, Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcomes with Early implementation of the ACC/AHA guidelines (CRUSADE) score, operative timing, and lesion vessel were obtained from the Electronic Medical Record. Besides, PCI-related information was collected, including PCI type, stent diameter, and stent length (total). Additionally, bivalirudin or heparin (LMWH or UFH) were used as anticoagulants. The dosage of bivalirudin was 0.75 mg/kg of body weight as first dose, followed by 1.75 mg/kg per hour for at least 4 hours after PCI. The dosage of LMWH was 0.5 mg/kg. The dosage of UFH was 70-100 IU/kg without a GPI or 50-70 IU/kg with a GPI. The anticoagulant and glycoprotein inhibitor choice were non-intervene, which was according to the patient’s disease condition. The detailed regimens of bivalirudin and heparin (LMWH or UFH) were the same as in previous studies (Steg et al. 2013; Ali-Hassan-Sayegh et al. 2016).
GroupsPatients who were administrated with bivalirudin were defined as the bivalirudin group (N = 493), while patients who were administrated with heparin were defined as the heparin group (N = 793). In 793 patients who received heparin, there were 544 (68.6%) patients administrated with LMWH and 249 (31.4%) patients administrated with UFH.
Evaluations and definitionsNACEs, MACCEs, bleeding, and major bleeding within 30 days after PCI treatment were recorded for analysis. The bleeding was defined as the Bleeding Academic Research Consortium (BARC) types 2-5, and the major bleeding was defined as BARC types 3-5 (Choi et al. 2022). The MACCEs involved all-cause mortality, cardiac mortality, recurrent myocardial infarction (MI), ischemia-driven target vessel revascularization, and stroke (Navarese et al. 2014). The NACEs contained bleeding and MACCEs.
Statistical analysesSPSS v.26.0 (IBM, Armonk, NY, USA) was used for data analysis. The student t-test, Mann-Whitney U test, or χ2 test was used for comparison analysis as appropriate. The univariate and multivariate logistic regression analyses were used for screening factors related to risks of NACEs, MACCEs, bleeding, or major bleeding. The forward-step method was used in the multivariate analysis. P < 0.05 indicated significance.
The mean age of heparin group and bivalirudin group was 73.6 ± 6.1 years and 73.4 ± 5.9 years (mean ± SD), correspondingly. There were 317 (40.0%) females in heparin group and 180 (36.5%) females in bivalirudin group. All clinical characteristics [including age, sex, BMI, hypertension, diabetes mellitus, cardiac surgery, clinical manifestation, CRUSADE score, CRUSADE high risk, operative timing, lesion vessel, PCI type, stent diameter, and stent length (total)] were of no difference between heparin group and bivalirudin group (all P > 0.050) (Table 1).

Clinical characteristics of patients with percutaneous coronary intervention (PCI).
SD, standard deviation; BMI, body mass index; UA, unstable angina; NSTEMI, non-ST-elevation myocardial infarction; SCAD, spontaneous coronary artery dissection; STEMI, ST-elevation myocardial infarction; IQR, interquartile range; CRUSADE, Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcomes with Early implementation of the ACC/AHA guidelines; PCI, percutaneous coronary intervention.
Incidence of NACEs was decreased in bivalirudin group compared to heparin group (12.4% vs. 17.4%, P = 0.015) (Fig. 1A). No difference was seen in MACCE incidence between bivalirudin group and heparin group (7.5% vs. 9.6%, P = 0.200) (Fig. 1B). Bleeding incidence was reduced in bivalirudin group than that in heparin group (6.7% vs. 12.1%, P = 0.002) (Fig. 1C). Meanwhile, incidence of major bleeding was descended in bivalirudin group compared to heparin group (2.2% vs. 6.6%, P < 0.001) (Fig. 1D).

Incidences of net adverse clinical events (NACEs), bleeding, and major bleeding were declined in heparin group vs. bivalirudin group.
Comparison of NACEs (A), major adverse cardiac and cerebral events (MACCEs) (B), bleeding (C), and major bleeding (D) incidences between bivalirudin and heparin in elderly patients treated with percutaneous coronary intervention (PCI).
No difference was found in all-cause mortality (5.9% vs. 4.5%, P = 0.257), cardiac mortality (4.4% vs. 3.7%, P = 0.504), recurrent MI (2.3% vs. 1.6%, P = 0.423), ischemia-driven revascularization (1.9% vs. 2.4%, P = 0.509), or stroke (2.0% vs. 2.6%, P = 0.467) between bivalirudin group and heparin group. The detailed information was listed in Fig. 2.
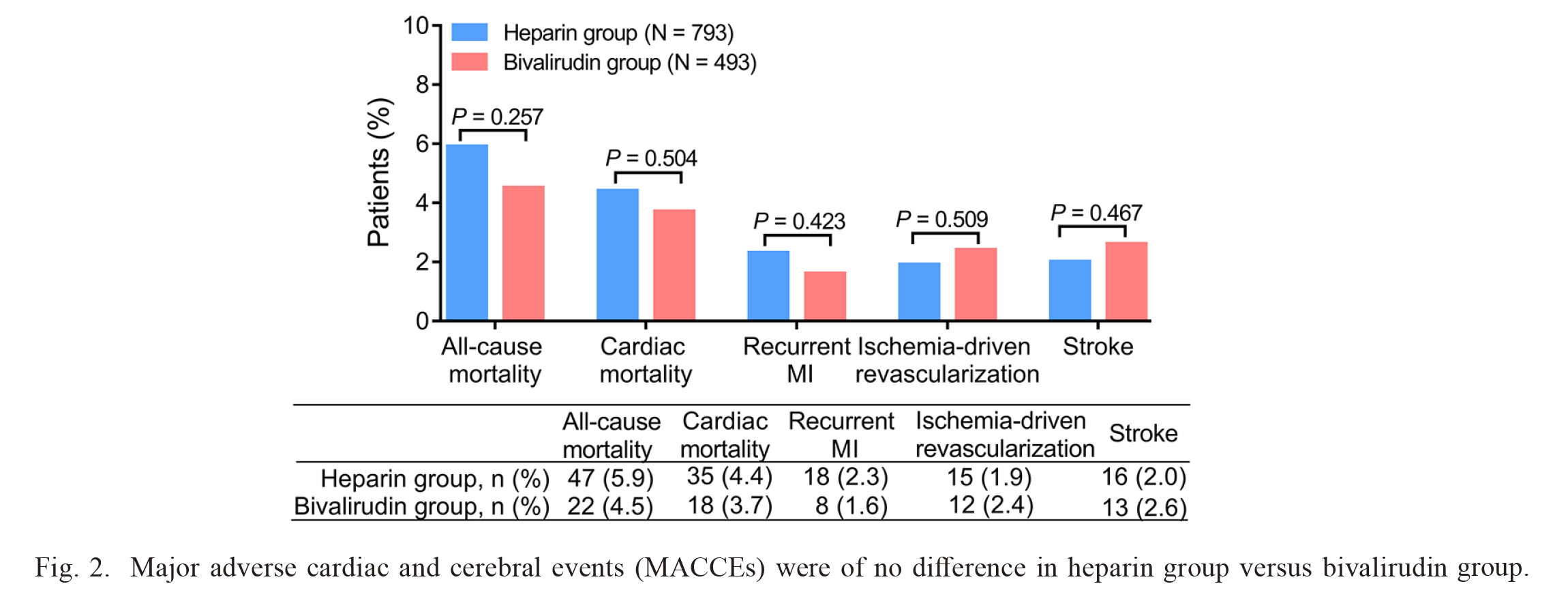
Major adverse cardiac and cerebral events (MACCEs) were of no difference in heparin group versus bivalirudin group.
Comparison of MACCEs between bivalirudin and heparin in elderly patients treated with percutaneous coronary intervention (PCI). MI, myocardial infarction.
Bivalirudin (vs. heparin) (P = 0.016) was correlated with fewer NACEs, while age ≥ 75 years (P < 0.001), female (vs. male) (P = 0.026), SCAD (vs. UA) (P < 0.001), NSTEMI (vs. UA) (P = 0.008), STEMI (vs. UA) (P = 0.003), CRUSADE high risk (P = 0.030), emergency operation (vs. elective operation) (P < 0.001), and multiple vessel lesion (vs. single vessel lesion) (P = 0.047) were related to higher NACE incidence (Fig. 3A). Further multivariate logistic regression analysis indicated that bivalirudin (vs. heparin) [odds ratio (OR): 0.619, P = 0.009] was an independent factor for fewer NACEs, whereas age ≥ 75 years (OR: 1.851, P < 0.001), female (vs. male) (OR: 1.419, P = 0.040), emergency operation (vs. elective operation) (OR: 2.459, P < 0.001), and multiple vessel lesion (vs. single vessel lesion) (OR: 1.702, P = 0.008) were independent factors for higher NACE incidence (Fig. 3B).

Bivalirudin was independently correlated with fewer net adverse clinical events (NACEs).
Univariate (A) and multivariate (B) logistic regression analysis for NACEs in elderly patients treated with percutaneous coronary intervention (PCI).
Bivalirudin (vs. heparin) was not associated with MACCEs (P = 0.202). While age ≥ 75 years (P = 0.025), female (vs. male) (P = 0.023), diabetes mellitus (P = 0.050), SCAD (vs. UA) (P = 0.012), and multiple vessel lesion (vs. single vessel lesion) (P = 0.005) were correlated with higher MACCE incidence (Fig. 4A). After the adjustment of multivariate logistic regression analysis, it was noticed that age ≥ 75 years (OR: 1.601, P = 0.024) and multiple vessel lesion (vs. single vessel lesion) (OR: 1.747, P = 0.013) were independent factors for higher MACCE incidence (Fig. 4B).

Bivalirudin was not associated with fewer major adverse cardiac and cerebral events (MACCEs).
Univariate (A) and multivariate (B) logistic regression analysis for MACCEs in elderly patients treated with percutaneous coronary intervention (PCI).
Bivalirudin (vs. heparin) (P = 0.002) was correlated with fewer incidence of bleeding, while age ≥ 75 years (P < 0.001), SCAD (vs. UA) (P = 0.002), NSTEMI (vs. UA) (P = 0.001), STEMI (vs. UA) (P = 0.001), CRUSADE high risk (P < 0.001), and emergency operation (vs. elective operation) (P < 0.001) were related to higher incidence of bleeding (Fig. 5A). Forward step multivariate logistic regression analysis indicated that bivalirudin (vs. heparin) (OR: 0.499, P = 0.003) was an independent factor for fewer incidence of bleeding. Contrarily, age ≥ 75 years (OR: 1.969, P = 0.001), CRUSADE high risk (OR: 1.621, P = 0.025), and emergency operation (vs. elective operation) (OR: 3.086, P < 0.001) were independent factors for higher incidence of bleeding (Fig. 5B).

Bivalirudin was independently correlated with fewer bleeding.
Univariate (A) and multivariate (B) logistic regression analysis for bleeding in elderly patients treated with percutaneous coronary intervention (PCI).
Bivalirudin (vs. heparin) (P = 0.001) was correlated with fewer incidence of major bleeding, while age ≥ 75 years (P < 0.001), diabetes mellitus (P = 0.038), NSTEMI (vs. UA) (P = 0.034), STEMI (vs. UA) (P = 0.017), CRUSADE high risk (P < 0.001), and emergency operation (vs. elective operation) (P = 0.001) were related to higher incidence of major bleeding (Fig. 6A). Moreover, bivalirudin (vs. heparin) (OR: 0.342, P = 0.003) was an independent factor for fewer major bleeding incidence, whereas age ≥ 75 year (OR: 2.392, P = 0.003), CRUSADE high risk (OR: 2.142, P = 0.008), and emergency operation (vs. elective operation) (OR: 2.605, P = 0.001) were independent factors for higher incidence of major bleeding (Fig. 6B).

Bivalirudin was independently correlated with fewer major bleeding.
Univariate (A) and multivariate (B) logistic regression analysis for major bleeding in elderly patients treated with percutaneous coronary intervention (PCI).
This study discovered that: (1) Bivalirudin realized fewer NACEs, bleeding, and major bleeding compared to heparin in elderly patients treated with PCI. (2) No difference was seen in MACCEs between bivalirudin and heparin in elderly patients treated with PCI. (3) Bivalirudin was independently correlated with fewer incidences of NACEs, bleeding, and major bleeding in elderly patients treated with PCI.
Bivalirudin is an effective anticoagulant inhibiting thrombin either free or bound to fibrin, while lowering bleeding rates compared to heparin (Ng et al. 2016; Gargiulo et al. 2018; Patel et al. 2019; Meng et al. 2020; Li et al. 2022; Montinari and Minelli 2022). For example, one study demonstrates that bivalirudin significantly reduces bleeding complications than UFH in ACS patients receiving PCI (10.8% vs. 12.2%) (Gargiulo et al. 2018). Another meta-analysis for AMI patients with PCI shows that bivalirudin decreases major bleeding compared to heparin (2.3% vs. 3.5%) (Patel et al. 2019). Concerning heightened surgical complexities during PCI attributed to age-related anatomical and physiological changes, it is imperative to pay more attention to the utilization of drugs for reducing risks of adverse events in elderly patients (Guo et al. 2020). A previous study indicates that bivalirudin realizes declined bleeding vs. heparin in elderly patients with PCI (10.0% vs. 12.9%) (Li et al. 2022). Similarly, this study discovered that bivalirudin realized fewer bleeding (6.7% vs. 12.1%) and major bleeding (2.2% vs. 6.6%) compared to heparin in elderly patients treated with PCI. The possible explanations could be: (1) Due to the unique pharmacologic profile (a fast onset of action, 25-minute half-life, not binding to plasma proteins, linear pharmacokinetic and pharmacodynamic features), bivalirudin could prevent excessive anticoagulant effect (Lee and Ansell 2011; Meng et al. 2020; Montinari and Minelli 2022). (2) Unlike heparin acting on coagulation factors to inhibit thrombin, bivalirudin directly inhibited thrombin, reducing the interference of anticoagulant (Lee and Kong 2015; Beurskens et al. 2020; Capodanno et al. 2022; Montinari and Minelli 2022). (3) With low immunogenic potential, bivalirudin avoided immune-mediated thrombocytopenia, which further prevented bleeding (Lee and Ansell 2011; Montinari and Minelli 2022). Thereby, bivalirudin was correlated with fewer bleeding and major bleeding compared to heparin in elderly patients treated with PCI.
MACCE is a critical endpoint in patients treated with PCI (Gabriel et al. 2021). In this study, MACCEs were of no difference between bivalirudin and heparin in elderly patients treated with PCI. The possible explanation could be that the occurrence of MACCEs mainly depended on disease burden and surgical implementation (Tsai et al. 2017; Zhao et al. 2020; Gabriel et al. 2021; Fadah et al. 2022), rather than the use of bivalirudin or heparin. Thus, the similarity of aforementioned features resulted in similar incidence of MACCEs between the two drugs in elderly patients treated with PCI.
Bivalirudin results in fewer NACEs compared to heparin in patients treated with PCI, which is supported by several studies (Stone et al. 2008; Han et al. 2015; Meng et al. 2020). According to a randomized controlled study, bivalirudin realizes lower 30-day rate of NACEs is in STEMI patients with primary PCI than heparin plus GPIs (9.2% vs. 12.1%) (Stone et al. 2008). Another study indicates that the use of bivalirudin realizes a decrement in NACEs compared to heparin in AMI patients undergoing primary PCI (8.8% vs. 13.2%) (Han et al. 2015). This study displayed that bivalirudin realized fewer NACEs compared to heparin in elderly patients treated with PCI (12.4% vs. 17.4%). The incidence of NACEs was elevated in this study than previous studies (Stone et al. 2008; Han et al. 2015), which could be explained by the fact that patients in this study (73.4 ± 5.9 years) were older than previous studies (57.3 ± 11.6 years) and were more likely to experience NACEs due to extensive coronary artery disease and severe ischemic burden (Guo et al. 2020). As NACEs included MACCEs and bleeding, and MACCEs was of no difference between bivalirudin group and heparin group, the reduction of NACEs was mainly driven by reduction of bleeding due to bivalirudin vs. heparin in elderly patients treated with PCI.
Moreover, this study used forward step logistic regression analysis to adjust the incidences of NACEs, MACCEs, bleeding, and major bleeding in elderly patients treated with PCI and discovered that bivalirudin was independently correlated with fewer incidences of NACEs, bleeding, and major bleeding in these patients. These findings provided clinical evidence for the perioperative application of bivalirudin during in elderly patients treated with PCI who were at a high risk of poor prognosis. Meanwhile, these findings were also in accordance to previous studies (Koeth et al. 2013; Liang et al. 2016; Ng et al. 2016). Taking a randomized controlled study as an example, it reveals that bivalirudin is an independent protective factor for 30-day NACEs in AMI patients with emergency PCI (Liang et al. 2016). A multivariate regression analysis from one study elucidates that bivalirudin is one of independent predictors of fewer bleeding events in elderly patients with PCI (Koeth et al. 2013). In addition, age ≥ 75 years was also independently correlated with more incidences of NACEs, MACCEs, bleeding, and major bleeding. The probable reason could be that patients whose age ≥75 years were more likely to have coronary calcification and multiple vessel lesions, resulting in higher risks of adverse events (Vandermolen et al. 2015).
There were some limitations in this study. To begin with, this study was a single-center study, which might result in selective bias. Secondly, this retrospective study was not under the randomized, controlled settings (including uncontrolled dosage and duration of medications), thus, the confounding factors existed and internal validity was not ensured. Finally, the 30-day follow-up of this study was relatively short.
In summary, bivalirudin displays attenuated NACEs, bleeding, and major bleeding, but not MACCEs compared to heparin in elderly patients treated with PCI, providing certain evidence-based basis for the use of bivalirudin in elderly Chinese patients.
The authors declare no conflict of interest.