2024 年 263 巻 1 号 p. 27-34
2024 年 263 巻 1 号 p. 27-34
This study aimed to investigate the effects of a Roy adaptation model (RAM)-based cognitive stimulation therapy (CST) intervention on elderly patients diagnosed with primary non-small cell lung cancer (NSCLC) undergoing curative resection. A total of 280 patients diagnosed with primary NSCLC were randomized into RAM-based CST group and control group. Outcomes were assessed at three intervals: pre-surgery, discharge, and one-month post-discharge. Cognitive function was evaluated using Mini-Cognitive test. Postoperative delirium prevalence was determined within 48 hours post-surgery using Nursing Delirium Screening Scale. The Hospital Anxiety and Depression Scale evaluated anxiety and depression symptoms, while Quality of Life (QoL) was assessed via Short Form-36 (SF36) Health Survey. The RAM-based CST group demonstrated significantly higher Mini-Cog test scores than the control group upon discharge and post-intervention. Patients with RAM-based CST exhibited a decrease in postoperative delirium compared to the control group. The RAM-based CST intervention yielded an improvement in anxiety and depression at discharge and 1-month post-discharge compared to preoperative levels. Additionally, the RAM-based CST group exhibited substantial enhancements in SF36 subcategory scores at 1-month post-discharge compared to pre-surgery. At post-intervention, the RAM-based CST group demonstrated significantly higher scores than the control group across various health-related domains, including role limitations due to emotional problems, mental health, general health perception, bodily pain, and role limitations due to physical problems. The RAM-based CST intervention in elderly NSCLC patients undergoing curative resection yielded significant enhancements in cognitive function, reduced delirium incidence, improved emotional well-being, and better QoL postoperatively.
Lung cancer constitutes a significant global health challenge, accounting for 13% (1.6 million) of new cancer cases worldwide among the 12.7 million total cases and ranking as the most frequently diagnosed cancer in men. Alarmingly, it stands as the primary cause of cancer-related mortality, claiming 1.4 million lives, which represents 18% of cancer deaths globally (Polanski et al. 2022). It is broadly categorized into non-small cell lung cancer (NSCLC), making up 80% of cases, and small cell lung cancer (SCLC), comprising the remaining 20% (Jankowska-Polanska et al. 2020). Projections suggest that by 2030, the majority of newly diagnosed cancer cases will be within the elderly demographic (Kamel and Port 2018). The median age at which lung cancer is diagnosed is 70 years, with an estimated 70% of future cases anticipated to manifest in individuals aged over 65 years (Im et al. 2019). Effective interventions for individuals with NSCLC necessitate a comprehensive approach, ensuring not only medical care but also emotional and instrumental support from healthcare providers, peers, family, and friends, particularly within the initial phase following surgery (Banik et al. 2017). In light of these critical considerations, interventions targeting cognitive stimulation and emotional well-being have garnered recognition for their potential to enhance postoperative outcomes.
The Roy adaptation model (RAM) evaluates adaptation across physical (physiological) and psychosocial (self-concept, role function, and interdependence) modes (Banik et al. 2017; Dagcan et al. 2023). In the context of this study, physiological measurements pertain to bodily functions, activity levels, and functionality. Self-concept refers to an individual’s beliefs, including spiritual and self-assessment components, operationalized as exercise confidence or self-efficacy. Role function measures an individual’s expectations regarding functioning and relationships, while interdependence evaluates the exchange of love within nurturing relationships (Yeh 2003; DeSanto-Madeya 2006). RAM has demonstrated successful application in various medical contexts, such as female breast cancer patients (Erol Ursavas and Karayurt 2021), pediatric cancer cases (Yeh 2001), and bone metastasis (Maxwell et al. 2001). Its structured approach has facilitated pain assessment in older adults (Flanagan 2018) and promoted physical activity among sedentary elderly populations (Rogers and Keller 2009).
Postoperative cognitive impairment, delirium, and psychological distress significantly impact the recovery trajectory and Quality of Life (QoL) in lung cancer patients undergoing surgical resection (Root et al. 2013; Shiono et al. 2013). Several studies have indicated the positive effects of cognitive stimulation therapy (CST) on global cognitive function (Binns et al. 2020; Alvares-Pereira et al. 2021, 2022). Home-based CST has also shown beneficial effects in the oncology population (Tapia et al. 2023). Within the context of CST, RAM offers theoretical foundations guiding interventions focused on enhancing cognitive abilities. In RAM’s physiological mode, CST interventions such as respiratory training and physical exercises aim to stimulate the brain and enhance cognitive function. Correspondingly, RAM’s self-concept mode aligns with CST activities targeting memory improvement and problem-solving. The simulated daily activities in CST, akin to RAM’s role function mode, effectively engage cognitive skills. Furthermore, RAM’s interdependence mode, emphasizing nurturing relationships, parallels CST’s family-based rehabilitation plans, nurturing cognitive improvement within the home environment. The RAM-based CST improved cognition in Alzheimer’s disease patients, resulting in reduced disease-related expenses and indirectly contributing to the national economy (Lok et al. 2020).
The study hypothesizes that RAM-based CST intervention would exert a positive impact by enhancing cognitive function, mitigating postoperative delirium, alleviating symptoms of anxiety and depression, and notably improving the overall QoL among elderly NSCLC patients undergoing curative resection. These anticipated outcomes aim to illuminate the potential advantages offered by RAM-based CST intervention, thereby offering invaluable insights to refine postoperative care strategies tailored for this specific patient population.
In line with the Helsinki Declaration’s principles, this study received approval from the ethics committee of our hospital and obtained informed consent from all participating patients.
Enrolled subjectsThe study enrolled patients diagnosed with primary NSCLC between May 2021 and May 2023, with histological confirmation of NSCLC either preoperatively or intraoperatively. Inclusion criteria encompassed patients without prior malignancies, possessing communication and social engagement capabilities, having a life expectancy of at least six months, and expected to return home after surgery. Exclusion criteria included patients with the central nervous system (CNS) cancer or cerebral metastases, preoperative diagnosis of dementia, or an American Society of Anesthesiologists (ASA) score > 3. A total of 280 patients were enrolled and underwent envelope randomization, which assigned them to either the RAM-based CST group (RAM-based CST intervention in addition to standard care) or the control group (standard care), with 140 patients allocated to each group. All participants underwent major pulmonary resections, specifically lobectomy or pneumonectomy, aimed at curative treatment.
InterventionIn Table 1, the standard care typically involved basic respiratory exercises, general encouragement for mobility post-surgery, limited cognitive training, and basic emotional support across various modes, lacking structured programs for cognitive stimulation, social skill enhancement, or family involvement in rehabilitation plans. Conversely, the RAM-based CST group adopts a comprehensive approach. In the physiologic mode, patients engage in respiratory slow-speed training and a rehabilitation exercise regimen (Jonsson et al. 2019) to bolster respiratory control and physical function, thereby stimulating the brain, enhancing attention, concentration, and fostering cognitive improvement. This includes: 1) Preoperative Respiratory Training: Incorporating deep breathing exercises and mild physical exercises to enhance respiratory control and physical function. On the day of surgery, patients are encouraged to sit in a chair or at the bedside, gradually progressing to walking within the ward on the first postoperative day as per their individual needs, with or without assistance. 2) Deep Breathing Exercise Training: Involving 10 repetitions per set, thrice hourly with a one-minute interval between sets, continued until discharge. 3) Specific Exercises: Comprising shoulder elevation, shoulder flexion during deep breathing, horizontal shoulder abduction during deep breathing, and chest rotation exercises. Patients are advised to perform these exercises at least twice daily, repeating each exercise five times, starting on the first postoperative day and continuing throughout the initial month post-surgery. In the Self-Concept mode: 1) Preoperative Memory and Attention Training: Engaging in activities such as memory games, problem-solving, reading, or listening exercises to improve cognitive abilities. 2) Postoperative Memory and Attention Training: Conducting various activities twice weekly within the first month after surgery, aimed at enhancing memory and attention by evoking childhood memories, current events, sound, and word games, each session lasting one hour (Zubatsky et al. 2023). 3) Emotional Support Groups: Organized to provide psychological support and comfort. Under the Role Function mode, patients simulate daily activities pre- and postoperatively, offering cognitive stimulation by utilizing various cognitive skills. Tasks like household chores and shopping help in gradually restoring daily living skills, contributing to cognitive function improvement. Additionally, social skill courses are conducted to enhance patient sociability. Within the Interdependence mode, a family-based rehabilitation plan is devised, providing handbooks and supplementary materials. Caregivers encourage postoperative patients to continue similar cognitive stimulating activities at home, fostering cognitive improvement in the home setting. Nurses offer patients general instructions before discharge and deliver tailored information and education during phone calls, each lasting approximately 20 minutes.

Comparison of interventions between Roy adaptation model (RAM)-based cognitive stimulation therapy (CST) and standard care across different care modes.
Outcomes were measured at three time points: before surgery (preintervention), at discharge, and one-month post-discharge (postintervention). Cognitive function was evaluated using the Mini-Cognitive (Mini-Cog) test (Yajima et al. 2022), involving a three-item memory recall and a clock drawing test to assess visuo-spatial representation and executive function. Scores range on a 5-point scale, with normal cognition considered at scores of 4 and 5, mild impairment at scores of 2 and 3, and severe impairment for scores less than 2. Postoperative Delirium (POD) prevalence was determined by the Nursing Delirium Screening Scale (Nu-DESC) within the initial 48 hours post-surgery, defined as a Nu-DESC score ≥ 2 (Ristescu et al. 2021). The Hospital Anxiety and Depression Scale (HADS) is a 14-item tool used to evaluate nonphysical anxiety and depression symptoms (Du et al. 2020). It comprises two sets of 7 items each for measuring anxiety (HADS‐A) and depression (HADS‐D) separately. Scores on both HADS‐A and HADS‐D can range from 0 to 21 points, categorized as follows: No anxiety or depression (≤ 7), mild or moderate symptoms (8‐14). Additionally, Quality of Life (QoL) was assessed using the Short Form-36 Health Survey version 2 (SF36v2), a comprehensive 36-item survey (Salati et al. 2009). It measured eight health concepts: physical functioning (PF), role limitations due to physical problems (RP), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH).
Sample size calculationThe sample size calculation was performed using G*Power 3.1.9.2 software. At the one-month post-intervention mark, the RAM-based CST group (n = 140) displayed a Mini-Cog test score of 4.200 ± 0.923 (mean ± standard deviation, SD), while the control group (n = 140) showed a score of 3.600 ± 1.268, indicating a significant difference (P < 0.001). The effect size (d) calculated between these groups was 0.541. Statistical analysis employed a two-sample t-test (means: Wilcoxon-Mann-Whitney test, two groups), and the sample size calculation utilized post hoc power analysis with an α error probability set at 0.05. The resulting calculated power was determined to be 99.28%.
Statistical analysesAll statistical analyses were conducted using GraphPad Prism 8.0, with a significance level set at P < 0.05 to denote statistical significance. Frequency data are presented as n (%). The distribution analysis performed using the Shapiro-Wilk test indicated non-normality. Normally distributed data are reported as mean ± SD, while non-normally distributed data are expressed as median (interquartile range, IQR). Student t-tests were applied for normally distributed data when comparing between the two groups. For non-normally distributed data comparisons, the Mann-Whitney test was utilized. Group-wise comparisons across three time points were performed using the Friedman’s ANOVA test followed by Dunn’s multiple comparisons test. Furthermore, comparisons between two time points were analyzed using the Wilcoxon matched-pairs signed rank test.
Among the 280 patients included in the analysis (as shown in Table 2), the comparison between RAM-based CST and control groups encompassed various demographic factors. Notably, no statistically significant differences were observed in age (RAM-based CST: median 73 years, IQR 68-77; control: median 72 years, IQR 68-76; P = 0.422) and body mass index (BMI) (RAM-based CST: median 21.2 kg/m2, IQR 19.2-23.15; control: median 21.6 kg/m2, IQR 20.1-23.6; P = 0.126) between the two groups. Furthermore, there were no significant distinctions found in sex, marital status, education level, smoking status, tumor histology (adenocarcinoma vs. squamous cell carcinoma), or type of pulmonary resections (lobectomy vs. pneumonectomy) when comparing the RAM-based CST group with the control group (all P > 0.05). These suggested a well-matched baseline among enrolled patients, minimizing potential confounders that could affect study outcomes.

Demographic characteristics of enrolled patients.
RAM, Roy adaptation model; CST, cognitive stimulation therapy; BMI, body mass index.
The Shapiro-Wilk test revealed a non-normal distribution of Mini-Cog test scores. According to Fig. 1A, there was no significant difference in preoperative Mini-Cog test scores between the RAM-based CST group and the control group, as assessed by the Mann-Whitney test (P = 0.939). However, patients in the RAM-based CST group demonstrated higher Mini-Cog test scores compared to the control group upon discharge [4 (3-5) vs. 4 (2-5), P = 0.007] and post-intervention [4 (4-5) vs. 4 (3-5), P < 0.001], indicating enhanced cognitive function compared to the control group. The Friedman test ANOVA results indicated significant differences in Mini-Cog test scores at various time points for patients in the RAM-based CST group (all P < 0.05). Conversely, no significant differences were observed in the control group at different time points (all P > 0.05). As illustrated in Fig. 1B, the incidence of postoperative delirium in the control group was notably higher than that in the RAM-based CST group (20.71% vs. 10.71%, P = 0.032), highlighting the potential of this intervention in reducing post-surgical cognitive complications.

Improvement in postoperative cognitive function and reduction of delirium in elderly lung cancer patients with Roy adaptation model (RAM)-based cognitive stimulation therapy (CST) intervention.
A. Cognitive function was assessed using the Mini-Cognitive (Mini-Cog) test. B. Postoperative Delirium (POD) prevalence, ascertained with the Nursing Delirium Screening Scale (Nu-DESC) within the initial 2 days post-surgery, was defined by a Nu-DESC score ≥ 2. *P < 0.05.
Table 3 presented a comparison of anxiety and depression scores assessed using the HADS among elderly lung cancer patients undergoing RAM-based CST intervention and those in the control group at different time intervals. Before the intervention, no significant differences were noted in anxiety (RAM-based CST: 8.57%; control: 10.00%, P = 0.837) or depression (RAM-based CST: 10.71%; control: 12.14%, P = 0.851). Similar findings were observed at discharge for anxiety (RAM-based CST: 5.71%; control: 10.71%, P = 0.191) and depression (RAM-based CST: 7.86%; control: 11.43%, P = 0.418). However, following the intervention at 1 month, the RAM-based CST group exhibited notable reductions in both anxiety (3.57%) and depression (2.86%) compared to the control group (anxiety: 11.43%; depression: 12.86%). These results signify a significant improvement in anxiety and depression post-intervention within the RAM-based CST group compared to the control group (P = 0.021 and P = 0.003, respectively), indicating its efficacy in alleviating postoperative psychological distress. Utilizing Dunn’s multiple comparisons test (Fig. 2), our analysis revealed that, in contrast to the preoperative state, the RAM-based CST group at discharge and 1-month post-discharge (post-intervention) demonstrated a substantial decrease in HADS anxiety scores (at discharge: P = 0.020; post-intervention:P = 0.024) and HADS depression scores (at discharge: P = 0.002; post-intervention:P = 0.002). These findings underline the potential role of RAM-based CST in enhancing mental health outcomes among elderly lung cancer patients. Conversely, the control group did not display significant differences in HADS anxiety scores and HADS depression scores across these three time points (all P > 0.05).

Improved postoperative depression and anxiety in elderly lung cancer patients with Roy adaptation model (RAM)-based cognitive stimulation therapy (CST) intervention.
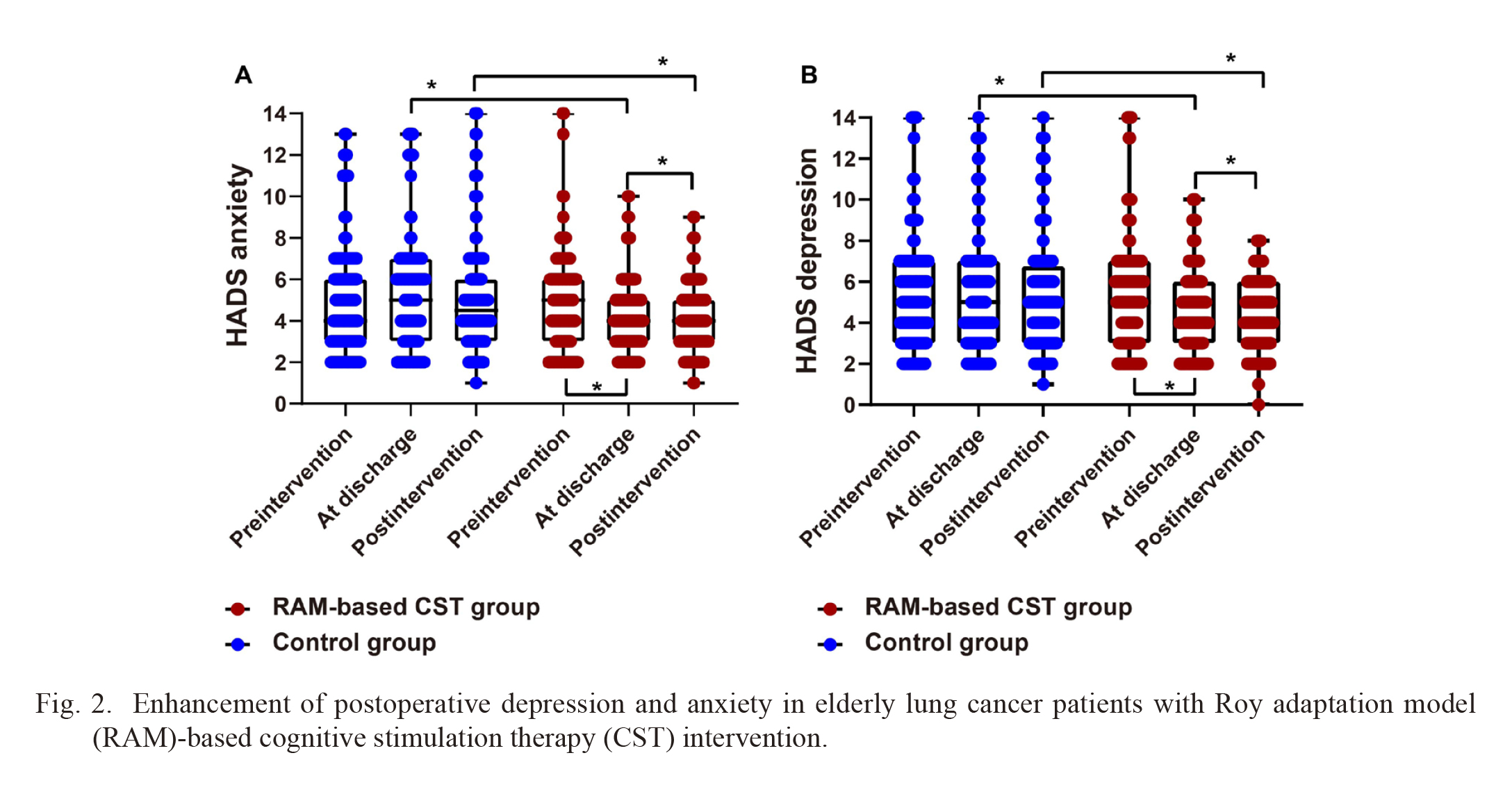
Enhancement of postoperative depression and anxiety in elderly lung cancer patients with Roy adaptation model (RAM)-based cognitive stimulation therapy (CST) intervention.
Hospital Anxiety and Depression Scale (HADS) includes two sets of 7 items for assessing anxiety (A. HADS‐A) and depression (B. HADS‐D), respectively. *P < 0.05.
Table 4 displayed notable improvements in SF36 subcategory scores for the RAM-based CST group at 1-month post-discharge (postintervention) compared to pre-surgery (all P < 0.001). Conversely, the control group showed no significant changes in scores between preintervention and postintervention (all P > 0.05). Furthermore, at postintervention, the RAM-based CST group exhibited significantly higher scores than the control group in RE [50 (43-57.75) vs. 48 (41.25-54), P = 0.030], MH [51 (45-57.75) vs. 49 (43-56), P = 0.043], GH [49 (41.25-57) vs. 46.5 (41-53), P = 0.034], BP [54 (48-63) vs. 53 (45.25-60), P = 0.044], and RP [45 (39-50) vs. 43 (38-49), P = 0.031], highlighting the potential role of RAM-based CST in fostering better postoperative QoL among elderly lung cancer patients.

Improved postoperative quality of life in elderly lung cancer patients with Roy adaptation model (RAM)-based cognitive stimulation therapy (CST) intervention.
*denotes comparison with the control group at postintervention.
VT, vitality; SF, social functioning; RE, role limitations due to emotional problems; MH; mental health; GH, general health perception; BP, bodily pain; RP, role limitations due to physical problems; PF, physical functioning.
Cognitive impairments following cancer treatment pose significant challenges to patients’ daily functioning and overall QoL. Previous studies have emphasized the intricate relationship between cancer therapies and cognitive decline, encompassing diverse cognitive domains such as processing speed, attention, memory, and executive function (Weyer-Jamora et al. 2021; Guran et al. 2022). Our study adds to this understanding by highlighting the critical role of preoperative cognitive status, correlating it with discharge destination and hospital stays (Larrabee et al. 2023). The significant enhancement in postoperative cognitive function among elderly NSCLC patients receiving RAM-based CST aligns with the theoretical framework’s focus on adaptation modes and their application in clinical settings (Flanagan 2018; Salazar-Barajas et al. 2018; Aydogdu et al. 2023). This structured intervention’s positive impact on cognitive recovery and stimulation offers a promising avenue for addressing postoperative cognitive impairments. Integrating RAM’s concepts into CST interventions appears to bolster cognitive rehabilitation strategies, potentially contributing to a better understanding of adaptation models in healthcare contexts.
Moreover, postoperative delirium remains a formidable challenge following surgical procedures, particularly among older adults. Its association with adverse outcomes, including prolonged hospitalization and increased morbidity and mortality rates, emphasizes the need for effective preventive measures (Shi et al. 2020; Crawford et al. 2021). Our findings highlight the potential of RAM-based CST in reducing the incidence of postoperative delirium, aligning with studies emphasizing cognitive stimulation’s role in preventing delirium across various patient populations (Tobar et al. 2017; O’Gara et al. 2020).
Furthermore, the observed improvements in anxiety, depression, and QoL dimensions among RAM-based CST participants resonate with previous research, underlining the intervention’s holistic approach (Lok et al. 2020; Erol Ursavas and Karayurt 2021). The multifaceted nature of RAM-based CST, incorporating cognitive, emotional, and social dimensions, emphasizes the comprehensive care approach essential for addressing the complex needs of cancer patients undergoing surgery.
In clinical practice, the integration of RAM-based CST interventions could potentially optimize care pathways for elderly NSCLC patients’ post-surgery. Implementation strategies focusing on cognitive stimulation, emotional support, and functional rehabilitation, guided by RAM’s adaptive modes, hold promise in enhancing recovery and promoting better patient outcomes.
However, acknowledging the study’s limitations is crucial for contextualizing these findings. The study’s single-center design and relatively moderate sample size might limit result generalizability. Additionally, longer-term follow-up assessments beyond the one-month post-discharge period would provide valuable insights into the sustainability of the observed improvements.
In conclusion, the findings underscore the potential of RAM-based CST interventions in improving postoperative outcomes among elderly NSCLC patients. The multifaceted approach targeting various dimensions of adaptation within the RAM framework offers a promising avenue for addressing cognitive impairments, psychological distress, and enhancing overall well-being. Future research endeavors should focus on larger-scale studies with extended follow-up periods to further validate and refine the implementation of these interventions in diverse clinical settings.
The authors declare no conflict of interest.