2024 Volume 263 Issue 2 Pages 115-121
2024 Volume 263 Issue 2 Pages 115-121
Conventional coronal CT scans of paranasal sinuses, aligned perpendicularly to the nasal floor, often deviate significantly from the endoscopic view during sinus surgery. This discrepancy complicates the interpretation of anatomical structures. In response, we propose the utilization of anteriorly tilted coronal CT slices to enhance anatomical understanding. These slices align more closely with the endoscopic view, fostering an intuitive grasp of paranasal sinus anatomy. This study aims to quantify the tilt of the endoscope to the nasal floor during endoscopic sinus surgery. To figure out the tilt of the endoscopically true coronal slices, we calculated the tilt of the endoscope to the nasal floor in the operative setting by taking pictures of the operation and measuring the image and sagittal CT. Fourteen patients (25 sides of paranasal sinuses) were analyzed. Endoscope tilts to the nasal floor were measured at different anatomical landmarks: 16.2 ± 9.7 degrees (lower edge of ground lamella), 29.8 ± 7.9 degrees (central ground lamella), 62.3 ± 10.1 degrees (most superior part), and 25.6 ± 7.0 degrees (optic canal). In conclusion, we showed the actual tilt of the endoscope to the nasal floor during endoscopic sinus surgery. A 30-degree anteriorly tilted coronal scan for frontal recess and sphenoid sinus is more intuitive than a traditional coronal scan, which helps surgeons understand the complex sinus anatomy.
Computed tomography (CT) scans play a crucial role in guiding endoscopic sinus surgery, providing essential insights into the intricate anatomy of the paranasal sinuses. Multiplanar reconstruction (MPR) CT, incorporating axial, coronal, and sagittal views, has become a standard approach in visualizing these anatomical structures (Campbell et al. 2009). The interactive nature of MPR CT images enhances our ability to comprehend complex sinus anatomy (Rimmer et al. 2019). MPR CT, by presenting a single reference point across all three planes, has significantly advanced our understanding, particularly in navigating the complexities of the frontal recess. However, despite these advancements, surgical interventions involving the frontal recess and sphenoid sinus persist as formidable challenges in the field (Wada et al. 2015; Wormald et al. 2016). This underscores the need for innovative images to further enhance anatomical comprehension in these challenging areas.
In the past, prior to the availability of CT reconstruction technology, coronal slices were captured while the patient assumed a prone position, with the chin hyperextended on the CT scanner bed. The scanner gantry was angled perpendicular to the patient’s hard palate (Zinreich et al. 1990, 1998). This traditional coronal scan has been considered the one cross-sectional plane that best correlates with the surgeon’s field of view, and the coronal section is made in the same way in the age of MPR CT. However, the endoscope is directed upward rather than parallel to the nasal floor in the operative settings. Imagining an intraoperative endoscopic view before the operation is challenging even with the MPR CT because the conventional coronal plane does not mirror the actual endoscopic view.
The tilt of the endoscope to the nasal floor changes during surgery depending on the site manipulated. The actual endoscopic tilt cannot be calculated on MPR CT because the external nose is flexible, and the nares are upwardly lifted during surgery. To understand the tilt of the endoscope during surgery and know the anterior tilt that needs to be applied on traditional coronal slices, we measured the angle of the endoscope during the surgery. We calculated the anterior tilt using the CT.
We evaluated patients who underwent endoscopic sinus surgery at Tohoku Kosai Hospital, Japan, between October 2023 and November 2023. Written informed consent was obtained from all the patients, including their consent to participate in the study and publish the findings. This study was approved by the institutional review board of Tohoku Kosai Hospital according to the ethical standards of the Committee on Human Experimentation of the institution (kkrtohoku-202310otor2-S1-01) and in accordance with the Helsinki Declaration of 1975, as revised in 1983.
All patients underwent endoscopic sinus surgery with the frontal sinus opening, and the optic canal was revealed to be prominent. The operation was performed in the following steps: 1) Anterior ethmoidectomy, frontal sinusotomy. 2) The 0-degree endoscope directed to the mid portion of the ground lamella, the lower edge of the ground lamella, and the frontal sinus, i.e., the uppermost angle (Fig. 1A-C). 3) Posterior ethmoidectomy and sphenoidotomy. 4) The 0-degree endoscope is directed to the optic canal prominence (Fig. 1D). The pictures of steps 2) and 4) were taken from the patient’s lateral side with a distance of 2 m with the smartphone camera (iPhone SE, model MMYD3J/A, Apple Inc, Cupertino, CA) (Fig. 2A, B).
The midsagittal slice was defined as the slice that shows the largest crista galli on sagittal slices. The skin surface of the philtrum was used to measure the angle (Fig. 2C). When the line of the nasal floor is not identifiable because of the vomer, one or two slices (each slice = 0.5mm) away from the midsagittal slice were used to trace the nasal floor. The tilt of the endoscope to the nasal floor (γ) in Fig. 2C is equivalent to the ideal anterior tilt of the coronal scan. The tilt of the endoscope to the nasal floor, γ in Fig. 2C, is calculated as 180 degrees minus the angle between the endoscope and the philtrum (denoted as α in Fig. 2B, corresponding to α in Fig. 2C) minus the angle between the philtrum and the nasal floor (measured in sagittal CT and represented as β in Fig. 2C). During surgery, we position patients in a 20-degree reverse Trendelenburg position. However, this specific angle has no impact on the measured angles, as the angle between the endoscope and the philtrum (α in Fig. 2B) remains unaffected by the patients’ positioning. Reconstruction of anterior tilted coronal slices was made using SYNAPSE VINCENT Ver. V.6.3 (FUJIFILM Corporation, Japan). Anteriorly tilted coronal CT images were obtained by clicking and holding the reference line on the sagittal scan, then moving it counterclockwise.

Intraoperative images of the right nasal cavity with 0-degree endoscope of a 63-year-old female.
A. The lower edge of the ground lamella is seen. B. The center of the ground lamella is visualized. C. The maximum tilt of the endoscope. The frontal sinus and frontal septal cell are seen. D. The optic canal is at the center of the view.

How we measured the endoscopic tilt for the nasal floor during operation.
A. We take a picture of the nose and endoscope from 2 m away from the patient at the same height as the nose. B. Magnified picture of A. α indicates the angle of the endoscope and the philtrum. C. Midsagittal CT scan. A yellow line indicates a supposed 0-degree endoscope. α indicates the angle of the endoscope and the philtrum and measured on the picture (B). β indicates the angle of the philtrum and the nasal floor and measured here. γ indicates the tilt of the endoscope from the nasal floor and derived using α and β.
Data are presented as means ± standard deviation. The difference in the tilt of the endoscope to the nasal floor (γ in Fig. 2C) between sexes was compared using the Mann-Whitney U test. Regression analysis was performed to determine the effect of age on the tilt of the endoscope to the nasal floor. Statistical analysis of all data was performed using Stata version 14.0 (StataCorp, College Station, TX, USA). A p-value < 0.05 was considered statistically significant.
Fourteen patients were included in the study. The characteristics of the patient’s background are summarized in Table 1. The tilts of the endoscope to the nasal floor (represented as γ in Fig. 2C) focusing on the lower edge of the ground lamella, the mid portion of the ground lamella, the frontal sinus, and the optic canal were 16.2 ± 9.7, 29.8 ± 7.9, 62.3 ± 10.1, and 25.6 ± 7.0 degrees respectively (Fig. 3). The tilt of the 0-degree endoscope dealing with frontal recess is between the range of the mid portion of the ground lamella and the frontal sinus. We present the 30-degree anterior tilted coronal slice and regular coronal slice for a frontal recess (Fig. 4) and Onodi cell/sphenoid sinus separation (Fig. 5). Anterior tilted coronal slices are more comparable to the endoscopic view than traditional coronal slices (Figs. 1B, C, 4A, C and 5A-C). No statistical differences were observed in the tilt from the nasal floor between the sexes in any position (Table 2). Age also had no impact on the tilt from the nasal floor (Table 3).
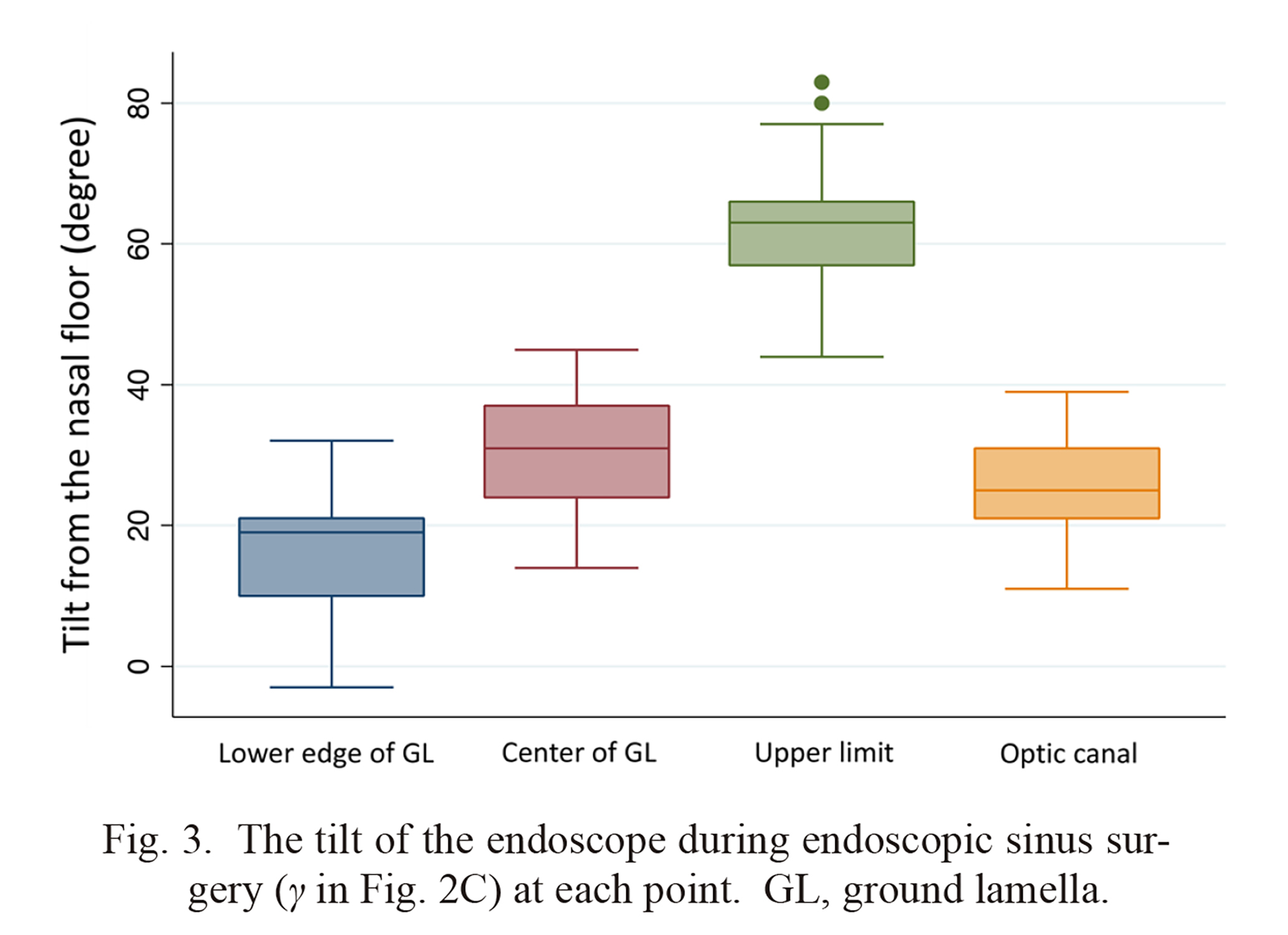
The tilt of the endoscope during endoscopic sinus surgery (γ in Fig. 2C) at each point. GL, ground lamella.

The CT images of the 63-year-old female patient presented in Fig. 1.
A. traditional coronal slice. B sagittal slice. The vertical red line corresponds to the conventional coronal slice (A). C. 30-degree anteriorly tilted coronal slice. D. sagittal slice. The oblique red line corresponds to the anteriorly tilted coronal slice (C).

The CT images and intraoperative endoscopic view of a 53-year-old female.
A. traditional coronal slice. B. Endoscopic view at the left side optic canal. C. 30-degree anteriorly tilted coronal slice. D. Sagittal slice. The oblique red line corresponds to the anteriorly tilted coronal slice (C). yellow arrow, the separation between the posterior ethmoid cell and the sphenoid sinus.

Patients’ background.
ECRS, eosinophilic chronic rhinosinusitis

Tilt from the nasal floor (degree) between the sexes.
GL, ground lamella

Effect of age (years) on the tilt from the nasal floor (degree).
GL, ground lamella; Coef, coefficient; CI, confidence interval
We measured the tilt of the 0-degree endoscope aiming at the critical landmark structures to the nasal floor. The tilt while visioning the center of the ground lamella and optic canal was around 30 degrees. The maximum tilt visioning at the frontal sinus was around 60 degrees. These tilts are far from 0 degrees, in which traditional coronal CT slices correspond to the endoscopic view.
Traditional coronal CT slices are cut perpendicular to the patient’s hard palate/nasal floor (Zinreich et al. 1990, 1998). After the MPR CT was introduced and slicing became possible with any tilt, the coronal slice continued perpendicular to the nasal floor. There are many merits and reasons that coronal slices are perpendicular to the hard palate. 1) The nasal floor is a conspicuous structure with thick bones and straight, a significant landmark to set as a common reference point for coronal slices. 2) The nasal floor is perpendicular to the face, and there is no structure comparable to the nasal floor suitable for the reference structure. However, as shown in this study, the endoscope always has an upward tilt during endoscopic sinus surgery. The discrepancy between the endoscopic view and coronal CT images makes endoscopic sinus surgery more challenging, especially for resident surgeons. We need to reconstruct the operative images in our mind using 3-direction CT images. This reconstruction in our mind becomes more manageable and straightforward using anteriorly tilted coronal slices.
One of the most challenging parts of the endoscopic sinus surgery is around the frontal recess (Wormald et al. 2016). Identifying and opening the frontal sinus requires an anatomical understanding of the anatomical structure and surgical skills. Poor understanding of the anatomy leads to prolonged operation, unsuccessful opening of the frontal sinus, or, in worst case, cerebrospinal fluid leakage, anterior ethmoidal artery hemorrhage, and orbital complications. The three planar CTs with each slice interactively related have made understanding of the frontal recess significantly (Rimmer et al. 2019). Anatomical classification of the frontal recess and anatomical terminology of ethmoid cells at the frontal recess have made frontal sinus surgery manageable for many rhinologists (Wormald et al. 2016). Furthermore, 3D images of frontal recesses can be made with special software and some effort. (Moral et al. 2007; Reitzen et al. 2010). The methods mentioned above are helpful but require significant mental effort to imagine how the operative view will appear.
Anteriorly tilted coronal CT has rarely been mentioned before, and we found one article that shows the anteriorly tilted coronal CT on a figure without any comments on its usefulness in manuscript (Dassi et al. 2020). They call it an oblique section for the true coronal plane. We want to emphasize the benefit of anteriorly tilted coronal CT because it is the slice perpendicular to the endoscope. The anteriorly tilted coronal CT represents the operative view more than traditional coronal CT (Figs. 1B, C and 4A, C). Making anteriorly tilted coronal slices is simple; click and hold the reference line on the sagittal scan and move counterclockwise. During the endoscopic sinus surgery, the tilt varies depending on the operation site from 16.2 ± 9.7 to 62.3 ± 10.1 degrees. We chose 30 degrees as a standard tilt for anteriorly tilted coronal slices because when the endoscope aims at the center of the ground lamella, the tilt is 29.8 ± 7.9. When the endoscope has a maximum tilt, it is 62.3 ± 10.1. We usually switch to a 70-degree endoscope when manipulating inside the frontal sinus where normal axial slices represent the endoscopic view. The tilt can be determined by the surgeon’s preference and the individual patient’s anatomical variance. We found no influence of sex or age on the endoscopic tilt from the nasal floor in our series.
Sphenoid sinus surgery is the next challenge after the frontal sinus surgery. The optic canal and the internal carotid artery are two primary anatomical structures facing the sphenoid sinus. The relationship between the most posterior ethmoid cell and the sphenoid sinus is highly variable (Wada et al. 2015). Using the three planar CTs and the classification of the sphenoid sinus for endoscopic sinus surgery, understanding the anatomical structures around the sphenoid sinus became easier. However, similar to the frontal recess surgery, you need to imagine the anatomical structures in your mind before the surgery using CT, which is difficult. As we have shown, the tilt of the endoscope aiming at the optic canal is 25.6 ± 7.0 degrees. The separation between the most posterior ethmoid cell and the sphenoid sinus appears on traditional coronal slices more vertically than in the endoscopic view (Fig. 5). In general, the separation between the most posterior ethmoid cell and the sphenoid sinus appears lower than expected according to conventional coronal CT scans. We chose 30 degrees as the standard tilt for the optic canal because it is the same as for the frontal recess and is a familiar angle used by a set square.
Anteriorly tilted coronal CT shows different images compared to traditional coronal CT regarding important structures, including the lateral lamella of the cribriform plate, lamina papyracea, sphenoid sinus pneumatization, Haller cell, and anterior ethmoidal artery. The lateral lamella of the cribriform plate appears longer in the anteriorly tilted coronal CT (Fig. 6A, D). The lamina papyracea appears rounder in the anteriorly tilted coronal CT (Fig. 6A, D). The vital structures facing the sphenoid sinus, including the optic canal and internal carotid artery prominence, appear less conspicuous on anteriorly tilted coronal CT than on traditional coronal CT (Fig. 6C, F). The separation of the maxillary sinus and the Haller cell appears deeper in the anteriorly tilted coronal CT (Fig. 6B, E). The anterior ethmoidal artery appears more prominent on the anteriorly tilted coronal CT than traditional coronal CT (Fig. 6A, D).
A significant limitation of our study is the selection of a 30-degree anterior tilted coronal scan without rigorous mathematical validation compared to the traditional coronal scan. Our assertion is based more on intuition than on quantifiable or statistical methodology. While we have suggested the potential utility of the anterior tilted coronal scan, further investigation is imperative to substantiate its effectiveness. Additionally, our focus on the 0-degree endoscope view neglects exploration of frontal sinus surgery under the 70-degree endoscope. The frontal recess viewed with an angled endoscope corresponds to normal axial CT slices. Consequently, we did not deem it necessary to modify the normal axial slices. We did not measure the angle of the endoscope in pediatric patients due to the limited opportunities to perform endoscopic sinus surgery in this age group.
In conclusion, since examining anteriorly tilted coronal CT is very simple, we propose using it combined with traditional coronal CT, which has been familiar to us for a long time. Anterior tilted coronal CT represents the endoscopic view more similarly to conventional coronal slices.

CT images of a 31-year-old male.
A - C. Traditional coronal slices. D - F. 30-degree anteriorly tilted coronal slices. A, D. Anterior ethmoidal artery and lateral plate of the cribriform plate are seen. B, E. Left Haller cell is seen. C, F. The sphenoid sinus is seen.
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
The authors declare no conflict of interest.