Current issue
Displaying 1-50 of 71 articles from this issue
PICTORIAL ESSAY
-
Article type: PICTORIAL ESSAY
2025Volume 10 Pages e2025-0013
Published: November 14, 2025
Released on J-STAGE: November 14, 2025
Download PDF (2200K)
TECHNICAL NOTE
-
Article type: TECHNICAL NOTE
2025Volume 10 Pages e2025-0034
Published: October 31, 2025
Released on J-STAGE: October 31, 2025
Download PDF (602K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2025-0005
Published: October 31, 2025
Released on J-STAGE: October 31, 2025
Download PDF (468K)
TECHNICAL NOTE
-
Article type: TECHNICAL NOTE
2025Volume 10 Pages e2025-0022
Published: October 31, 2025
Released on J-STAGE: October 31, 2025
Download PDF (388K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2025-0023
Published: October 21, 2025
Released on J-STAGE: October 21, 2025
Download PDF (463K)
TECHNICAL NOTE
-
Article type: TECHNICAL NOTE
2025Volume 10 Pages e2025-0030
Published: October 21, 2025
Released on J-STAGE: October 21, 2025
Download PDF (1021K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0008
Published: October 21, 2025
Released on J-STAGE: October 21, 2025
Download PDF (698K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0066
Published: October 21, 2025
Released on J-STAGE: October 21, 2025
Download PDF (657K)
TECHNICAL NOTE
-
Article type: TECHNICAL NOTE
2025Volume 10 Pages e2025-0027
Published: October 21, 2025
Released on J-STAGE: October 21, 2025
Download PDF (759K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2025-0002
Published: September 30, 2025
Released on J-STAGE: September 30, 2025
Download PDF (932K)
TECHNICAL NOTE
-
Article type: TECHNICAL NOTE
2025Volume 10 Pages e2025-0012
Published: September 30, 2025
Released on J-STAGE: September 30, 2025
Download PDF (507K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2025-0014
Published: September 17, 2025
Released on J-STAGE: September 17, 2025
Download PDF (3365K) -
Article type: REVIEW
2025Volume 10 Pages e2025-0029
Published: September 17, 2025
Released on J-STAGE: September 17, 2025
Download PDF (428K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2025-0011
Published: September 17, 2025
Released on J-STAGE: September 17, 2025
Download PDF (664K) -
Article type: CASE REPORT
2025Volume 10 Pages e2025-0016
Published: September 17, 2025
Released on J-STAGE: September 17, 2025
Download PDF (613K)
GUIDELINE
-
Article type: GUIDELINE
2025Volume 10 Pages e2024-0025
Published: September 03, 2025
Released on J-STAGE: September 03, 2025
Download PDF (225K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2025-0007
Published: September 03, 2025
Released on J-STAGE: September 03, 2025
Download PDF (941K) -
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0038
Published: September 03, 2025
Released on J-STAGE: September 03, 2025
Download PDF (412K) -
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0053
Published: September 03, 2025
Released on J-STAGE: September 03, 2025
Download PDF (273K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0061
Published: September 03, 2025
Released on J-STAGE: September 03, 2025
Download PDF (750K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0041
Published: September 03, 2025
Released on J-STAGE: September 03, 2025
Download PDF (641K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2024-0063
Published: September 03, 2025
Released on J-STAGE: September 03, 2025
Download PDF (870K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2025-0009
Published: August 21, 2025
Released on J-STAGE: August 21, 2025
Download PDF (466K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0042
Published: August 01, 2025
Released on J-STAGE: August 01, 2025
Download PDF (217K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2024-0057
Published: August 01, 2025
Released on J-STAGE: August 01, 2025
Download PDF (2142K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0023
Published: August 01, 2025
Released on J-STAGE: August 01, 2025
Download PDF (715K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2024-0060
Published: August 01, 2025
Released on J-STAGE: August 01, 2025
Download PDF (436K)
TECHNICAL NOTE
-
Article type: TECHNICAL NOTE
2025Volume 10 Pages e2025-0004
Published: August 01, 2025
Released on J-STAGE: August 01, 2025
Download PDF (276K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2025-0003
Published: August 01, 2025
Released on J-STAGE: August 01, 2025
Download PDF (445K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0044
Published: July 23, 2025
Released on J-STAGE: July 23, 2025
Download PDF (338K)
CASE REPORT
-
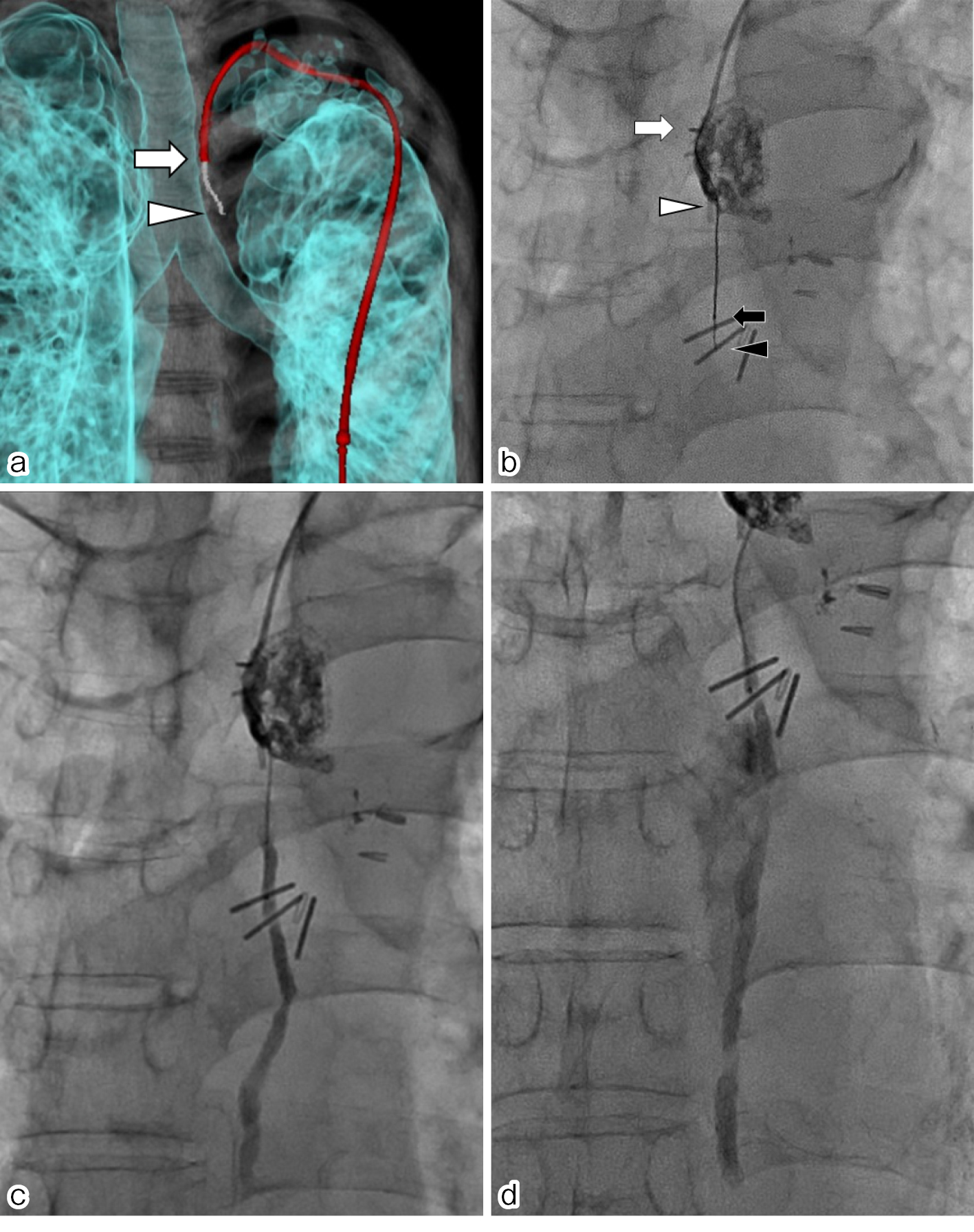
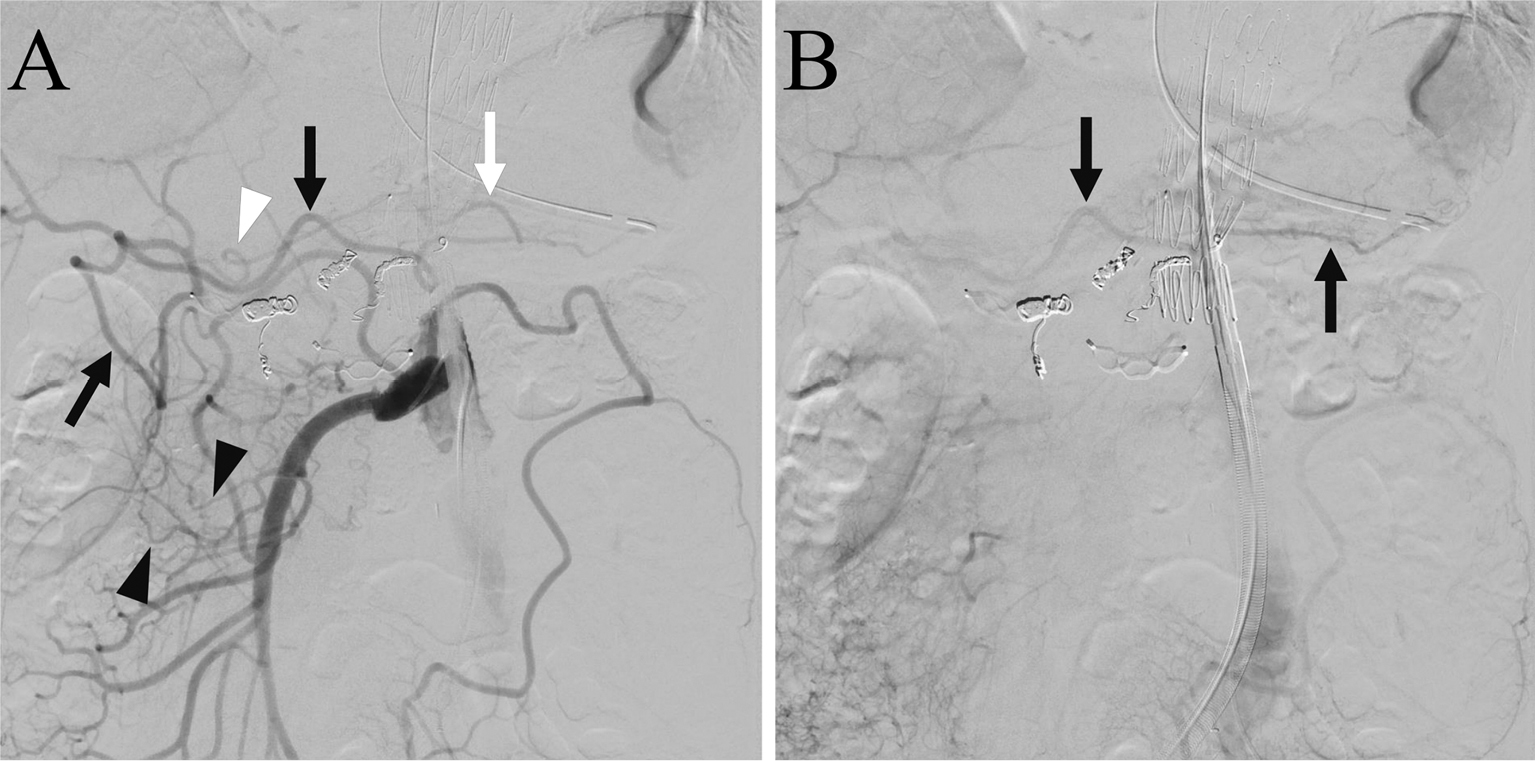
Thoracic Duct Embolization via Retrograde Cannulation of a Leaking Stump through the Thoracic CavityArticle type: CASE REPORT
2025Volume 10 Pages e2024-0049
Published: July 23, 2025
Released on J-STAGE: July 23, 2025
Download PDF (896K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0051
Published: July 23, 2025
Released on J-STAGE: July 23, 2025
Download PDF (560K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0047
Published: June 30, 2025
Released on J-STAGE: June 30, 2025
Download PDF (1001K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2024-0052
Published: June 30, 2025
Released on J-STAGE: June 30, 2025
Download PDF (851K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0031
Published: June 13, 2025
Released on J-STAGE: June 13, 2025
Download PDF (180K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0034
Published: June 13, 2025
Released on J-STAGE: June 13, 2025
Download PDF (933K) -
Article type: CASE REPORT
2025Volume 10 Pages e2024-0064
Published: June 13, 2025
Released on J-STAGE: June 13, 2025
Download PDF (442K)
ORIGINAL RESEARCH
-
Article type: ORIGINAL RESEARCH
2025Volume 10 Pages e2024-0068
Published: June 13, 2025
Released on J-STAGE: June 13, 2025
Download PDF (566K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0048
Published: May 29, 2025
Released on J-STAGE: May 29, 2025
Download PDF (931K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2024-0039
Published: April 25, 2025
Released on J-STAGE: April 25, 2025
Download PDF (2647K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2024-0014
Published: April 25, 2025
Released on J-STAGE: April 25, 2025
Download PDF (1027K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2024-0040
Published: April 25, 2025
Released on J-STAGE: April 25, 2025
Download PDF (575K) -
Article type: REVIEW
2025Volume 10 Pages e2024-0037
Published: April 25, 2025
Released on J-STAGE: April 25, 2025
Download PDF (573K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2022-0035
Published: March 28, 2025
Released on J-STAGE: March 28, 2025
Advance online publication: August 11, 2023Download PDF (98K) -
Article type: REVIEW
2025Volume 10 Pages e2023-0009
Published: March 28, 2025
Released on J-STAGE: March 28, 2025
Advance online publication: December 14, 2023Download PDF (1349K) -
Article type: REVIEW
2025Volume 10 Pages e2023-0027
Published: March 28, 2025
Released on J-STAGE: March 28, 2025
Advance online publication: March 27, 2024Download PDF (1670K) -
Article type: REVIEW
2025Volume 10 Pages e2023-0026
Published: March 28, 2025
Released on J-STAGE: March 28, 2025
Advance online publication: March 27, 2024Download PDF (938K)
CASE REPORT
-
Article type: CASE REPORT
2025Volume 10 Pages e2023-0036
Published: March 28, 2025
Released on J-STAGE: March 28, 2025
Advance online publication: August 07, 2024Download PDF (762K) -
Article type: CASE REPORT
2025Volume 10 Pages e2024-0006
Published: March 28, 2025
Released on J-STAGE: March 28, 2025
Advance online publication: August 07, 2024Download PDF (1289K)
REVIEW
-
Article type: REVIEW
2025Volume 10 Pages e2023-0042
Published: March 28, 2025
Released on J-STAGE: March 28, 2025
Advance online publication: October 04, 2024Download PDF (561K)