2014 Volume 37 Issue 6 Pages 947-953
2014 Volume 37 Issue 6 Pages 947-953
It is thought that both selective serotonin reuptake inhibitors (SSRIs) and non-steroidal anti-inflammatory drugs (NSAIDs) can cause the adverse reaction of upper gastrointestinal hemorrhage (UGIH). To evaluate differences in the probability of UGIH occurring when SSRIs, NSAIDs, or both combined are administered, the authors performed a systematic review of related articles and a meta-analysis of data in those articles, which were identified by searching the literature published between 1999 and 2012 using PubMed, Scirus, and Google Scholar. The odds ratios were calculated using the Mantel–Haenszel method. The integrated odds ratios for SSRIs only, NSAIDs only, and the combination were 1.73 (0.65–2.82), 2.55 (1.51–3.59), and 4.02 (2.89–5.15), respectively. Use of the combination resulted in an odds ratio 2.32 times higher than use of either alone. Since the combination of SSRIs and NSAIDs resulted in a significantly higher risk of UGIH than either type of drug alone, clinicians should avoid use of the combination as much as possible. If it is necessary to administer both kinds of drugs, the minimum dosage should be prescribed for the shortest time period possible, and patients, particularly elderly patients, should be closely monitored for development of UGIH and other complications.
Selective serotonin reuptake inhibitors (SSRIs) are widely used in the treatment of panic and obsessive compulsive disorders in many countries, and the effects have been confirmed. Usage of SSRIs is increasing because of their low toxicity compared with classical antidepressants, which have a different mode of action.1) Thus, among the many kinds of antidepressants available, SSRIs are currently the most commonly prescribed, and their usage has steadily increased in elderly patients with depression in particular.2) However, SSRIs are reported to have some specific adverse reactions, such as upper gastrointestinal hemorrhage (UGIH).3)
Non-steroidal anti-inflammatory drugs (NSAIDs), which are widely used over-the-counter drugs, have also been shown to be associated with a risk of UGIH.1) Although SSRIs and NSAIDs are sometimes administered in combination,4) the harmful effects of this combination have not been clarified, as the Food and Drug Administration (FDA) has not accurately analyzed the risk of UGIH resulting from combination use of SSRIs and NSAIDs.3)
Therefore, we collected data for cases of UGIH resulting from the administration of SSRIs alone, NSAIDs alone, and combination use reported between 1999 and 2012, and performed a meta-analysis in order to analyze the risk of UGIH associated with combination use of SSRIs and NSAIDs.
We searched the literature through PubMed, Scirus, and Google Scholar for articles published between 1999 and 2012 using the following terms: “NSAIDs other drug interaction,” “adverse interaction between NSAIDs and other drugs,” “selective serotonin reuptake inhibitors and risk of upper gastrointestinal tract bleeding,” “NSAIDs, serotonin reuptake inhibitors, and risk of upper gastrointestinal bleeding,” “risk of gastrointestinal adverse effects under SSRI NSAID,” “NSAIDs tricyclic antidepressant adverse interactions,” and “NSAIDs antidepressant risk of upper gastrointestinal bleeding.”
Selection CriteriaEnrolled articles satisfied the following criteria:
a) There was no language restriction initially. However, only articles written in English were ultimately selected, as no articles in other languages were found to be acceptable after applying the following three criteria.
b) Human data only.
c) Since no intervention studies could be extracted, only case control studies were selected.
d) Only studies in which all three cases (SSRI alone, NSAIDs alone, and combination use) were analyzed for UGIH risk were selected. In addition, both odds ratios (ORs) and 95% confidence intervals (CIs), as well as the number of cases and controls had to be described.
Analysis and Reporting MethodsWe confirmed that the data had no significant publication bias using funnel plots and the regression analysis proposed by Macaskil et al.5) and then integrated all ORs using the Mantel–Haenszel method. In addition, forest plots were produced to present the results of the studies. The selected studies were checked against the STROBE statement.6) As a result, the studies that were used for this meta-analysis roughly conformed to the STROBE statement.
The data were analyzed and reported according to the PRISMA statement.7)
In total, 51 reports from the following countries were selected: United States (U.S.A.), Japan, United Kingdom (U.K.), Canada, Denmark, Italy, Spain, Germany, Norway, Finland, Mexico, India, Netherlands, Sweden, Turkey, Hungary, Poland, Libya, Romania, and Belgium (Table 1). After reviewing the titles and summaries of these 51 reports, we identified 15 (U.S.A., 5; U.K., 4; Denmark, 3; Spain, 1; Finland, 1; and Japan, 1) reports that provisionally satisfied the selection criteria.
| Country | Number of reports found | Number of reports included in the study |
|---|---|---|
| United States | 11 | 2 |
| Japan | 6 | 0 |
| United Kingdom | 5 | 2 |
| Denmark | 5 | 1 |
| Canada | 3 | 0 |
| Italy | 2 | 0 |
| Spain | 2 | 1 |
| Germany | 2 | 0 |
| Norway | 2 | 0 |
| Finland | 2 | 0 |
| Mexico | 2 | 0 |
| India | 1 | 0 |
| Netherland | 1 | 0 |
| Sweden | 1 | 0 |
| Turkey | 1 | 0 |
| Hungary | 1 | 0 |
| Poland | 1 | 0 |
| Libya | 1 | 0 |
| Romania | 1 | 0 |
| Belgium | 1 | 0 |
| Total | 51 | 6 |
These 15 reports were then systematically reviewed, and six were included in the study (U.S.A., 2; Denmark, 1; U.K., 2; and Spain, 1). Among these six reports,2,3,8–11) one was a study on the drug interaction between SSRI and NSAIDs,9) and four also included the interactions of non-SSRIs (serotonin noradrenaline receptor inhibitors; SNRIs) or tricyclic antidepressants (TCAs).2,8,10,11) The remaining study was a meta-analysis on the interaction between SSRIs and NSAIDs.3) The total number of cases included in these six studies was 223947 (Fig. 1).

n indicates number of selected studies.
The funnel plots of SSRI alone, NSAID alone, and combination use are shown in Figs. 2–4. Although the numbers involved were not sufficient to demonstrate that there was no significant bias, the figures visually show that the data are not so obviously biased that they could not be used for this meta-analysis. The data in the reports resulted in an approximately zero slope after performing regression analysis per Macaskil et al. (Table 2), also indicating that the data were not biased.
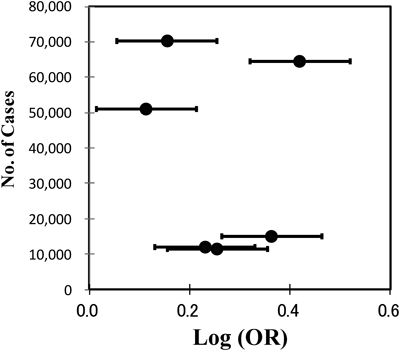


The combined ORs for use of SSRIs alone, use of NSAIDs alone, and combination use were 1.73 (0.65–2.82), 2.55 (1.51–3.59), and 4.02 (2.89–5.15), respectively (Tables 3–6, Fig. 5).
| Independent variables | Coefficients | Standard errors | t | Pr>| t | | |
|---|---|---|---|---|---|
| SSRI+NSAIDs | Intercept | 0.475 | 0.199 | 2.394 | 0.062 |
| β | 0.000 | 0.000 | 0.199 | 0.850 | |
| SSRI | Intercept | 0.193 | 0.095 | 2.031 | 0.098 |
| β | 0.000 | 0.000 | 0.366 | 0.729 | |
| NSAIDs | Intercept | 0.344 | 0.118 | 2.907 | 0.034 |
| β | 0.000 | 0.000 | 0.354 | 0.738 |

LL, lower limit; UL, upper limit; CI, confidence interval.
The forest plots, which incorporate ORs of the enrolled studies excluding that of patients older than 80 years, showed that use of NSAIDs alone and combination use resulted in a significantly higher risk of UGIH than that of control subjects. In addition, integrated ORs show that combination use had an additive effect on the risk of UGIH (Tables 3–6, Figs. 6–8).
| Case number | SSRIs were administered | SSRIs were NOT administered | Total number of subjects | LL 95% CI | UL 95% CI | OR | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| UGIH | Controls | Total | UGIH | Controls | Total | ||||||
| 7 | SSRI only (all patients)8) | 253 | 11008 | 11261 | 522 | 52634 | 53156 | 64417 | 2.24 | 3.07 | 2.63 |
| 6 | SSRI only11) | 284 | 8907 | 9191 | 931 | 40849 | 41780 | 50971 | 1.13 | 1.5 | 1.3 |
| 5 | SSRI only9) | 22 | 1299 | 1321 | 105 | 9895 | 10000 | 11321 | 1.1 | 2.9 | 1.8 |
| 4 | SSRI only2) | 62 | 1490 | 1552 | 1881 | 66709 | 68590 | 70142 | 1.09 | 1.89 | 1.43 |
| 3 | SSRI only (over age of 80)8) | 59 | 2763 | 2822 | 130 | 12069 | 12199 | 15021 | 1.66 | 3.2 | 2.31 |
| 2 | SSRI only10) | 40 | 606 | 646 | 326 | 11103 | 11429 | 12075 | 1.01 | 2.8 | 1.7 |
| 1 | Integrated OR | 26793 | 197154 | 223947 | 0.6451 | 2.8224 | 1.7337 | ||||
Integrated ORs from each article’s data as results of observational studies of SSRI and NSAIDs exposure and association with UGIH. LL, lower limit; UL, upper limit; CI, confidence interval; OR, odds ratio.
| Case number | NSAIDs were administered | NSAIDs were NOT administered | Total number of subjects | LL 95% CI | UL 95% CI | OR | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| UGIH | Controls | Total | UGIH | Controls | Total | ||||||
| 7 | NSAIDs only (all patients)8) | 1871 | 9390 | 11261 | 4700 | 48456 | 53156 | 64417 | 2.05 | 2.33 | 2.19 |
| 6 | NSAIDs only11) | 1714 | 7477 | 9191 | 3089 | 38691 | 41780 | 50971 | 2.65 | 3.03 | 2.83 |
| 5 | NSAIDs only9) | 173 | 1148 | 1321 | 642 | 9358 | 10000 | 11321 | 2.3 | 3.5 | 2.8 |
| 4 | NSAIDs only2) | 263 | 1289 | 1552 | 5266 | 63324 | 68590 | 70142 | 2.26 | 3.03 | 2.62 |
| 3 | NSAIDs only (over age of 80)8) | 738 | 2084 | 2822 | 2030 | 10169 | 12199 | 15021 | 1.74 | 2.14 | 1.93 |
| 2 | NSAIDs only10) | 625 | 21 | 646 | 2635 | 8794 | 11429 | 12075 | 3.7 | 5.1 | 4.3 |
| 1 | Integrated OR | 26793 | 197154 | 223947 | 1.5129 | 3.5853 | 2.5491 | ||||
Integrated ORs from each article’s data as results of observational studies of SSRI and NSAIDs exposure and association with UGIH. LL, lower limit; UL, upper limit; CI, confidence interval; OR, odds ratio.
| Case number | Combination use of SSRIs and NSAIDs | Neither SSRIs nor NSAIDs were administered | Total number of subjects | LL 95% CI | UL 95% CI | OR | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| UGIH | Controls | Total | UGIH | Controls | Total | ||||||
| 7 | SSRI and NSAIDs (all patients)8) | 92 | 11169 | 11261 | 168 | 52988 | 53156 | 64417 | 2.26 | 3.82 | 2.93 |
| 6 | SSRI and NSAIDs11) | 157 | 9034 | 9191 | 159 | 41621 | 41780 | 50971 | 3.3 | 5.31 | 4.19 |
| 5 | SSRI and NSAIDs9) | 23 | 1298 | 1321 | 44 | 9956 | 10000 | 11321 | 2.8 | 8.3 | 4.8 |
| 4 | SSRI and NSAIDs2) | 23 | 1529 | 1552 | 337 | 68253 | 68590 | 70142 | 2.01 | 5 | 3.17 |
| 3 | SSRI and NSAIDs (over age of 80)8) | 41 | 2781 | 2822 | 78 | 12121 | 12199 | 15021 | 1.76 | 3.94 | 2.64 |
| 2 | SSRI and NSAIDs10) | 99 | 547 | 646 | 183 | 11246 | 11429 | 12075 | 4.8 | 13 | 8 |
| 1 | Integrated OR | 26793 | 197154 | 223947 | 2.8923 | 5.1519 | 4.0221 | ||||
Integrated ORs from each article’s data as results of observational studies of SSRI and NSAIDs exposure and association with UGIH. LL, lower limit; UL, upper limit; CI, confidence interval; OR, odds ratio.
| At least NSAIDs or SSRIs were administered | Neither SSRIs nor NSAIDs were administered | Total number of subjects | LL 95% CI | UL 95% CI | OR | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| UGIH | Controls | Total | UGIH | Controls | Total | |||||
| SSRI only (all patients)8) | 253 | 11008 | 11261 | 522 | 52634 | 53156 | 64417 | 2.24 | 3.07 | 2.63 |
| NSAIDs only (all patients)8) | 1871 | 9390 | 11261 | 4700 | 48456 | 53156 | 64417 | 2.05 | 2.33 | 2.19 |
| SSRI and NSAIDs (all patients)8) | 92 | 11169 | 11261 | 168 | 52988 | 53156 | 64417 | 2.26 | 3.82 | 2.93 |
| SSRI only11) | 284 | 8907 | 9191 | 931 | 40849 | 41780 | 50971 | 1.13 | 1.5 | 1.3 |
| NSAIDs only11) | 1714 | 7477 | 9191 | 3089 | 38691 | 41780 | 50971 | 2.65 | 3.03 | 2.83 |
| SSRI and NSAIDs11) | 157 | 9034 | 9191 | 159 | 41621 | 41780 | 50971 | 3.3 | 5.31 | 4.19 |
| SSRI only9) | 22 | 1299 | 1321 | 105 | 9895 | 10000 | 11321 | 1.1 | 2.9 | 1.8 |
| NSAIDs only9) | 173 | 1148 | 1321 | 642 | 9358 | 10000 | 11321 | 2.3 | 3.5 | 2.8 |
| SSRI and NSAIDs9) | 23 | 1298 | 1321 | 44 | 9956 | 10000 | 11321 | 2.8 | 8.3 | 4.8 |
| SSRI only2) | 62 | 1490 | 1552 | 1881 | 66709 | 68590 | 70142 | 1.09 | 1.89 | 1.43 |
| NSAIDs only2) | 263 | 1289 | 1552 | 5266 | 63324 | 68590 | 70142 | 2.26 | 3.03 | 2.62 |
| SSRI and NSAIDs2) | 23 | 1529 | 1552 | 337 | 68253 | 68590 | 70142 | 2.01 | 5.00 | 3.17 |
| SSRI only (over age of 80)8) | 59 | 2763 | 2822 | 130 | 12069 | 12199 | 15021 | 1.66 | 3.2 | 2.31 |
| NSAIDs only (over age of 80)8) | 738 | 2084 | 2822 | 2030 | 10169 | 12199 | 15021 | 1.74 | 2.14 | 1.93 |
| SSRI and NSAIDs (over age of 80)8) | 41 | 2781 | 2822 | 78 | 12121 | 12199 | 15021 | 1.76 | 3.94 | 2.64 |
| SSRI only10) | 40 | 606 | 646 | 326 | 11103 | 11429 | 12075 | 1.01 | 2.8 | 1.7 |
| NSAIDs only10) | 625 | 21 | 646 | 2635 | 8794 | 11429 | 12075 | 3.7 | 5.1 | 4.3 |
| SSRI and NSAIDs10) | 99 | 547 | 646 | 183 | 11246 | 11429 | 12075 | 4.8 | 13 | 8.0 |
| Integrated OR | 26793 | 197154 | 223947 | 1.4456 | 3.5097 | 2.4777 | ||||
Integrated ORs from each article’s data as results of observational studies of SSRI and NSAIDs exposure and association with UGIH. LL, lower limit; UL, upper limit; CI, confidence interval; OR, odds ratio



The studies used for this analysis specified that patients who were taking different kinds of drugs, or who were in outlying age groups, were alcohol drinkers, or were smokers, had been excluded8,9,11) (Tables 3–6). Considering those facts, it is highly unlikely that the “SSRIs were NOT administered” group had taken NSAIDs, or that the “NSAIDs were NOT administered” group had taken SSRIs.
The risk analyses using integrated ORs revealed a risk of UGIH when using either SSRIs or NSAIDs alone; the UGIH risk when using NSAIDs alone was 1.47 times higher than that when using SSRIs alone. Combination use of the two kinds of drugs showed a 1.58- and 2.32-times higher risk of UGIH than did use of only NSAIDs or only SSRIs, respectively (Figs. 6–8).
Because some studies reported that SSRIs and NSAIDs increase the risk of UGIH, the risk analyses in this study were performed with regard to the combination use of these two kinds of drugs vs. use of each type of drug alone. However, the conclusions of past studies varied; some concluded that the risk was not increased with combination use,4,8,12,13) whereas others concluded that risk was increased1–3,9–11,14–17) compared to use of SSRIs or NSAIDs alone.
Four of the articles included in the present study2,3,9,10) reported a >2-times higher risk of UGIH with combination use vs. SSRIs alone, whereas none of the six articles reported the same risk increase for the use of NSAIDs alone. This suggests that the risk of UGIH with combination use of SSRIs and NSAIDs is higher than the additive effect of each type of drug alone (Fig. 6).
Moreover, the literature indicates that the upper gastrointestinal tract of SSRI users can be vulnerable because many of them are smokers.10) Alcohol use is also known to increase the risk of UGIH and should be considered an important confounding factor.10) These two factors would seem to support the increased risk of UGIH seen with the combination use of SSRIs and NSAIDs; however, even when all patients with alcoholism and cirrhosis were excluded,1) an increase in UGIH risk was still observed for combination use patients with no other complications.8)
Furthermore, the risk for UGIH is even higher in elderly patients and in those having some important confounding factor, because many of them are prescribed NSAIDs and SSRIs in order to prevent depression as well as recurrence of serious sequelae, including cerebral infarction.18)
Additional factors, such as Helicobacter pylori infection and use of NSAIDs, antiplatelet agents, and anticoagulants including aspirin and clopidogrel, all of which are common among elderly individuals, were reported to effect a higher risk of UGIH in elderly patients.2) Thus, elderly patients with depression have a high absolute risk of UGIH due to SSRI use. It was also reported that doctors generally prescribe both SSRIs and NSAIDs to these patients.3)
In contrast to the articles reporting on the risk of combination use in the elderly, one article reported that it is not necessary to force doctors to avoid combination use of antidepressants and NSAIDs,8) including in elderly patients. Another article reported that age did not influence the increase in risk seen with combination use.16) Thus, the effect of age on the risk of UGIH remains unclear. However, it is thought that greater attention to the combination use of such drugs in elderly people is warranted, since it is suggested that the risk of UGIH increases with age.
On the other hand, results of basic studies on the influence of these two kinds of drugs on gastric acid secretion, neutrophil infiltration and inflammatory cytokine levels or antiplatelet activity suggest these as the three greatest factors influencing gastric injury in animal models. A recent study confirmed that one of the SSRIs, paroxetine, was not involved in influencing systemic serotonin levels to inhibit gastric acid secretion in the rat, suggesting that the influence of SSRIs could affect, dose-dependently, gastric acid secretion via serotonin levels in the brain; however, the mechanisms involved remain unclear.19)
Moreover, despite the fact that prostaglandin E2 (PGE2) secretion, which produces gastric mucous and increases mucosal blood flow, is stimulated by serotonin, this study confirmed that paroxetine does not affect it, and suggested that reduction in the secretion of PGE2 is more likely to be caused by NSAID inhibition of cyclooxygenase 1 (COX1).19)
In addition, it was also reported that aspirin, one of the NSAIDs, induced production of inflammatory cytokines and increased neutrophil infiltration.19)
SSRIs are associated with a hemorrhagic tendency as a result of decreased platelet aggregation due to a lack of serotonin in the platelets. Additionally, it was also reported that SSRIs such as fluoxetine, paroxetine, and sertraline, which show much higher serotonin reuptake inhibition power,4) may increase hemostasis disorder and extension of the hemorrhagic time as a result of serotonin depletion for several weeks,3) and no UGIH tendencies were observed in the cases of patients administered noradrenergic and specific serotonergic antidepressants (NaSSas).18) On the other hand, NSAIDs act through a completely different mechanism to effect UGIH. NSAIDs inhibit the production of thromboxane A2 (TXA2), which is necessary for platelet aggregation, by inhibiting platelet COX1, whereas SSRIs deplete serotonin, which is necessary for platelet aggregation, by inhibiting the platelet serotonin transporter. One report stated that the degree of serotonin reuptake inhibition was not changed by the combination use of NSAIDs and SSRIs, in either case of low or high SSRI affinity to serotonin receptors.12) Moreover, another report stated that nonselective antidepressants did not increase the risk of UGIH in combination with NSAIDs.17)
On the other hand, in the case of NSAIDs, it was reported that there were no differences in the increase in UGIH risk with the combination use of SSRIs between non-selective COX inhibitors and the COX2 selective inhibitors.17)
In addition, NSAIDs inhibit production of prostaglandin I2 (PGI2), which inhibits platelet aggregation,19) but whether SSRIs affect this process is unclear. Hence, results of these studies suggest that the increase in risk with combination use of SSRIs and NSAIDs, which affect the three greatest risk factors for gastric injury, is additive.
Since this analysis was mainly of studies carried out in the United States and European countries, the results might be applicable only to Caucasians. However, because the mechanisms causing UGIH in other racial groups is thought to be same, this study’s results should provide a meaningful warning for all. There were no Asian studies that met our inclusion criteria and therefore none were selected for this analysis. This probably does not indicate that NSAIDs or SSRIs are less frequently prescribed compared with Western countries, but that there are few studies that were performed in Asia that comply with the STROBE statement. Thus, more pharmacoepidemiological studies are needed in Asian countries in order to confirm that concomitant use of these two kinds of drugs should be avoided to prevent UGIH.
Our meta-analysis shows that combination use of SSRIs and NSAIDs is associated with a greater increase in the risk of UGIH than the use of either type of drug alone.
Clinicians should be aware of the risk of UGIH in SSRI and NSAID users, and it is desirable to avoid combining these drugs. However, if the drugs are used simultaneously, the minimum dosage and treatment period should be prescribed.
Combination use of NSAIDs and SSRIs is frequent in elderly patients, despite the common presence of complicating disorders that can affect UGIH. Thus, clinicians should monitor this population carefully for UGIH onset during the treatment period.