2015 Volume 38 Issue 11 Pages 1827-1830
2015 Volume 38 Issue 11 Pages 1827-1830
Overuse of vitamin A as a dietary supplement is a concern in industrialized countries. High-level dietary vitamin A is thought to shift immunity to a T helper 2 (Th2)-dominant one, resulting in the promotion of allergies. We have been studying a fluorescein isothiocyanate (FITC)-induced contact hypersensitivity (CHS) mouse model that involves Th2-type immunity. We fed a diet with a high retinyl palmitate content (250 international units (IU)/g diet) or a control diet (4 IU/g diet) to BALB/c mice for three weeks. No augmentation of FITC-induced CHS was found in mice fed the diet with a high vitamin A content, although accumulation of the vitamin was confirmed in the livers of these animals. The results indicated that relatively short-term feeding of the high-level vitamin A diet did not influence the Th2-driven response at a stage with significant retinol accumulation in the liver. The results were in contrast to the high-dose pyridoxine diets that produced a reduced response in FITC-induced CHS.
Studies on mucosal immunity have revealed that vitamin A has a significant impact on the immune system.1) Retinal dehydrogenase produced by intestinal dendritic cells converts retinol into retinoic acid (RA). The imprinting in T cells by RA is believed to contribute to the maintenance of mucosal immunity in the intestine.1) Furthermore, vitamin A deficiency in pregnant mothers resulted in insufficient lymph node development in offspring in a mouse system.2) This could lead to weakening of adaptive immunity resulting in an inefficient outcome of vaccination in children.
For the above reasons, vitamin A supplementation in children has been implemented and has been shown to be beneficial.3) On the other hand, one of the most popular dietary supplements is vitamin A in developed countries. There is a growing concern about the overuse of preformed vitamin A.4)
High-level dietary vitamin A was reported to enhance the production of immunoglobulin E and the development of experimental asthma in a mouse study.5) Thus, the overuse of vitamin A supplements in industrialized countries may increase the risk or the severity of allergies involving T helper 2 (Th2)-type responses.
We have been studying a mouse contact hypersensitivity (CHS) model, in which fluorescein isothiocyanate (FITC) is used as an immunogenic hapten.6) This model has been shown to require Th2-type response.7,8) In this model, dibutyl phthalate (DBP) is applied together with FITC, and we have shown that DBP contributes to the sensitization process as an adjuvant.6,9)
We previously examined an effect of high-dose dietary vitamin B6 on the immune system. Vitamin B6 is another popular dietary supplement, like vitamin A. We demonstrated that relatively short-term (3 weeks) exposure to high-dose dietary vitamin B6 (pyridoxine) reduced FITC-induced CHS associated with a polarization to T helper 1 (Th1)-type immunity.10) In the present study, we examined whether a high dose of preformed vitamin A (all-trans retinyl palmitate) in diets affects FITC-induced CHS, using the same schedule of exposure to high-dose vitamin B6 we used previously. We also monitored the accumulation of retinol in the liver as to the general toxicity of preformed vitamin A. We did not find an effect of a high content of dietary vitamin A on FITC-induced CHS despite the significant accumulation of retinol in the liver.
Specific pathogen-free female BALB/c mice were purchased from Japan SLC Inc. (Shizuoka, Japan), and were used at 8 weeks of age, weighing 17.4±0.2 g (mean±standard error of the mean (S.E.M.)). They were housed at 22–24°C with 50–60% humidity under artificial lighting conditions with a 12-h light/dark cycle. Animal care and experiments were performed in accordance with the guidelines for the care and use of laboratory animals of the University of Shizuoka and those of Japan Ministry of Education, Culture, Sports, Science and Technology. The plans of animal studies were reviewed and approved (approval number: 136031) by the Institutional Animal Care and Use Committee of the University of Shizuoka.
DietsAs a standard-vitamin A diet, we used American Institute of Nutrition (AIN)-93G, which contains four international units (IU)/g of all-trans-retinyl palmitate as preformed vitamin A (4 IU-diet). An AIN-93G based diet with a high vitamin A content (250 IU/g) was also prepared (250 IU-diet). These diets were custom-ordered and purchased from Oriental Yeast Co. (Tokyo, Japan) as pellets of 12-mm diameter (Table 1). Feeding of these diets was started at 8 weeks of age and continued during the experiments.
| Ingredient | Standard | Excess |
|---|---|---|
| g/kg diet | ||
| Caseina) | 200 | 200 |
| L-Cystine | 3.0 | 3.0 |
| Corn starch | 397 | 397 |
| α-Corn starch | 132 | 132 |
| Sucrose | 100 | 100 |
| Soybean oil | 70.0 | 70.0 |
| Cellulose powder | 50.0 | 50.0 |
| Mineral mix (AIN-93G-MX) | 35.0 | 35.0 |
| Vitamin mix (AIN-93-VX) (vitamin A omitted) | 10.0 | 10.0 |
| Choline bitartrate | 2.5 | 2.5 |
| Butylhydroquinone, mg | 14.0 | 14.0 |
| Vitamin A,b) international units (IU)/kg | 4000 | 250000 |
a) Vitamin-free casein. b) All-trans-retinyl palmitate.
Acetone, DBP, FITC, all-trans-retinyl palmitate, pyrogallol, potassium hydroxide, hexane, anhydrous sodium sulfate, ethanol, methanol, sodium chloride and ethyl acetate were purchased from Wako Pure Chemical Industries, Ltd. (Osaka, Japan).
Contact Hypersensitivity (CHS) Mouse ModelContact sensitization to FITC was performed as earlier studies6) with modifications. After five days feeding of the synthetic diets (Table 1), mouse forelimbs were shaved. Two days later, the mice were anesthetized by intraperitoneal injection of pentobarbital, and then 160 µL of an FITC solution (0.5%, w/v) dissolved in a 1 : 1 (v/v) mixture of acetone and DBP (A/DBP) was epicutaneously applied to the shaved forelimbs (day 7). On day 14, the mice were sensitized again. On day 21, mice were challenged with FITC on the ear auricle after the baseline ear thickness (0 h) was measured using a dial thickness gauge (Mitutoyo; Kanagawa, Japan). Ear thickness was measured 24 and 48 h later, too. Ear swelling was defined as an increase in the ear thickness (ΔEar thickness) as compared with one before challenge as described previously.6)
Determination of the Retinol Content in the LiverForty-eight hours after challenge (on day 23), mouse liver tissue (50 mg specimen) was ground with a mortar and pestle in the presence of 100 mg of anhydrous sodium sulfate. The tissue homogenate was saponified for 30 min at 70°C in 1.3 mL of 77% ethanol containing 4.6% (w/v) potassium hydroxide (KOH), 2.3% (w/v) pyrogallol and 0.15% (w/v) sodium chloride (NaCl). After the addition of 2.25 mL of 1% NaCl, retinol was extracted into 1.5 mL of a 9 : 1 (v/v) mixture of ethyl acetate and hexane. The aqueous phase was extracted twice with ethyl acetate/hexane to ensure recovery, and then the organic phases were combined. After evaporation, the pooled organic phases were re-dissolved in ethanol, and then analyzed by reversed-phase HPLC (JASCO Co., Tokyo, Japan) on a column of Mightysil RP-18 Aqua (4.6 mm×150 mm; Kanto Chemicals, Tokyo, Japan) with an isocratic mobile phase of methanol–water (92 : 8). Retinol was detected at 325 nm with a UV detector (JASCO Co.), for which retinyl palmitate was used to generate a standard curve for vitamin A.
Statistical AnalysesFor two-group comparisons, Student’s t test was employed. When p<0.05, two groups were regarded as being significantly different. If the variance was significantly different between two groups by F test, Welch’s test was applied. For the analysis of body weight changes, two-way ANOVA was used.
Feeding of the synthetic diet containing a high level of vitamin A (250 IU-diet) or an adequate level of vitamin A (4 IU-diet) was started at 8 weeks of age (denoted as day 0). The body weights of the mice in each group increased similarly during the experiments from 8 to 11 weeks of age (Fig. 1). The average food intakes were 2.45 g/d and 2.41 g/d for the 4 IU-diet and 250 IU-diet groups, respectively.
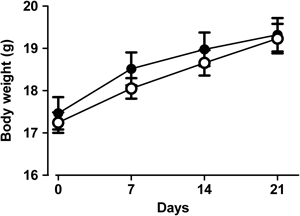
BALB/c mice were fed on a standard (4 IU/g) or an excess amount (250 IU/g) of vitamin A. Feeding of a synthetic diet was started at 8 weeks of age (day 0). Body weights were measured on days 0, 7, 14 and 21. The results are shown as the mean±S.E.M. for each group (filled circles, 4 IU-diet, n=7; open circles, 250 IU-diet, n=8). There is no significant difference (p>0.05) between two groups by two-way ANOVA.
We examined whether a relatively short-term intake of a high-level of dietary vitamin A influenced the response of FITC-induced CHS. Mice were fed on the 250 IU-diet or 4 IU-diet for 23 d. During this period, the mice were epicutaneously sensitized with FITC twice on days 7 and 14. On day 21, the mice were challenged with FITC on an ear auricle, and the increase in ear thickness was determined (Fig. 2). The ear-swelling response peaked at 24 h after challenge with an average response of around 110 µm. There was no difference in the ear-swelling response at 24 h between the groups on the 250 IU-diet and the 4 IU-diet. At 48 h after challenge, the ear-swelling response had decreased and no difference was seen between the two groups. Without epicutaneous sensitization with FITC, the average response at 24 h after challenge was 10 µm (data not shown). No mouse exhibited an ear-swelling response of more than 30 µm regardless of whether they were on the 4 IU- or 250 IU-diet.

BALB/c mice were fed on a synthetic diet containing either a standard (4 IU/g) or an excess amount (250 IU/g) of vitamin A for a total 23 d. After one-week feeding on one of the synthetic diets, mice were epicutaneously sensitized with FITC on days 7 and 14. On day 21, mice were challenged with FITC on an ear auricle, and the ear-swelling responses at 24 and 48 h were determined. The increase in the ear thickness (ΔEar thickness) of individual mice (ordinate) as compared with one before challenge (0 h) is plotted, and the mean for each group (4 IU-diet, n=7; 250 IU-diet, n=8) is shown by a horizontal bar. The means of the two groups are not significantly different (p>0.05).
The accumulation of vitamin A in the liver was examined. After measurement of the CHS response (day 23), the retinol content in the liver was measured. The retinol content was significantly higher in the group on the 250 IU-diet (Fig. 3). This suggests that the relatively short period on the diet with an excess amount of preformed vitamin A resulted in the accumulation of retinol in the liver.

After 23 d on a synthetic diet, the control 4 IU-diet or the excess vitamin A 250 IU-diet, retinol accumulation in mouse livers was measured by HPLC. The contents of retinol per wet weight of tissue of individual mice are plotted. The mean for each group (4 IU-diet, n=7; 250 IU-diet, n=8) is shown by a horizontal bar. Due to the different variance between two groups (p<0.05; F test), statistical significance was analyzed by means of Welch’s test.
We focused on whether or not excess intake of a preformed form of vitamin A for a short period of time, which may reflect temporary use of a dietary supplement, could cause an increased sensitization in the FITC-induced CHS. Although we did not directly measure Th2-polarization in the preset studies, the Th2-type immune response has been shown to be required for the FITC-induced CHS.7,8) Thus, the FITC-induced CHS will provide a parameter that could evaluate potential risk of allergies involving Th2-type responses.
The diet with a high vitamin A content was set as the 250 IU/g diet (250 IU-diet), while the control diet was set as the 4 IU/g diet (4 IU-diet) considering the recommended vitamin A intake for mice, as reported in earlier studies.5,11) Body weight gain did not differ between the groups of mice on the high vitamin A and the control diet. However, significantly increased accumulation of retinol in the liver was observed after 23 d with the 250-IU diet. Nevertheless, FITC-induced CHS that requires Th2 responses did not differ between the mice on the different diets. The results suggested that the effect of excess vitamin A intake on the immune system might not become obvious at the stage when abnormal accumulation of retinol in the liver is already apparent. It is an interesting issue whether or not Th2-polarization is detectable with a short period excessive vitamin A intake. Further studies are needed to address this question.
It is still possible that the intake of excess vitamin A for an extended period could influence helper T cell polarization. For example, a total 8 weeks exposure to the 250 IU-diet resulted in decreased interferon (IFN)-γ but increased interleukin (IL)-10 production in a mouse influenza virus infection model.11) Another study examined the effect of the 250 IU-diet and a vitamin A-deficient diet for a total 12 weeks starting from birth (diet for lactating mothers). The results indicated that the excessive vitamin A intake increased but the vitamin A-deficient diet decreased the disease severity of asthma in a mouse model.5)
As to other adverse effects of high-level dietary vitamin A, liver function is a concern. In a rat experiment, daily oral administration of 10000 IU/kg body weight of vitamin A for 6 weeks caused elevation of alanine aminotransferase and aspartate aminotransferase activities.12) Although we did not measure these markers in the present experiment, measurement of food consumption suggested 32500 IU/kg body per day in our 250 IU-diet group. Accumulation of retinol in the liver might coincide with the effects on the liver function.
Our previous studies demonstrated that the feeding of a diet with a 20-fold excess of vitamin B6 (pyridoxine) for 23 d resulted in a reduction of FITC-induced CHS10) in BALB/c mice. Although the same experimental schedule was applied for the high-level vitamin A diet (62.5-fold excess), no significant effect on FITC-induced CHS was observed. As to high-level dietary vitamin A, accumulation of retinol in the liver may have a more direct and immediate impact on health than the effect on the immune system might do.
This work was supported partly by a Grant-in-Aid for Scientific Research (B) (Grant No. 23390031) and Grant-in-Aid for Challenging Exploratory Research (Grant No. 15K14990) of the Japan Society for the Promotion of Science. We thank Mr. NJ Halewood for providing an English editing service as a native English speaker.
The authors declare no conflict of interest.