Abstract
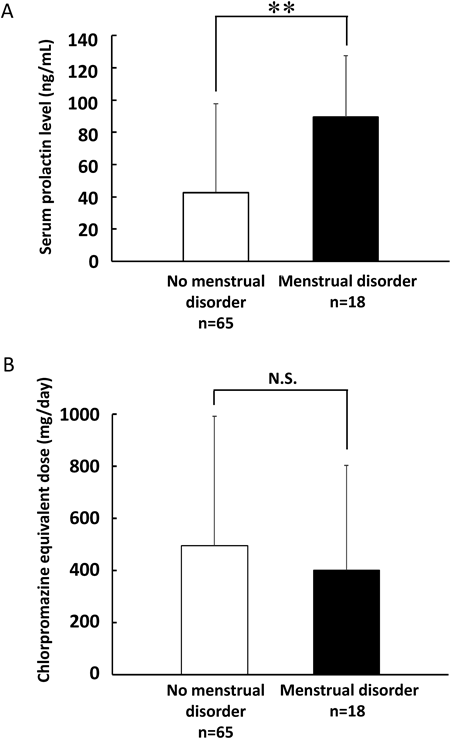
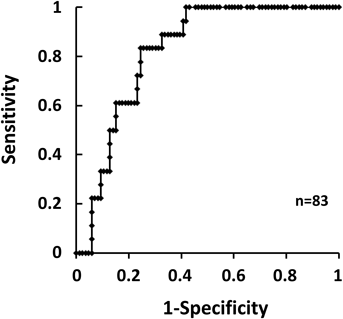
Treatment with antipsychotic drugs has been associated with hyperprolactinemia. The same antipsychotic drugs have also been associated with side effects such as menstruation disorders. The aim of this study was to evaluate the prevalence of hyperprolactinemia and menstruation disorders in women undergoing antipsychotic treatment. We performed a retrospective chart review study of psychiatric patients who underwent laboratory testing for serum prolactin (PRL) level between March 2011 and March 2015 in Ehime University Hospital. Patients presenting with and without menstruation disorders were evaluated to determine if they presented concomitant hyperprolactinemia. Patients with menstrual disorders had a significant increase in serum PRL level with a mean of approximately 90 ng/mL. Those with menstrual disorders presented increased PRL levels by 2-fold that of patients without menstrual disorder. However, there was no significant difference in the equivalent dose of chlorpromazine between these two groups. Additionally, about 70% of patients with menstrual disorders received risperidone treatment. The receiver operating characteristic curve showed that the optimal cutoff point of serum PRL level associated with the development of menstrual disorders was 60 ng/mL. Based on these results, we concluded that patients with menstrual disorders presented increased serum PRL, and that most of them underwent treatment with risperidone.
Atypical antipsychotics are recommended as first-line treatments for individuals with schizophrenia. These drugs not only improve symptoms, such as auditory or visual hallucinations, but compared with typical antipsychotics, they are associated with fewer side effects, such as sleepiness, weight gain, and tremors.1) However, antipsychotic drugs are also known to influence the hypothalamo-hypophyseal axis and induce variable degrees of hyperprolactinemia.2,3) Hyperprolactinemia is a recognized adverse side effect of antipsychotic drugs. It can be acute or chronic, and it can be associated with sexual dysfunction, menstrual irregularities, amenorrhea, galactorrhea and osteoporosis.4) The proportion of premenopausal women who develop hyperprolactinemia during treatment with antipsychotic drugs can be as high as 48 to 93%.5) Despite such high prevalence, in most cases, hyperprolactinemia is asymptomatic. However, some patients present clinical symptoms along with severe disease.6) Additionally, the condition and its management strategies are scarcely mentioned in psychiatric nursing journals or textbooks.7) Therefore, hyperprolactinemia induced by antipsychotic drugs may be less successfully managed. This could be potentially harmful to patients and affect their QOL.6,8) In clinical practice, serum prolactin (PRL) levels are helpful in the early detection of adverse side effects induced by antipsychotic drugs. Hyperprolactinemia is the presence of abnormally high levels of PRL in serum. Normal PRL levels are less than 25 ng/mL for women and less than 20 ng/mL for men.9) However, if patients receiving antipsychotic therapy develop hyperprolactinemia (>25 ng/mL), it is very difficult to discontinue medication at once, because of therapeutic efficacy. It remains unclear what cutoff level of PRL concentration causes menstrual disorders. Therefore, the relationship between serum PRL and adverse side effects, such as menstrual irregularities, needs further investigation.
The purpose of this study was to evaluate the prevalence of hyperprolactinemia in women with psychiatric disorders receiving antipsychotic treatment.
PATIENTS AND METHODS
Ethical Approval of the Study ProtocolThis study was conducted in accordance with the guidelines for the care of human study participants adopted by the Ethics Committee of Ehime University Hospital (approval number: 1602009), the Ethical Guidelines for Medical and Health Research Involving Human Subjects, and the principles of the Helsinki Declaration.
Research Data and Patient CharacteristicsThis retrospective study was carried out at Ehime University Hospital using data from electronic medical records dated between March 2011 and March 2015. We excluded the medical records of pregnant women, nursing women, as well as women with hypothyroidism or hypophyseal adenoma. Patients who underwent serum PRL monitoring after administration of psychiatric drugs were enrolled in this study. Patient characteristics (age [under 55 years], sex [only women]) and necessary research data (serum PRL and prescription history) were collected from the medical records of 83 patients with psychiatric disorders (Table 1). The antipsychotic drugs prescribed in this study were chlorpromazine, haloperidol, levomepromazine, risperidone, paliperidone, quetiapine, olanzapine, blonanserin, aripiprazole and clozapine. We used the equation described by Woods10) to calculate the equivalent dose of chlorpromazine for the dose of the other psychiatric drugs. The antipsychotic drug dosages used were then compared by chlorpromazine equivalent dosages.
Table 1. Background of Patients with and without Menstrual Disorders
| No menstrual disorder | Menstrual disorder |
|---|
| N | 65 | 18 |
| Age | 37 [15–44] | 32 [15–44]a) |
| Combination use (%) | 8 (12) | 4 (22) |
| Chlorpromazine equivalent dose (mg/d) | 495.8±419.7 | 401.6±387.6 |
Rate of prescribed atypical antipsychotic following patients with menstrual disorder versus with no menstrual disorder: a) p<0.05. Combination use show the number of patients with over two drugs induced by hyperprolactinemia such as chlorpromazine, haloperidol, levomepromazine, risperidone, paliperidone, quetiapine, olanzapine, blonanserin, aripiprazole and clozapine.
The data are shown as means and standard deviation. The statistical significance of the differences resulting from comparisons of patients with or without menstrual disorders was evaluated using the Mann–Whitney U test or Fisher’s exact test after checking for normal distribution using the Kolmogorov–Smirnov test. Receiver operating characteristic (ROC) curves were calculated, and the area under the curve (AUC) was calculated to evaluate the optimal cutoff point of serum PRL level to induce menstrual disorders. The optimal cutoff value was calculated using the following formula: (1−sensitivity)2+(1−specificity)2 with the ROC curve. A value of p<0.05 was considered significant. Statistical analyses were performed using Ekuseru-Toukei 2012 (Social Survey Research Information Co., Ltd., Tokyo, Japan).
RESULTS
Relation of Serum PRL and Menstrual DisordersThe changes in serum PRL level in the antipsychotic drug treatment group were compared between patients with or without menstrual disorders (Fig. 1). A total of 83 women were included in this study. Patients with and without menstrual disorder had a mean age (range) of 32 (15–44) and 37 (15–44) years, respectively. The mean age of women with menstrual disorder was significantly less than that of patients without menstrual disorders (p<0.05). The mean PRL serum level was significantly higher in patients with menstrual disorders compared with those without menstrual disorder (89.3±36.9 vs. 42.5±54.5; 95% confidence interval (CI): 46.8 [19.3–74.3], p<0.001) (Fig. 1A). However, patients with menstrual disorder showed no significant difference in chlorpromazine equivalent dose (mg/d) compared with patients without menstrual disorder (401.6±387.6 vs. 495.8±419.7; 95% CI: 94.2 [−124.7–313.2], p=0.36) (Fig. 1B).
Next, we focused on the rate of prescribed atypical antipsychotic drugs in patients receiving antipsychotic drugs to identify a relationship between menstrual disorder and type of drug. The proportion of atypical psychotic drugs used is shown in Table 2. The proportion of patients with menstrual disorders that received risperidone treatment was significantly higher than that in those without menstrual disorders, while the proportion of patients without menstrual disorders that received aripiprazole treatment was higher than that of patients with menstrual disorders.
Table 2. The Proportion of Prescribed Atypical Antipsychotics between Patients with and without Menstrual Disorders
| No menstrual disorder (n=65) | Menstrual disorder (n=18) |
|---|
| Aripiprazole (%) | 16 (25) | 0 (0)a) |
| Risperidone (%) | 15 (23) | 12 (67)b) |
| Olanzapine (%) | 19 (29) | 4 (22) |
| Quetiapine (%) | 11 (17) | 5 (28) |
Rate of prescribed atypical antipsychotic following patients with menstrual disorder versus with no menstrual disorder: a) p<0.05; b) p<0.01.
Finally, using the ROC curve, we examined the relation between hyperprolactinemia and adverse side effects, such as menstrual disorders (Fig. 2). In the ROC curve, the AUC for serum PRL level was 0.82. The optimal cutoff point of serum PRL level for the detection of antipsychotic-induced hyperprolactinemia was found to be 60 ng/mL.
DISCUSSION
The present study results showed that serum PRL level in women with psychiatric disorders without menstrual disorders was about 40 ng/mL. The normal range of serum PRL level is between 10 and 20 ng/mL in men and 10 and 25 ng/mL in women.11) This result suggests that in clinical practice, the therapeutic effect of antipsychotic drugs is prioritized over the risks associated with the use of these drugs. The group with menstrual disorders showed a significantly higher PRL serum value compared with the group without menstrual disorders. We found that the mean age of patients with menstrual disorders was significantly less than that of patients without menstrual disorder. However, in a previous study, there was no significant correlation between age and PRL values in 54 patients with menstrual disorders, such as uterine bleeding.12) Additionally, the dose of medication that was calculated based on the chlorpromazine dose was not significantly different in either group (with or without menstrual disorders), and the patients receiving risperidone had menstrual disorders. In a previous study, abnormal menstrual cycles were reported in 88% of women treated with risperidone compared with 48% of women taking first-generation antipsychotics.5) Additionally, antipsychotic-induced hyperprolactinemia is related to differential dopamine D2 receptor affinity, 5-hydroxytryptamine (5-HT) receptor affinity, and blood–brain disposition of antipsychotics.13) The introduction of atypical antipsychotics represented a major advance in clinical therapy, and it was associated with lower adverse side effects compared with typical antipsychotics. However, risperidone has a strong D2-blocking effect and a simultaneous effect on the 5-HT2 receptors.14) Thus, patients with hyperprolactinemia were more likely to receive risperidone in our study. In contrast, Zhao et al. reported that adjunctive aripiprazole treatment in patients with schizophrenia who develop risperidone-induced hyperprolactinemia results in a significant reduction of serum PRL level.15) In a previous study, it was reported that at week 52, the median PRL had increased by 177% in the haloperidol group and decreased by 40% in the aripiprazole group.16) Interestingly, our results showed that the proportion of patients without menstrual disorders that received aripiprazole treatment was significantly higher than that of patients with menstrual disorders. Thus, our results seem to be consistent with those of previous research. These findings indicate that the increase in PRL induced by antipsychotics can be attributable to the drug type rather than the dose of antipsychotics. Bostwick et al. reported that if the effects of PRL are evident, the drug can be changed to another agent that is less likely to affect PRL levels.17)
Further research is needed to clarify the appropriate method for PRL monitoring. In the present study, using ROC curve analysis, we estimated that the cutoff value of PRL that can lead to adverse side effects induced by antipsychotic drugs, such as menstrual disorders, was 60 ng/mL. Additionally, the AUC (0.82) of the ROC curve had an acceptable accuracy.
The limitations of this study and details that we should consider in the future are as follows. This was a single-center study with a relatively small sample size. This study was retrospective in nature and we did not include a control group. Additionally, the previous treatments received by the patients were various and heterogeneous. Therefore, a large-scale prospective cohort validation study, including other factors associated with hyperprolactinemia is necessary. Future large-scale prospective validation studies may determine whether the cutoff value of 60 ng/mL in serum PRL may be a useful indicator of menstrual disorders induced by antipsychotic treatment. Although further studies are required to clarify the involvement of hyperprolactinemia in the adverse effects induced by psychiatric treatment, our findings indicate that clinicians should monitor PRL in these patients based on the cutoff value of 60 ng/mL to improve early detection of adverse effects such as menstrual disorders.
Conflict of Interest
The authors declare no conflict of interest.
REFERENCES
- 1) Khanna P, Suo T, Komossa K, Ma H, Rummel-Kluge C, El-Sayeh HG, Leucht S, Xia J. Aripiprazole versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst. Rev., 2014, Cd006569 (2014).
- 2) Howes OD, Wheeler MJ, Pilowsky LS, Landau S, Murray RM, Smith S. Sexual function and gonadal hormones in patients taking antipsychotic treatment for schizophrenia or schizoaffective disorder. J. Clin. Psychiatry, 68, 361–367 (2007).
- 3) Konarzewska B, Wolczynski S, Szulc A, Galinska B, Poplawska R, Waszkiewicz N. Effect of risperidone and olanzapine on reproductive hormones, psychopathology and sexual functioning in male patients with schizophrenia. Psychoneuroendocrinology, 34, 129–139 (2009).
- 4) Holt RI, Peveler RC. Antipsychotics and hyperprolactinaemia: mechanisms, consequences and management. Clin. Endocrinol. (Oxf.), 74, 141–147 (2011).
- 5) Kinon BJ, Gilmore JA, Liu H, Halbreich UM. Prevalence of hyperprolactinemia in schizophrenic patients treated with conventional antipsychotic medications or risperidone. Psychoneuroendocrinology, 28 (Suppl. 2), 55–68 (2003).
- 6) Johnsen E, Kroken RA, Abaza M, Olberg H, Jorgensen HA. Antipsychotic-induced hyperprolactinemia: a cross-sectional survey. J. Clin. Psychopharmacol., 28, 686–690 (2008).
- 7) Wong-Anuchit C. Clinical management of antipsychotic-induced hyperprolactinemia. Perspect. Psychiatr. Care, 52, 145–152 (2016).
- 8) Lu ML, Shen WW, Chen CH. Time course of the changes in antipsychotic-induced hyperprolactinemia following the switch to aripiprazole. Prog. Neuropsychopharmacol. Biol. Psychiatry, 32, 1978–1981 (2008).
- 9) Halbreich U, Kinon BJ, Gilmore JA, Kahn LS. Elevated prolactin levels in patients with schizophrenia: mechanisms and related adverse effects. Psychoneuroendocrinology, 28 (Suppl. 1), 53–67 (2003).
- 10) Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J. Clin. Psychiatry, 64, 663–667 (2003).
- 11) Peuskens J, Pani L, Detraux J, De Hert M. The effects of novel and newly approved antipsychotics on serum prolactin levels: a comprehensive review. CNS Drugs, 28, 421–453 (2014).
- 12) Ratchev E, Dokumov S. Premenopausal bleeding associated with hyperprolactinaemia. Maturitas, 21, 197–200 (1995).
- 13) Fitzgerald P, Dinan TG. Prolactin and dopamine: what is the connection? A review article. J. Psychopharmacol., 22 (Suppl.), 12–19 (2008).
- 14) Just MJ. The influence of atypical antipsychotic drugs on sexual function. Neuropsychiatr. Dis. Treat., 11, 1655–1661 (2015).
- 15) Zhao J, Song X, Ai X, Gu X, Huang G, Li X, Pang L, Ding M, Ding S, Lv L. Adjunctive Aripiprazole Treatment for Risperidone-Induced Hyperprolactinemia: An 8-week randomized, open-label, comparative clinical trial. PLOS ONE, 10, e0139717 (2015).
- 16) Argo TR, Carnahan RM, Perry PJ. Aripiprazole, a novel atypical antipsychotic drug. Pharmacotherapy, 24, 212–228 (2004).
- 17) Bostwick JR, Guthrie SK, Ellingrod VL. Antipsychotic-induced hyperprolactinemia. Pharmacotherapy, 29, 64–73 (2009).