2020 Volume 43 Issue 11 Pages 1634-1642
2020 Volume 43 Issue 11 Pages 1634-1642
Hepatic fibrosis (HF) is a common disease, with currently no available treatment. Galangin, a natural flavonoid extracted from Alpinia officinaruim Hance, has multiple effects demonstrated in previous studies. The aim of the present study was to explore the anti-fibrogenic effect of galangin in vitro, and research its potential molecular mechanisms. LX-2 cells were chosen as an in vitro HF model, and were treated with galangin in different concentrations. Cell viability was analyzed using Cell Counting Kit-8 (CCK-8) and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay, cell apoptosis was measured using flow cytometry, and the anti-fibrogenic effect of galangin was determined using RT-quantitative (q)PCR, immunofluorescence, and Western blotting. The results show that the proliferation of LX-2 cells was efficiently inhibited by galangin, and apoptosis was induced in a dose-dependent manner. Both the mRNA and protein expression of alpha-smooth muscle actin (α-SMA) and collagen I were markedly downregulated. Galangin also inhibited the phosphatidylinositol 3-kinase (PI3K)/Akt and Wnt/β-catenin signaling pathways and increased the Bax/Bcl-2 ratio. The results of this study suggest that galangin has an anti-fibrogenic effect and may represent a promising agent in the treatment of hepatic fibrosis.
Hepatic fibrosis (HF) represents a response to an acute or chronic liver damage1) that can be caused by various factors such as hepatitis B and C virus infections,2) drug-induced hepatitis, alcoholic hepatitis and non-alcoholic hepatitis. HF is a critical stage in the development of liver cirrhosis and liver cancer.3) The central process of HF is represented by the activation of hepatic stellate cells (HSCs),4) leading to the excessive accumulation of proteins such as collagen I and α-smooth muscle actin (α-SMA) in the extracellular matrix (ECM).5) Under the influence of pro-fibrotic adipocytokines, quiescent HSCs are activated and gradually transformed into myofibroblasts, leading to a metabolic imbalance and a large amount of ECM. As a result, ECM accumulation in the liver can accelerate and aggravate the pathophysiological process of HF. Therefore, inhibiting the activation and proliferation of HSCs and inducing their apoptosis can be an effective anti-fibrogenic therapeutic solution.6)
Phosphatidylinositol 3-kinase (PI3K) is an intracellular kinase that responds to a wide range of signals, resulting in the activation of phosphoinositide-dependent kinases through the phosphorylation of threonine 308 (Thr308) and serine 473 (Ser473) residues. Serine/threonine protein kinase B (PKB), also known as Akt, is one of the downstream molecules in the PI3K signaling pathway. The PI3K/Akt pathway regulates a large number of cell processes such as proliferation, apoptosis, translation, and differentiation.7–9) Furthermore, the PI3K/Akt signaling pathway is involved in a variety of diseases, including cancers,10) cardiovascular diseases,11) and diabetes,12) but also in the regulation of HSCs proliferation, differentiation, and apoptosis in HF.13) Thus, the pathway may regulate the activity of numerous downstream proteins, such as members of the Bcl-2 family, that interfere with apoptosis.7) The PI3K/Akt pathway is also related to the Wnt/β-catenin pathway by regulating the phosphorylation level of glycogen synthase kinase-3β (GSK-3β) inside the cell.
Alpinia officinaruim Hance (Fig. 1), a plant in the ginger family, has been widely used as a food flavor, fragrance, and traditional medicine in South Asian countries for centuries.14–16) Galangin or 3,5,7-trihydroxyflavone, a naturally active flavonoid, is a polyphenolic compound extracted from the rhizome of Alpinia officinarum Hance. It has been reported that galangin has anti-oxidant,17) anti-inflammatory,18) anti-allergic,19) anti-Alzheimer’s disease (AD),20) and anti-tumor21,22) effects. Studies suggest that galangin is able to regulate the AMP activated protein kinase (AMPK) pathway, the nuclear factor-kappaB (NF-κB) pathway, and the Bax/Bcl-2 ratio in different cells,23,24) having a lower cytotoxicity on normal cells.25–27) Early studies have shown that galangin has a protective effect on alcoholic liver injury, can downregulate the level of alanine aminotransferase (ALT) and aspartate aminotransferase (AST), and is able to reverse liver damage in an animal model28) by reducing the level of oxidative stress and lipid peroxidation in hepatic cells.29,30) Galangin has also shown anti-fibrogenic activity in rats,31) but the relevant molecular mechanism has not been identified yet. Further studies are needed regarding the involvement of galangin in HF through the PI3K/Akt pathway or its downstream pathways.
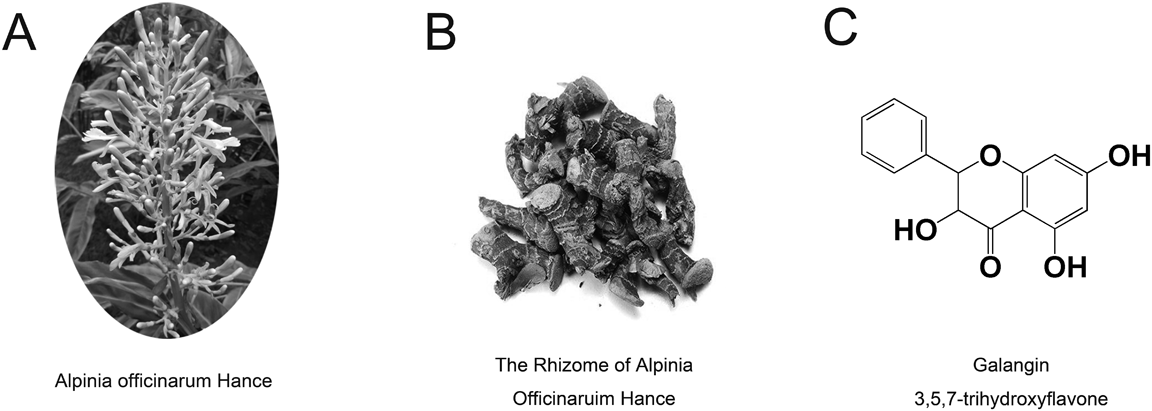
(A) Alpinia officinarum Hance, a plant of the Zingiberaceae family; (B) Galangal, the rhizome of Alpinia officinarum Hance, a traditional medicine in China and South Asian countries for centuries; (C) The chemical structure of galangin, 3,5,7-trihydroxyflavone, extracted from the rhizome of Alpinia officinarum Hance.
In this study, we aim to assess the anti-fibrogenic effect of galangin on LX-2 cells, a human HSC line, exploring its influence on the PI3K/Akt and downstream pathways and its potential to be used as a new anti-fibrogenic therapy.
Galangin (batch no.: K1706037) was purchased from Aladdin Pharmaceutical (Shanghai, China). Dimethyl sulfoxide (DMSO), Triton X-100, paraformaldehyde, the Akt inhibitor (MK-2206), and transforming growth factor-β1 (TGF-β1) were purchased from Servicebio (Wuhan, China). Cell Counting Kit-8 (CCK-8) and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) testing kits were purchased from BioSharp (Wuhan, China), and PE-Annexin V/7-AAD kits were purchased from BD Biosciences (Franklin Lakes, NJ, U.S.A.). TRIzol Reagent was purchased from Invitrogen/Thermo Fisher Scientific (Carlsbad, CA, U.S.A.), and PrimeScript RT reagent kits were purchased from TaKaRa (Tokyo, Japan). EnTurbo SYBR Green PCR SuperMix was purchased from Elk Biotechnology (Wuhan, China). BCA protein assay kits were purchased from Pierce/Thermo Fisher Scientific (Waltham, MA, U.S.A.). Primary antibodies against PI3K (#3285), p-PI3K (#3283), Akt (#4691), p-Akt (#4060), GSK-3β (#9315), p-GSK-3β (#9336), β-catenin (#9562), active β-catenin (#8814), Bax (#2772), Bcl-2 (#3498), and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (#2118), as well as Anti-Rabbit Secondary Antibody immunoglobulin G (IgG) H + L (#5151) and Goat Anti-Rabbit IgG/Cy3 (#1032) were purchased from Cell Signaling Technology Inc. (Danvers, MA, U.S.A.).
Cell CultureLX-2 cells were purchased from Beijing North Carolina Souren Biotechnology Research Institute (BNCC341818; Beijing, China). The cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) (HyClone/GE Healthcare, Logan, UT, U.S.A.) supplemented with 10% (v : v) fetal bovine serum (Gibco/Thermo Fisher Scientific) and 1% solution of antibiotics (100 U/mL penicillin and 100 µg/mL streptomycin) at 37 °C in a humidified incubator with a chamber atmosphere of 5% CO2.
Cell Viability AssayCell viability of LX-2 cells was examined using CCK-8 and MTT assay. LX-2 cells were seeded into 96-well plates at a density of 1 × 104 cells per well in DMEM supplemented with 10% fetal bovine serum (FBS) and incubated overnight. The medium was replaced with fresh DMEM containing different concentrations of galangin (0, 6, 8, 10 µg/mL) with and without TGF-β1 (5 ng/mL). After 12 or 24 h, the CCK-8 and MTT assays were performed. In brief, CCK-8 and DMEM (1 : 10, v:v) were added to each well (100 µL/well), and the plates were cultured at 37 °C for another 1 h. Then, the plates were measured using a microplate reader at 450 nm (optical density [OD] 450) (MR7000, Dynatech, Edgewood, NY, U.S.A.). Cell viability in CCK-8 was calculated using the following formula: CV = (OD450,test/OD450,control) × 100%. MTT (5 mg/mL) was added to each well (10 µL/well), cultured at 37 °C for another 4 h, then replaced with DMSO (100 µL/well), and measured using a microplate reader at 570 nm (OD 570) (MR7000, Dynatech, Edgewood, NY, U.S.A.). Cell viability in MTT was calculated using the following formula: CV = (OD570,test/OD570,control) × 100%.
Flow CytometryLX-2 cells were seeded into 6-well plates at a density of 2 × 105 cells per well in DMEM supplemented with 10% FBS overnight. The medium was replaced with fresh DMEM containing galangin (0, 6, 8, and 10 µg/mL) with and without TGF-β1 (5 ng/mL) for another 24 h. Then, all the cells were collected, washed twice in cold phosphate buffered saline (PBS), centrifuged, and assessed for apoptosis with PE-Annexin V/7-AAD kits, using flow cytometry at a wavelength of 488 nm (BD Biosciences, San Jose, CA, U.S.A.). Positivity for PE-Annexin V and negativity for 7-AAD was considered early apoptosis, while positivity for both was considered late apoptosis.
ImmunofluorescenceLX-2 cells were seeded into 6-well plates at a density of 2 × 105 cells per well in DMEM supplemented with 10% FBS overnight. The medium was replaced with fresh DMEM containing galangin (0, 6, 8, and 10 µg/mL) with and without TGF-β1 (5 ng/mL) for another 24 h. Then, the cells were washed in PBS three times, fixed in 4% paraformaldehyde, and permeabilized with 5% Triton X-100. The cells were incubated overnight at 4 °C with primary antibodies against collagen I (ratio: 1 : 100) and α-SMA (ratio: 1 : 100). After being washed in TBST three times, the samples were incubated for 1 h with Anti-Rabbit Secondary Antibody IgG/Cy3 (ratio: 1 : 100). The nuclei were stained with 4′-6-diamidino-2-phenylindole (DAPI) for 5 min and washed in TBST three times. Immunofluorescence signals were captured with a fluorescence microscope (Olympus BX53, Japan) and analyzed with ImageJ software.
RT-qPCRLX-2 cells were seeded into 6-well plates at a density of 2 × 105 cells per well in DMEM supplemented with 10% FBS overnight. The medium was replaced with fresh DMEM containing galangin (0, 6, 8, and 10 µg/mL) with and without TGF-β1 (5 ng/mL) for another 24 h. The total RNA was isolated using TRIzol reagent, and cDNA was synthesized using the PrimeScript RT reagent kit according to the manufacturer’s protocol. RT-qPCR was performed using EnTurbo SYBR Green PCR SuperMix and a real-time PCR system (Applied Biosystems 7500; Applied Biosystems/Thermo Fisher Scientific). Each cycle involved denaturing at 95 °C for 5 s, annealing at 60 °C for 40 s for 40 cycles, followed by melting at 95 °C for 40 s and cooling to 60 °C in 1 min. The levels of protein mRNA were normalized to the levels of GAPDH mRNA. The 2−ΔΔCq method was adopted to calculate the relative expression of mRNA.32) The primer sequences were as follows: α-SMA, forward 5′-ACG AGA CCA CCT ACA ACA GCA T-3′; reverse 5′-CTC GTC GTA CTC CTG CTT GGT-3′; collagen I, forward 5′-ACT GGT GAG ACC TGC GTG TA-3′; reverse 5′-AAT CCA TCG GTC ATG CTC TC-3′; GAPDH, forward 5′-ATG ACA TCA AGA AGG TGG TG-3′; reverse 5′-CAT ACC AGG AAA TGA GCT TG-3′.
Western BlottingLX-2 cells were seeded into 6-well plates at a density of 2 × 105 cells per well in DMEM supplemented with 10% FBS overnight. The cells were treated with TGF-β1 (5 ng/mL) alone, MK-2206 (6 µmol/L) with TGF-β1 (5 ng/mL), galangin (0, 6, 8, and 10 µg/mL) with TGF-β1 (5 ng/mL) for 24 h. The cells were collected, lysed at 4 °C for 30 min in RIPA buffer containing protease inhibitor cocktail, phenylmethanesulfonyl fluoride, and phosphorylated protease inhibitors A and B. The protein concentration was normalized with the BCA protein assay kit before Western blot. Proteins were separated on 8 to 15% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto polyvinylidene difluoride (PVDF) membranes. The membranes were blocked with 5% bovine serum albumin at room temperature for 2 h, washed in TBST three times, and incubated overnight at 4 °C with primary antibodies against α-SMA (ratio: 1 : 2000), collagen I (ratio: 1 : 500), PI3K (ratio: 1 : 1000), p-PI3K (ratio: 1 : 1000), Akt (ratio: 1 : 1000), p-Akt (ratio: 1 : 2000), GSK-3β (ratio: 1 : 1000), p-GSK-3β (ratio: 1 : 1000), β-catenin (ratio: 1 : 5000), active β-catenin (ratio: 1 : 5000), Bax (ratio: 1 : 2000), Bcl-2 (ratio: 1 : 1000), or GAPDH (ratio: 1 : 1000). After being washed in TBST and incubated for 2 h with Anti-Rabbit Secondary Antibody IgG H + L (ratio: 1 : 15000), the cells were scanned with an Odyssey system (LI-COR Biosciences, Lincoln, NE, U.S.A.). Protein levels were normalized to the levels of GAPDH.
Statistical AnalysisAll values are presented as mean ± standard error of mean (S.E.M.), and all experiments were repeated at least three times. The data was analyzed with Student’s t-test and one-way ANOVA using GraphPad Prism version 6 (GraphPad Software, La Jolla, CA, U.S.A.). A value of p < 0.05 was considered to indicate statistically significant differences.
Figure 2 shows the effect of galangin on the viability of LX-2 cells with and without TGF-β1. Both the CCK-8 and MTT assays have shown that galangin inhibited cell proliferation in a time-dose-dependent manner in both groups. The inhibition became significant after 24 h (p < 0.05). Furthermore, galangin exhibited a lower cellular toxicity at concentrations between 6–10 µg/mL in normal LX-2 cells, as there was no significant difference between the low- and medium-dose galangin in the 12 and 24 h groups, while the inhibitory rate of high-dose galangin was significant lower than in TGF-β1-activated LX-2 cells. To simulate the pathophysiological process of HF accurately with LX-2 cells in vitro, we decided to use TGF-β1 with concentrations of 6, 8, and 10 µg/mL of galangin in subsequent examinations.

(A) Relative cell viability of LX-2 cells under the galangin treatment with TGF-β1-activated for 12 and 24 h, measured with the CCK-8 assay; (B) Relative cell viability of LX-2 cells under the galangin treatment without TGF-β1-activated, used the CCK-8 assay; (C) Relative cell viability of LX-2 cells under the galangin treatment with TGF-β1-activated, detected with the MTT assay; (D) Relative cell viability of LX-2 cells under the galangin treatment without TGF-β1-activated by MTT assay. Each column shows the mean ± S.E.M. (n = 6 for each group). * p < 0.05, ** p < 0.01, *** p < 0.001 vs. the control group; # p < 0.05, ## p < 0.01, ### p < 0.001 vs. the TGF-β1 group.
As it can be seen in Fig. 3, there was a significant dose-dependent increase in the ratio of apoptosis (both early and late apoptosis) in LX-2 cells under treatment with galangin. Furthermore, galangin-treated LX-2 cells presented a significantly higher degree of apoptosis compared to cells treated with TGF-β1. The total apoptosis ratios (including early and late apoptosis ratios) were: 4.67 ± 0.74, 6.93 ± 1.10, 10.94 ± 1.87, 19.71 ± 2.57, and 71.32 ± 4.31%, respectively.

(A) Representative images of LX-2 cells apoptosis following 24 h exposure in galangin, using flow cytometry (n = 3); (B) The early LX-2 cells apoptosis rate of galangin; (C) The late LX-2 cells apoptosis rate; (D) The total LX-2 cells apoptosis rate. Each column shows the mean ± S.E.M. (n = 3 for each group). * p < 0.05, ** p < 0.01, *** p < 0.001 vs. the control group; # p < 0.05, ## p < 0.01, ### p < 0.001 vs. the TGF-β1 group.
HF is characterized by the excessive deposition of collagen I and α-SMA. As shown in Fig. 4, TGF-β1 has significantly increased the expression of mRNA and proteins, collagen I, and α-SMA compared to the control group. Galangin has reversed the expression of collagen I and α-SMA, indicating a potential anti-fibrogenic effect.

(A) Representative immunofluorescence images of collagen I and α-SMA in LX-2 cells following 24 h exposure in galangin (magnification: ×400), (B) Mean fluorescence intensity of collagen I; (C) Mean fluorescence intensity of α-SMA; (D) The mRNA level of collagen I, determined by RT-qPCR; (E) The mRNA level of α-SMA; (F) The protein level of Collagen I, α-SMA, and GADPH were detected via Western Blotting; (G) Collagen I and (H) α-SMA expression of was measured and presented in bar graph, GAPDH served as an internal control. Each column shows the mean ± S.E.M. (n = 3 for each group). * p < 0.05, ** p < 0.01, *** p < 0.001 vs. the control group; # p < 0.05, ## p < 0.01, ### p < 0.001 vs. the TGF-β1 group. (Color figure can be accessed in the online version.)
In order to explore the anti-fibrogenic mechanisms of galangin, we studied the PI3K/Akt pathway due to its important role in regulating proliferation, apoptosis, and autophagy in LX-2 cells. As shown in Figs. 5A–C, galangin has significantly restrained the expression of proteins phospho-PI3K and phospho-Akt, while has been upregulated by TGF-β1. These findings suggest that galangin inhibits PI3K/Akt signaling, suppressing the activation and proliferation of HSCs.

(A) Galangin restrained the proteins expression of phospho-PI3K and phospho-Akt in PI3K/Akt pathways: The protein level of phospho-PI3K, PI3K, phospho-Akt, Akt, and GADPH were detected via Western blotting; (B) phospho-PI3K and (C) phospho-Akt expression of was measured and presented in bar graph. (D) Galangin upregulated the expression of Bax and downregulated the expression of Bcl-2 in LX-2 cells, increased the Bax/Bcl-2 ratio: The protein level of Bax, Bcl-2, and GADPH were detected via Western blotting; (E) Bax and (F) Bcl-2 proteins expression; (G) the Bax/Bcl-2 ratio. (H), (K) Galangin inhibited the proteins expression of phospho-GSK-3β, and β-catenin in Wnt/β-catenin pathways. The protein level of phospho-GSK-3β, total β-catenin, active β-catenin and GADPH were detected via Western blotting; (I) phospho-GSK-3β, (J) total β-catenin and (L) active β-catenin expression. GAPDH served as an internal control. Data are shown as mean ± S.E.M. (n = 3 for each group). * p < 0.05, ** p < 0.01, *** p < 0.001 vs. the control group; # p < 0.05, ## p < 0.01, ### p < 0.001 vs. the TGF-β1 group.
Proteins of the Bcl-2 family, important regulators of mitochondria-mediated apoptosis, were chosen to investigate the effect of galangin on apoptosis. More specifically, we studied the anti-apoptotic protein Bcl-2 and the pro-apoptotic protein Bax. As shown in Figs. 5D–G, galangin has upregulated the expression of Bax and has downregulated the expression of Bcl-2 in LX-2 cells, increasing the Bax/Bcl-2 ratio in a concentration-dependent manner. These results suggest that galangin triggers the mitochondrial apoptotic pathway in part by regulating the expression of the Bcl-2 family of proteins.
Galangin Inhibits Wnt/β-Catenin SignalingThe Wnt/β-catenin pathway is engaged in the proliferation, differentiation, and apoptosis of HSCs. Figures 5H–L show that galangin was able to downregulate the expression of phospho-GSK-3β, total β-catenin and non-phospho(active) β-catenin, suggesting that it inhibits the Wnt/β-catenin pathway to increase HSCs apoptosis and autophagy.
In the present study, we investigated the anti-fibrogenic effect of galangin in vitro. The results suggest that galangin significantly reverses HF and induces HSCs apoptosis by disrupting the PI3K/Akt, Bax/Bcl-2, and Wnt pathways, playing an important role in the management of HF.
HF, a pathological condition caused by liver injury, is characterized by the excessive accumulation of ECM proteins produced by activated HSCs.33,34) These cells are modulated by several different agents including oxidative stress, growth factors, cytokines, and chemokines.35) Among them, TGF-β1 is a master regulator of pro-fibrogenic activities, acting on HSCs and affecting ECM expression.36,37) We treated HSCs with TGF-β1 to stimulate their activation. As a result, TGF-β1 increased the expression of α-SMA and collagen I, indicating that the transition of resting HSCs into myofibroblasts has been made successfully.38) We also found that the expression of mRNA, as well as the protein, α-SMA, and collagen I were significantly lower in the groups treated with galangin compared to those treated with TGF-β1. These results suggest that galangin is able to inhibit HSCs activation and ECM synthesis and may be a potential candidate for the treatment of hepatic fibrosis.39)
We also evaluated the underlying mechanism of the anti-fibrotic effect of galangin. Galangin has significantly inhibited cell viability and induced apoptosis at an increasing rate at concentrations between 6–10 µg/mL, leading to apoptosis in almost all cells at a concentration above 12 µg/mL, as shown by the blue nuclei on DAPI staining (Supplementary Fig. 1). The results suggest that galangin is able to trigger apoptosis in HSCs and that inhibiting the activation of HSCs and inducing their apoptosis could be an effective method to treat HF.40)
Our results also suggest that galangin is able to inhibit the PI3K/Akt signaling pathway by downregulating the phosphorylation of PI3K and Akt, which are activated by TGF-β1. Previous studies have shown that PI3K/Akt signaling plays a critical role in the process and progression of HF remodeling, including the activation, proliferation, and apoptosis of HSCs and ECM synthesis.13,41) It is clear that inducing apoptosis in activated HSCs is able to efficiently reverse this process.42,43) In this study, we found that galangin is able to inhibit HSC activation and ECM synthesis via the PI3K/Akt signaling pathway.
The mitochondrial pathway, one of the downstream signaling pathways regulated by Akt, is an important molecular signaling pathway of cell apoptosis, controlled by the Bcl-2 family of proteins.10) Earlier findings indicate that Akt can exert its anti-apoptotic effects by inhibiting Bax conformational change and Bax effects on the mitochondria.44,45) In the present study, TGF-β1 has downregulated the expression of Bax and upregulated the expression of Bcl-2, while galangin had an opposite effect. Furthermore, MK-2206 led to reduced levels of phospho-Akt and increased the Bax/Bcl-2 ratio (Supplementary Fig. 2). Thus, our results suggest that galangin may influence the mitochondrial pathway regulated by the Bax/Bcl-2 ratio via PI3K/Akt pathway, leading to the apoptosis of HSCs. Similar observations were made by other studies, where galangin was able to induce apoptosis in human gastric cancer SNU-484 cells.46)
The Wnt signaling pathway is a multifunctional pathway that regulates the development of HF.47) In normal, β-catenin is evident in the cytoplasm (total β-catenin) and nucleus (active β-catenin) to regulate target factors and activate target genes in Wnt pathway.48,49) In short, the total β-catenin, which accumulated in the cytoplasm, could enter the nucleus as its active form, known as the active β-catenin, and then combined with lymphocyte factor/lymphotropic factor (LEF/TCF), which can activate target genes of the Wnt signaling pathway, increasing pro-fibrogenic cytokines and protein expression of EMC compounds in HF.50,51) Our previous studies have shown that Akt could directly activate phospho-GSK-3β, a critical protein in the pathophysiological process of HF.52) Phospho-GSK-3β, the total β-catenin and active β-catenin were downregulated by galangin in the present study. To the best of our knowledge, Wnt signaling plays a role in increasing the anti-fibrogenic efficiency of galangin.53,54)
This study has a couple of limitations. Firstly, the anti-fibrogenic effect of galangin may be the result of the interaction of multiple pathways and multiple inhibitions. Secondly, it is not clear whether PI3K/Akt is the only pathway contributing to the anti-fibrogenic efficiency of galangin. The study of other pathways will be the subject of future research.
Our results suggest that galangin may reverse HF in LX-2 cells by inhibiting the PI3K/Akt signaling pathway and its downstream Bax/Bcl-2 and Wnt/β-catenin pathways. Therefore, galangin has the potential to become a promising candidate for the management of hepatic fibrosis.
The authors declare no conflict of interest.
The online version of this article contains supplementary materials.