2021 Volume 44 Issue 2 Pages 238-244
2021 Volume 44 Issue 2 Pages 238-244
Mirtazapine (MTZ) is a noradrenergic and specific serotonergic antidepressant. MTZ is reportedly associated with an increased risk of bleeding. However, the underlying mechanism remains unclear. In this study, we investigated the antiplatelet effect of MTZ in mice via light transmission aggregometry to elucidate the mechanism of MTZ-induced bleeding. The results of the ex vivo study showed that the oral administration of MTZ (20 or 100 mg/kg) significantly suppressed platelet aggregation mediated by the synergic interaction of 5-hydroxytryptamine (5-HT) and adrenaline. Additionally, MTZ significantly suppressed platelet aggregation, mediated by the synergic interaction of ADP and 5-HT or adrenaline. Similar results were obtained in vitro, under the condition of 5-HT- and adrenaline-induced platelet aggregation. Overall, the results suggest that MTZ exerts antiplatelet effect by co-blocking 5-HT2A and α2-adrenergic receptors on platelets and suppresses platelet aggregation mediated by ADP, increased by either 5-HT or adrenaline. Thus, a detailed monitoring of bleeding is recommended for patients taking MTZ.
Serotonergic antidepressants play an important role in the treatment of major depressive disorders, and selective serotonin reuptake inhibitors (SSRIs) are frequently used as the first-line treatment for depression.1) However, SSRIs have been reported to increase the risk of bleeding by inhibiting the reuptake of 5-hydroxytryptamine (5-HT), and thereby decrease the availability of 5-HT in the platelets.2) Therefore, SSRIs should not be used in patients with a high risk of bleeding.
Mirtazapine (MTZ) is a noradrenergic and specific serotonergic antidepressant.1) It is recommended as an alternative for patients with a risk of bleeding,2) because it does not have an inhibitory effect on serotonin reuptake. However, it has been reported that MTZ is also associated with an increased risk of bleeding. The antiplatelet effect of MTZ has been confirmed in a randomized double-blind placebo trial in post myocardial infarction patients with depression.3) The blood levels of two platelet activators, β-thromboglobulin (β-TG) and platelet factor 4 (PF4), were compared in the placebo and oral MTZ (30–40 mg/d for 8 weeks) groups. The results showed that although there were no significant differences between the two groups, the blood levels of β-TG and PF4 tended to decrease in the oral MTZ group.3) A case–control study, performed in 2011, to evaluate the risk of gastrointestinal (GI) bleeding during exposure to antidepressants in warfarin users reported that MTZ increased GI bleeding risk in less than 30 d after the first MTZ prescription.4) Furthermore, a meta-analysis reported no difference in the bleeding risk between patients taking MTZ and SSRIs.5) On the basis of these findings, we hypothesized that MTZ may affect platelet function and bleeding risk. However, the antiplatelet effect of MTZ has not been elucidated.
Platelet aggregation occurs in a two-step process, namely primary and secondary aggregation. When endothelial cells in the blood vessel are injured, primary hemostatic response (reversible primary aggregation of platelets) progresses. First, thrombogenic subendothelial matrix proteins, such as collagen and von Willebrand factor (vWF), are exposed to the blood stream. Next, the platelets in the site of vascular injury respond and adhere to the vessel wall by binding collagen and vWF to glycoprotein VI (GPVI) and glycoprotein Ib (GPIb) on the platelet membrane, respectively. These responses then trigger the release of ADP, 5-HT, and adrenaline from dense granules (δ granules),6–9) which then bind to P2Y1 and P2Y12, 5-HT2A, and α2 receptors on the platelet membrane, respectively. All these action mechanisms of 5-HT,10,11) adrenaline,12,13) and ADP14–16) are Ca2+-dependent, and they increase the intracellular Ca2+ level in platelets and subsequently amplify platelet activation. Thereafter, the glycoprotein IIb/IIIa (GPIIb/IIIa) receptors are expressed on the platelet membrane to bind to fibrinogen. The activated platelets connect with the surrounding platelets via fibrinogen binding with the GPIIb/IIIa receptors and result in secondary aggregation, which is an irreversible process.6–9) Additionally, ADP, 5-HT, and adrenaline act synergistically, and further enhance platelet aggregation.17–20)
MTZ has 5-HT2A and α2 receptor-specific antagonism in the neurons of the brain.1) Therefore, we hypothesized that MTZ exerts antiplatelet effects by blocking these receptors on the platelet membrane. In the present study, we investigated the effect of oral MTZ on platelet aggregation induced by typical platelet-aggregating agents and on the ADP platelet aggregation-enhancing effect of serotonin or adrenaline.
The drugs, platelet-aggregating agents, and chemicals used in the present study were purchased from the following manufacturers: MTZ and yohimbine hydrochloride (α2 receptor blocker) from Tokyo Chemical Industry Co., Ltd. (Tokyo, Japan); sarpogrelate hydrochloride (5-HT2A receptor blocker), 5-HT (platelet-aggregating agent), gelatin, and D(−)-mannitol from FUJIFILM Wako Pure Chemical Corporation (Osaka, Japan), human serum albumin from Nacalai Tesque, Inc. (Kyoto, Japan); dimethyl sulfoxide from Kanto Chemical Co., Inc. (Tokyo, Japan); and saline from Otsuka Pharmaceutical Co., Ltd. (Tokyo, Japan). As a platelet-aggregating agent, Levohem, a platelet aggregation agonist reagent kit for collagen, ADP, and adrenaline, was purchased from SYMEX (Kobe, Japan).
Preparation of Drug SolutionThe platelet-aggregating agents (collagen, ADP, and adrenaline) were dissolved and diluted according to the manufacturer’s instructions. 5-HT was dissolved and diluted with saline. MTZ, yohimbine hydrochloride, and sarpogrelate hydrochloride were dissolved in dimethyl sulfoxide and their concentrations were adjusted to 0.2 and 2 mg/mL (MTZ), 10 and 20 mM (yohimbine hydrochloride), and 10 and 20 mM (sarpogrelate hydrochloride), respectively. The prepared solutions were then diluted with saline, containing 0.1% human plasma albumin.
AnimalsMale Institute of Cancer Research mice (age, 8 weeks; weight, 32–36 g) were purchased from Sankyo Labo Service Co., Inc. (Tokyo, Japan). The mice were housed under standard conditions (23 ± 1 °C, 55 ± 5% relative humidity) and maintained under a 12-h light–dark cycle (lights on from 8:00–20:00 h), with free access to food and water for at least 4 d before the start of the experiment. All animal experiments were conducted in compliance with the protocol that was reviewed by the Institutional Animal Care and Use Committee and approved by the president of Tokyo University of Science (approval number: Y19059).
Blood CollectionApproximately 1 mL of blood was slowly collected from the heart of the mice into a plastic syringe (volume: 2.5 mL; needle size: 23 G), containing a 1/10 volume of 3.13% citrate sodium. Platelet-rich plasma (PRP) was obtained from the upper layer after centrifuging blood at 200 × g at room temperature for 10 min. Platelet-poor plasma (PPP) was obtained after centrifuging the residue at 1700 × g for 15 min at room temperature.
Measurement of Platelet AggregationPlatelet aggregation was measured using a light transmission aggregometer, PRP313M (IMI Co., Ltd., Saitama, Japan), according to the Born and Cross Method.20) Briefly, PRP (100 µL) was preincubated in a cuvette at 37 ± 0.5 °C for 15 min in the PRP313M. Platelet-aggregating agent (collagen, ADP, 5-HT + adrenaline, ADP +5-HT, or ADP + adrenaline) was added to PRP and the aggregation rate was recorded for 10 min. Assuming the light transmission of PPP as 100%, light transmission of the PRP sample was recorded as the aggregation rate.
Evaluation of the Ex Vivo Antiplatelet Effect of MTZ on Platelet Aggregation by Collagen, ADP, and the Combination of 5-HT and AdrenalineMice in the MTZ groups were orally administrated MTZ (suspended in solvent containing 0.375% gelatin and 3.75% D-mannitol), at a dose of 20 or 100 mg/kg, and mice in the control group were orally administrated solvent containing 0.375% gelatin and 3.75% D-mannitol. The volume of the orally administrated liquid was adjusted to 5 mL/kg. Blood samples were collected after an hour of oral administration. Collagen (final concentration: 10 µg/mL), ADP (final concentration: 5 µM), or combination of 5-HT (final concentration: 5 µM) and adrenaline (final concentration: 5 µM) were added to PRP as the platelet-aggregating agents. The maximum platelet aggregation rate (%) was measured for each group and compared.
Evaluation of the Ex Vivo Effect of MTZ on ADP Platelet Aggregation Enhanced by 5-HT or AdrenalineThe animal experiments were performed in the same way as described in the previous section. A combination of ADP (final concentration: 5 µM) and 5-HT (final concentration: 5 and 10 µM) or ADP (final concentration: 5 µM) and adrenaline (final concentration: 5, 10 µM) were added to PRP as the platelet-aggregating agent. Platelet aggregation rate curves were obtained by measuring the platelet aggregation rate for 10 min. The slope was calculated from the regression for a set of four points, collected every minute in the process of changing from primary aggregation to secondary aggregation. The starting point was defined as the point showing the maximum aggregation rate in the primary aggregation. Thereafter, the difference in platelet aggregation form was evaluated based on the slope of the regression line.
In Vitro Study to Examine the Mechanism of Action of MTZBlood samples were collected from the mice immediately before the experiment. MTZ (2 or 20 µg/mL), yohimbine (100 µM), and sarpogrelate (100 µM) were added to 100 µL PPP to obtain final MTZ, yohimbine, and sarpogrelate concentrations of 0.2 or 2.0 µg/mL, 10, and 10 µM, respectively. The prepared solutions were preincubated for 15 min at 37 °C ±0.5 °C, and then platelet-aggregating agent, 5-HT (5 µM) or adrenaline (5 µM), was added to induce aggregation. Platelet aggregation rate was measured for 10 min in each group, and the maximum platelet aggregation rate (%) was compared.
Statistical AnalysisThe maximum platelet aggregation rate in the ex vivo and in vitro studies is expressed as mean ± standard deviation (S.D.). Dunnett’s test was performed, using SPSS Statistics version 23.0, for comparison, and results with p-values less than 0.05 were considered statistically significant. The transition from primary to secondary platelet aggregation in the ex vivo study was assessed using a linear regression analysis, with Bonferroni adjusted significant levels, and results with p-values less than 0.05 were considered statistically significant. R Studio version 3.6.1 was used as the statistical analysis software.
We confirmed whether platelets were aggregated by treatment with adrenaline or 5-HT alone or their combination. Although adrenaline and 5-HT alone at 10 µM did not induce the aggregation of mouse platelets (data not shown), the combined administration of these two agonists caused the aggregation of mouse platelets. Under the condition of platelet aggregation induced by the co-administration of 5-HT and adrenaline, the maximum platelet aggregation rate was significantly reduced from 67 ± 18% in the control group to 23 ± 20% in the MTZ 20 mg/kg group and to 3.0 ± 0.9% in the MTZ 100 mg/kg group, and the platelet aggregation inhibitory effect of MTZ was dose dependent (Fig. 1A). Under the condition of platelet aggregation induced by ADP, MTZ had no effect on platelet aggregation. In addition, under the condition of collagen-induced platelet aggregation, a significant antiplatelet effect was observed only in the MTZ 100 mg/kg group, and the platelet aggregation inhibitory effect was MTZ dose-dependent (Fig. 1C).

A) Platelet-aggregating agent: 5 µM 5-HT +5 µM adrenaline. Control: n = 13, MTZ 20 mg/kg: n = 7, MTZ 100 mg/kg: n = 9. B) Platelet-aggregating agent: 5 µM ADP. Each group: n = 9. C) Platelet-aggregating agent: 10 µg/mL collagen. Each group: n = 10. Each value represents mean ± S.D. * p < 0.05; ** p < 0.01 compared with the control values.
Under the condition of ADP-induced platelet aggregation, the platelet aggregation rate decreased over time after the primary aggregation. In contrast, platelet aggregation was enhanced and the aggregation continued (secondary aggregation) by the combination of 5-HT or adrenaline with ADP (Figs. 2A, 3A).

A) Typical result of the enhancement effect of ADP-mediated platelet aggregation by 5-HT. 5 µM ADP (Black line), 5 µM ADP +5 µM 5-HT (Red line), 5 µM ADP +10 µM 5-HT (Green line). B) Comparison of the slope of platelet aggregation curve after primary aggregation by 5 µM ADP +5 µM 5-HT. C) Comparison of the slope of platelet aggregation curve after primary aggregation by 5 µM ADP +10 µM 5-HT. Thin lines and markers indicate individual data and thick line indicates the regression line. Linear regression analysis using Bonferroni adjusted significant levels. *: p < 0.05. n = 5. (Color figure can be accessed in the online version.)

A) Typical results of the enhancement effect of ADP-mediated platelet aggregation by adrenaline. 5 µM ADP (Black line), 5 µM ADP +5 µM adrenaline (Red line), 5 µM ADP +10 µM Adrenaline (Green line). B) Comparison of the slope of platelet aggregation curve after primary aggregation by 5 µM ADP +5 µM adrenaline. C) Comparison of the slope of platelet aggregation curve after primary aggregation by 5 µM ADP +10 µM adrenaline. Thin lines and markers indicate individual data, and the thick line indicates the regression line. A linear regression analysis using Bonferroni adjusted significant levels. *: p < 0.05. n = 4. (Color figure can be accessed in the online version.)
From the platelet aggregation curve, the platelet aggregation data of four points were collected every minute, starting from the point at which the platelets transitioned from primary aggregation to secondary aggregation. An evaluation of the difference in slope of the regression line, obtained from the platelet aggregation rate curve, showed significant differences between the control group and MTZ 20 mg/kg group or MTZ 100 mg/kg group. This suggests that MTZ could decrease the enhancement effect of ADP platelet aggregation by 5-HT, and thereby decrease the transition to secondary aggregation, at both 20 and 100 mg/kg doses (Figs. 2B, C).
Conversely, under the condition of ADP-induced platelet aggregation enhanced by 5 µM adrenaline, no significant difference was observed at a dose of MTZ 20 mg/kg, whereas a significant difference was observed at a dose of MTZ 100 mg/kg. In addition, under the condition of ADP-induced platelet aggregation enhanced by 10 µM adrenaline, significant differences were observed between the control group and MTZ 20 mg/kg or MTZ 100 mg/kg group. Moreover, owing to the fact that the ADP-induced platelet aggregation-enhancing effect of adrenaline was less effective than that of 5-HT, a significant difference was not observed under the condition of ADP-induced platelet aggregation enhanced by 5 µM adrenaline (Figs. 3B, C).
In Vitro Study to Examine the Mechanism of Action of MTZThe maximum platelet aggregation rate, induced by the combination of 5-HT and adrenaline, was significantly reduced from 72 ± 22% in the control group to 11 ± 8.0% in the 0.2 µg/mL MTZ group and 2.2 ± 1.1% in the 2.0 µg/mL MTZ group. This indicates that the antiplatelet effect was exerted by MTZ and not its metabolite.
Yohimbine (10 µM, α2 antagonist) and sarpogrelate (10 µM, 5-HT2A antagonist) inhibited the maximum platelet aggregation rate, enhanced by the combination of 5-HT and adrenaline, by 11.0 ± 9.5 and 6.0 ± 6.7%, respectively. In addition, the coincidental addition of 10 µM yohimbine or sarpogrelate further inhibited the maximum platelet aggregation rate to 3.0 ± 1.0%. The antiplatelet activity involved the co-blocking of 5-HT2A and α2 receptors (Fig. 4).
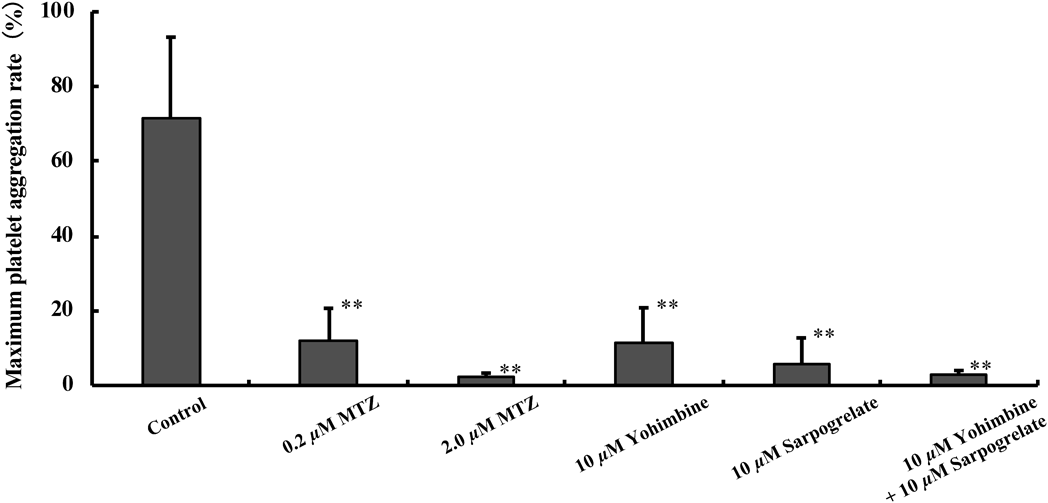
In this experiment, the mechanism of action of MTZ was investigated using sarpogrelate, a 5-HT2A receptor-selective inhibitor, and yohimbine, an α2 receptor-selective inhibitor. Control: n = 8, 0.2 µg/mL MTZ: n = 6, 2.0 µg/mL MTZ: n = 5, 10 µM Yohimbine: n = 3, 10 µM Sarpogrelate: n = 4, 10 µM Yohimbine +10 µM Sarpogrelate : n = 3. Each value represents mean ± S.D. ** p < 0.01 compared with the control values.
Collagen is considered one of the most potent vessel wall components involved in the initiation of platelet aggregation. When collagen binds to the GPVI receptor on the platelet membrane, ADP, 5-HT, and adrenaline are secondarily released from the δ granules. The action of these platelet activating factors on the respective receptors promotes platelet aggregation.6–9,21,22) Under the condition of 5-HT- and adrenaline-induced platelet aggregation, MTZ showed a significant antiplatelet effect (Fig. 1A). In contrast, under the condition of ADP-induced platelet aggregation, MTZ did not inhibit ADP-induced aggregation (Fig. 1B). These results suggest that MTZ inhibited platelet aggregation via the 5-HT2A and α2 receptors and not the P2Y1 and P2Y12 receptors, present on the platelet membrane. Under the condition of collagen-induced platelet aggregation, a significant antiplatelet effect of MTZ was observed only in the high-dose MTZ group (Fig. 1C). As collagen-induced platelet aggregation is associated with not only 5-HT and adrenaline, but also ADP released from the δ granules, MTZ could not completely inhibit platelet aggregation by collagen.
Many aggregating agonists act in synergism to induce platelet aggregation via multiple receptors and pathways. ADP is released from the δ granules in response to agonist stimulation and can synergize with 5-HT or adrenaline to activate platelets.16–19) Therefore, we examined whether MTZ could suppress the platelet aggregation effect of ADP, synergistically enhanced by 5-HT and adrenaline. Our results showed a sequential decrease in the platelet aggregation rate due to the dissociation of primary platelet aggregates under the condition of ADP-induced aggregation. However, platelet aggregation rate was either maintained or increased spontaneously, under the condition of ADP-induced aggregation, enhanced by 5-HT or adrenaline (Figs. 2A, 3A). These results suggest that 5-HT and adrenaline promote secondary platelet aggregation and change platelet aggregation to the irreversible aggregation form. However, the oral administration of MTZ, at a dose of 20 or 100 mg/kg, prevented the progression of secondary platelet aggregation by 5-HT or adrenaline, thereby enabling the redistribution of platelets (Figs. 2B, C, 3B, C). This indicates that the secondary aggregation, induced by ADP and 5-HT or adrenaline, was suppressed by the blocking of the 5-HT2A and α2 receptors on the platelets by MTZ; MTZ appears to affect the time-dependent changes. In this study, the effect of MTZ was not confirmed under the condition of platelet aggregation induced by the combination of ADP, 5-HT, and adrenaline. However, MTZ is expected to exert an inhibitory effect on platelet aggregation even under the condition for platelet aggregation induced by all three aggregating agents.
It was not clear from the results of the ex vivo studies whether the observed antiplatelet effect was due to MTZ or its metabolites. Therefore, the antiplatelet effect of MTZ was examined in vitro. A dose of 0.2 µg/mL MTZ is equivalent to the maximum blood concentration (Cmax) in Asians taking 30 mg MTZ or in Caucasians taking 75 mg MTZ.23,24) The antiplatelet activity was observed even at a concentration of 0.2 µg/mL MTZ. This suggests that the unaltered MTZ exerted the antiplatelet effect (Fig. 4).
To identify the receptors that mediated the antiplatelet effect of MTZ, we evaluated their activity by comparing the in vitro antiplatelet effect of 5-HT2A and α2 receptor antagonists. We showed that yohimbine, which is used as an α2-adrenergic receptor antagonist, inhibited platelet aggregation induced by the combination of 5-HT and adrenaline. A similar effect was observed for sarpogrelate, which is used as a 5-HT2A receptor antagonist. In addition, a simultaneous addition of yohimbine and sarpogrelate considerably inhibited platelet aggregation induced by the combination of 5-HT and adrenaline. These results suggest that MTZ exhibits antiplatelet effect by co-blocking these two receptors (Fig. 4).
The treatment concentrations of sarpogrelate and yohimbine were set based on previous studies.25–28) Because the concentrations of sarpogrelate and yohimbine in this study are more than 10-fold higher than the Ki values for the 5-HT2A receptor25) and α2 receptor,26) respectively, we consider that these drugs would completely block the respective receptors under the condition of this study. We showed that the inhibitory effect of 2 µM MTZ on platelet aggregation was higher than that of 10 µM yohimbine or 10 µM sarpogrelate (Fig. 4). This result suggests that MTZ may also exert a stronger antiplatelet effect under our experimental conditions than yohimbine and sarpogrelate.
In conclusion, MTZ exerts antiplatelet activity by co-blocking the 5-HT2A and α2 receptors and suppresses the ADP-induced aggregation-enhancing effect induced by 5-HT or adrenaline. Therefore, a detailed monitoring of bleeding is needed for patients taking MTZ.
This work was supported by a Research Education Fund for Tokyo University of Science.
The authors declare no conflict of interest.