2014 Volume 78 Issue 10 Pages 2519-2520
2014 Volume 78 Issue 10 Pages 2519-2520
A 61-year-old man with hypertension and smoking history presented to hospital because of sudden dizziness a few days beforehand. His vital signs were stable, but echocardiography showed a mobile, solid mass with halo adjacent to the proximal portion of the right coronary artery on parasternal short axis view (Figure A, arrow). A small amount of pericardial effusion and hypokinesis of the inferior wall were also noted. Electrocardiography showed no ischemic change.
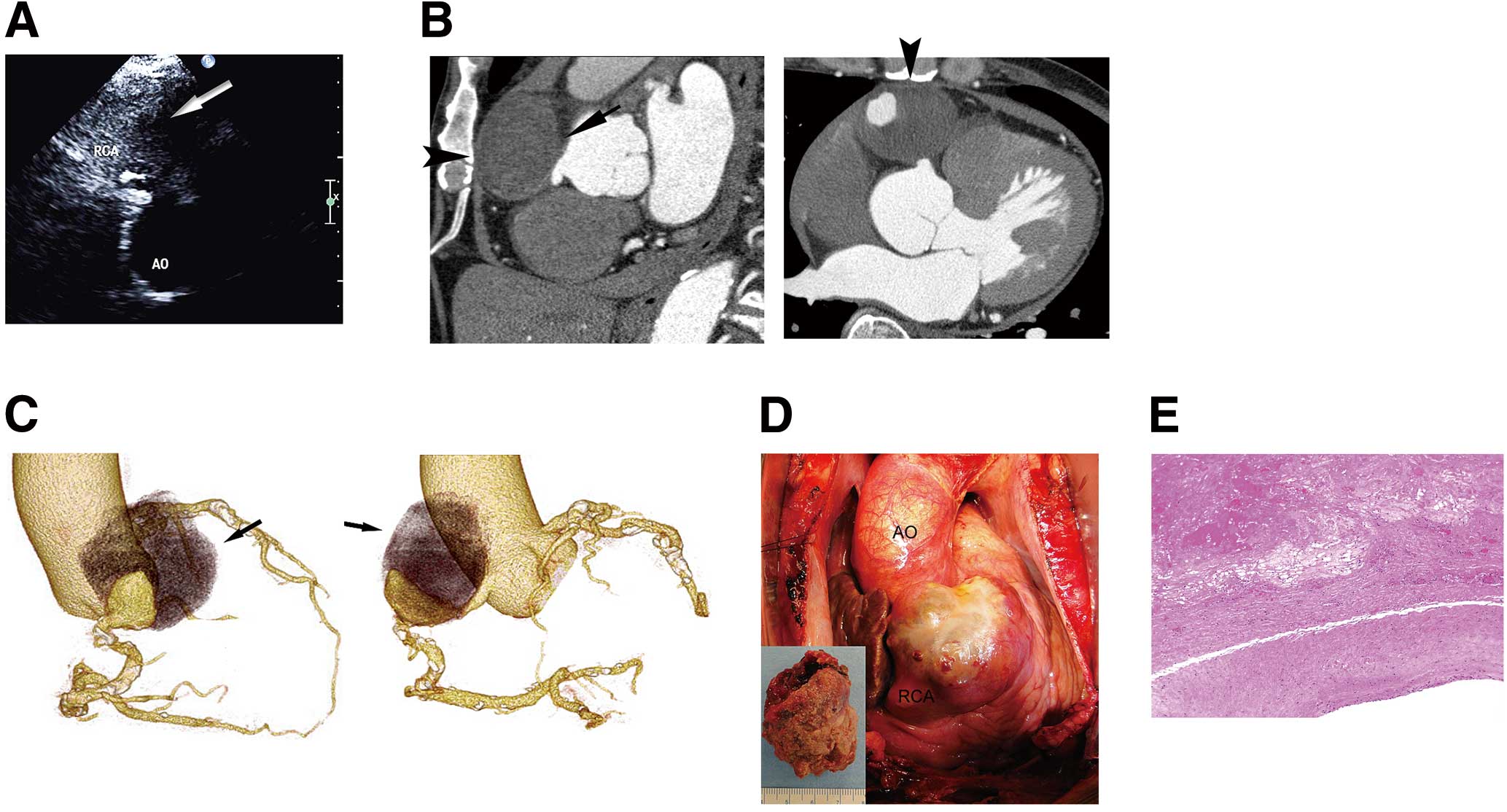
(A) Giant, thrombotic right proximal coronary artery aneurysm (CAA) detected on echocardiography: mobile, solid mass with halo (arrow) adjacent to the proximal portion of the right coronary artery in parasternal short axis view. Ao, aorta; RCA, right coronary artery. (B) Enhanced computed tomography (CT) angiography showed a giant, thrombotic right CAA (arrow) and a small amount of pericardial effusion. Both sagittal and horizontal sections of the CT clearly indicated that the CAA was compressed from the outside by the sternum (arrowheads), suggesting that spontaneous hemostasis of the CAA rupture had occurred partly due to compression by the sternum, resulting in limited pericardial effusion. (C) Three-dimensional coronary CT of giant right CAA (left, right anterior oblique view; right, left anterior oblique view) showing a giant aneurysm 48×33×55 mm in diameter with thrombus in its upper portion (arrows). (D) Appearance of the giant right CAA at operation, after sternotomy and pericardiotomy. There is a small hen’s egg-sized aneurysm at the base of the aorta, the surface of which appeared thickened but vulnerable, with inflammatory change. The site of the CAA rupture could not be clearly identified. (Inset) Thrombotic content of the resected CAA. (E) Histopathology of the resected CAA wall. On hematoxylin and eosin staining of the resected CAA wall, cholesterin clefts and deposition of eosinophilic granules in necrotic centers of the intima (Upper), thinning of the media, and mild infiltration of lymphocytes and plasma cells into the adventitia (Lower), were seen, indicating severe atherosclerosis.
Enhanced computed tomography (CT) angiography showed a giant, thrombotic right coronary artery aneurysm (CAA; Figure B, arrow) and a small amount of pericardial effusion. The density of pericardial effusion became lower and the amount was smaller on plain CT compared to that on CT taken 6 days previously at another hospital. Therefore, the CAA was assessed as having ruptured but spontaneously stopped. On CT, on both sagittal and horizontal sections, the aneurysm was clearly found to be compressed from the outside by the sternum (Figure B, arrowheads), suggesting that spontaneous hemostasis of the CAA rupture had been induced partly due to compression by the sternum, resulting in limited pericardial effusion. Three-dimensional coronary CT showed a giant aneurysm of 48×33×55 mm in diameter with thrombus in its upper portion (Figure C, arrows).
Surgical resection of the aneurysm was promptly performed. We found no adhesion between the back of the sternum and pericardium, but found a moderate amount of bloody pericardial effusion. There was a small hen’s egg-sized aneurysm at the base of the aorta, the surface of which appeared thickened but vulnerable, with inflammatory change (Figure D). The site of the aneurysm rupture could not be clearly identified. A few days later, the patient was discharged from hospital without complications.
CAA is a rare abnormality that has been found in 0.15–4.9% of patients undergoing coronary angiography.1 Currently, the term “aneurysm” is defined as an artery with a diameter >1.5-fold that of the adjacent normal segment, and that with a diameter >40 mm is referred to as a “giant aneurysm”.2 The most common etiology of CAA is atherosclerosis, which accounts for 50% of cases, and the other etiologies include Kawasaki disease,3 congenital malformation, polyarteritis nodosa, infection, trauma, and angioplasty.2 In the present case, histopathology of the resected CAA wall indicated that the etiology was atherosclerosis (Figure E).
Most patients who have CAA are asymptomatic in general, but once symptoms emerge the aneurysm can cause severe life-threatening complications such as myocardial infarction and rupture. The treatment strategy is not well established. Medical therapy consists of an antiplatelet and anticoagulation agent to prevent embolization.4 In contrast, surgical therapy consists of ligation and resection of the CAA together with coronary artery bypass grafting,5,6 but there is no evidence to indicate which treatment is superior to the other.
In the present case, the patient had fortunately stayed alive with only the symptom of dizziness because hemostasis of the CAA rupture had spontaneously occurred with subsequent prompt surgery. Rigorous management of the present patient’s hypertension would definitely be needed.