2016 Volume 80 Issue 3 Pages 750-752
2016 Volume 80 Issue 3 Pages 750-752
Takotsubo syndrome is a cardiac syndrome involving acute onset of ST segment elevation on electrocardiography (ECG), mimicking acute myocardial infarction, but with a normal coronary artery.1 Left ventriculography (LVG) shows apical ballooning akinesis and basal hyperkinesis in the typical case. This syndrome is not rare, but its pathophysiology remains unclear.
A 77-year-old woman presented to hospital with sudden-onset chest pain at rest. ECG showed ST elevation in the V2–4 leads (Figure 1A). Transthoracic echocardiography showed abnormal wall motion with akinesis in the mid-ventricle and hyperkinesis in the basal and apical area with estimated ejection fraction of 48%. Cardiac enzyme of troponin I was slightly elevated (1.13 ng/ml; normal, <0.10 ng/ml). On suspected acute coronary syndrome, urgent coronary angiography (CAG) was performed but no significant stenosis was seen in the epicardial coronary arteries, with TIMI 3 flow (Figures 1B,C); also, spasm provocation test with ergonovine was negative. LVG was notable for mid-ventricle ballooning with hyperkinesis in the basal and apical area (Figures 1D,E). A pressure gradient was not detected between the outflow tract and the apex of the left ventricle (LV). These findings were indicative of mid-ventricular ballooning cardiomyopathy, a subtype of takotsubo syndrome, along with an episode of mental stress. To determine if microvascular dysfunction (MVD) was coexisting or not, fractional flow reserve (FFR), coronary flow reserve (CFR) and index of microcirculatory resistance (IMR) were measured in the left anterior descending artery with pressure wire (Figure 1F) as previously described.2 FFR, CFR and IMR were 0.94, 1.80 and 66.0, respectively (normal, >0.80, >2.0 and <25, respectively). IMR was remarkably high compared with normal, indicating that microvascular function was highly impaired. The patient was treated with continuous infusion of nicorandil to improve coronary perfusion, and heparin to prevent thrombosis. The next day, serial rest thallium-201 (201Tl) and iodine-123-β-methl-p-iodophenyl penta-decanoic acid (123I-BMIPP) dual-isotope myocardial single-photon emission computed tomography (SPECT) was performed. The polar map of perfusion and BMIPP imaging demonstrated slightly decreased myocardial perfusion and highly decreased uptake of BMIPP in the mid-ventricle area (Figure 1G), suggesting localized transient ischemia. Summed defect scores for 201Tl and 123I-BMIPP were 1 and 8, respectively. On the 5th day after admission, normalization of ECG (Figure 2A) and transthoracic echocardiography was observed. The patient was discharged on the 12th day without any symptoms or complications. Plasma catecholamine and virus antibody concentration were normal. At 1 month after onset, several follow-up examinations were performed with written informed consent. After CAG again confirmed no obstructive coronary disease, pressure wire examination was performed (Figure 2B). FFR, CFR and IMR were 0.91, 5.0 and 19.2, respectively, indicating full recovery from MVD. LVG also showed recovery from LV dysfunction (Figures 2C,D). 201Tl-123I-BMIPP SPECT showed remarkable improvement of uptake of BMIPP in the mid-ventricle area (Figure 2E).
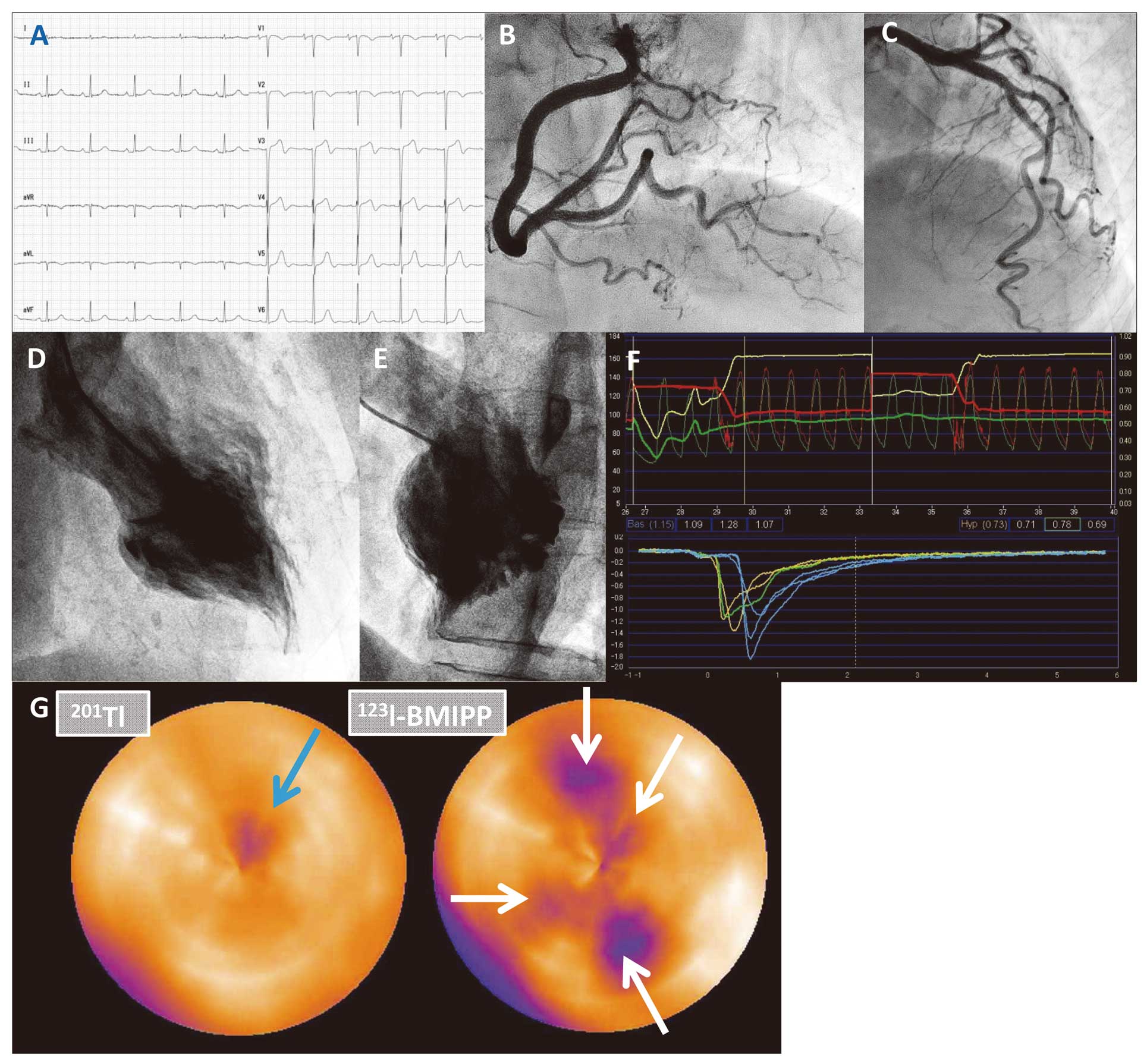
(A) Electrocardiography on admission showing ST elevation in the V2–4 leads. (B,C) Coronary angiography showing no significant stenosis in the (B) right coronary artery or (C) left coronary artery. (D,E) Left ventriculography demonstrating akinetic wall motion of the mid-ventricle with hyperkinesis in the basal and apical area (D, RAO; E, LAO). (F) Pressure curve data in the acute phase. (G) 123I-BMIPP uptake less than perfusion uptake in the mid-ventricular in the acute phase. Light blue arrow, decreased myocardial perfusion; white arrows, decreased uptake of BMIPP in this area. 123I-BMIPP, iodine-123-β-methl-p-iodophenyl penta-decanoic acid; 201Tl, thallium-201.
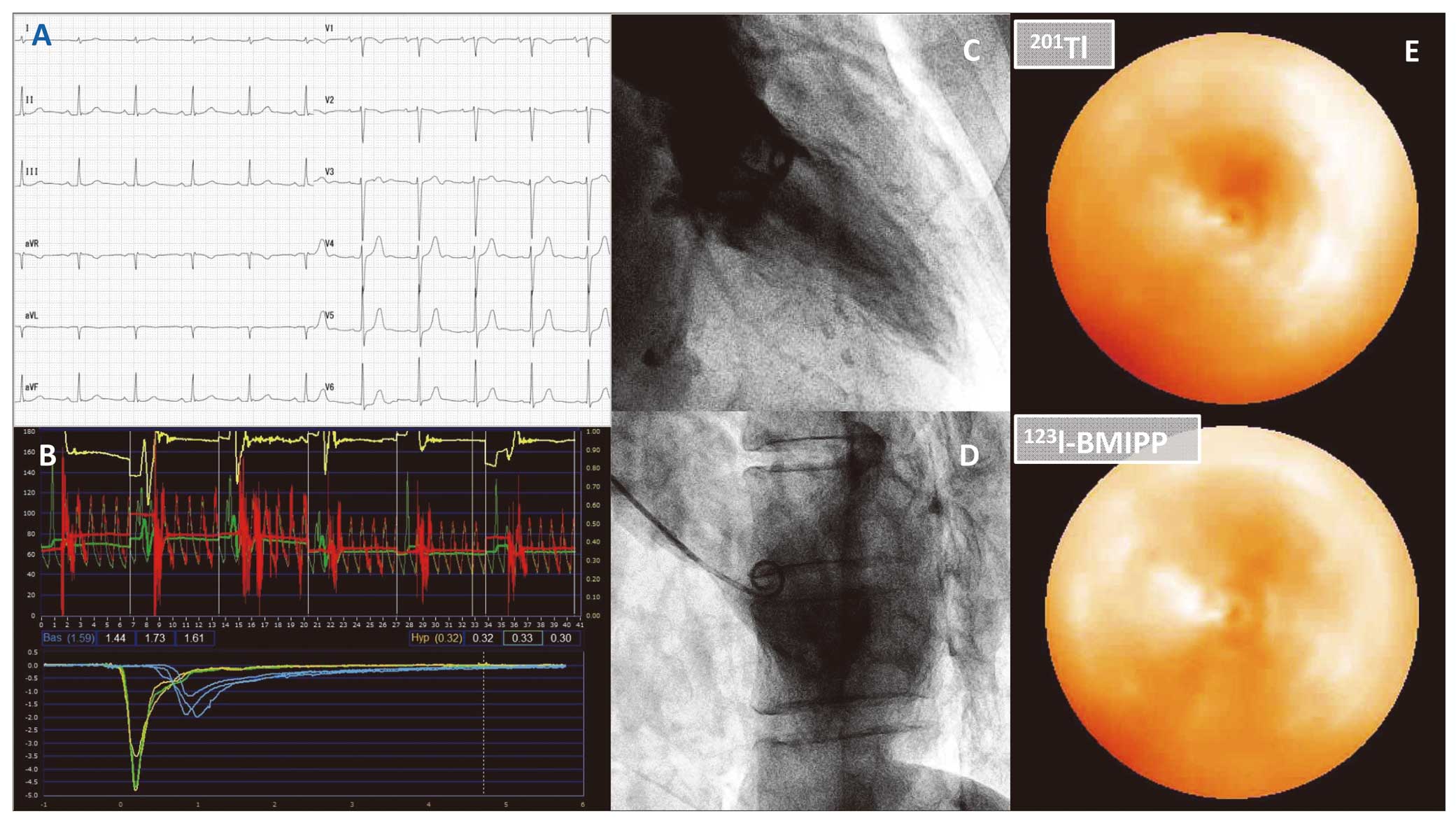
(A) Electrocardiography showing improvement of ST elevation. (B) Pressure curve data in the chronic phase. (C,D) Left ventriculography showing normal wall motion (C, RAO; D, LAO). (E) No discordance between uptake of 201Tl and 123I-BMIPP in the chronic phase. 123I-BMIPP, iodine-123-β-methl-p-iodophenyl penta-decanoic acid; 201Tl, thallium-201.
Takotsubo syndrome was first described in Japan and was named after an octopus trap, the appearance of which is similar to the apical ballooning seen on LVG in the typical case.3 Some subtypes are also known, such as mid-ventricular as well as inferior wall ballooning syndrome, with similar clinical presentations.4 The present patient had one of the subtypes, showing mid-ventricular ballooning with basal and apical hyperkinesis. Although approximately 25 years have passed since the first description, the details of the underlying mechanism are still unclear. Multivessel coronary spasm, MVD, catecholamine overload, and a combination of them have been suggested as a cause of the ventricular wall motion.5,6 In the present case, although coronary spasm was not observed and plasma catecholamine was normal, only MVD was confirmed on measurement of IMR. It was not able to be determined, however, whether MVD was the cause of takotsubo syndrome or the result.
Reversibility of MVD in this syndrome has been demonstrated non-invasively on Doppler transthoracic echocardiography7 and positron emission tomography,8 and invasively with intracoronary Doppler wire9 in previous studies using CFR. IMR, however, is considered more useful to detect MVD because of the independence of epicardial stenosis and hemodynamic status,10,11 but only 2 cases of MVD in takotsubo syndrome have been reported using IMR in the acute phase.12,13 To the best of our knowledge, this is the first case report in which IMR was evaluated twice in the same patient.
This case was distinguished by 3 points as follows. First, the presence of MVD was confirmed in a rare subtype of takotsubo syndrome, the pathophysiology of which is still uncertain.4,14 Second, the reversibility of MVD in this syndrome was confirmed using the novel technique of IMR for the first time. Third, the transient ischemia due to MVD was also confirmed with 201Tl-123I-BMIPP SPECT, which has been previously used to document this syndrome.15,16
None.