2017 Volume 81 Issue 12 Pages 1824-1831
2017 Volume 81 Issue 12 Pages 1824-1831
Background: Valve-preserving aortic surgery is increasingly used in acute aortic dissection type A (AADA). The object of this study was to compare the long-term results of aortic root remodeling (remodeling) for patients with and without AADA.
Methods and Results: Between October 1995 and December 2013, 776 patients underwent valve-preserving root replacement, of whom 59 patients with AADA (<2 weeks from onset, 56±16 years, 48 male) underwent remodeling (the remodeling-group); 7 patients had bicuspid anatomy (12%), 3 had Marfan syndrome (5%), and 1 had undergone previous cardiac surgery (2%). For this analysis the control group of patients who underwent remodeling for stable aneurysm (n=59) was generated using a propensity score matching. The long-term outcomes regarding survival and reoperation on the aortic valve were compared between the 2 groups. Pre- and intraoperative patients’ characteristics were comparable between groups. Early death was 7% in the AADA group and 3% in the control group (P=0.40). Actuarial survival at 10 years of the AADA group (72±6%) was insignificantly lower than that of the control group (83±5%) (P=0.16). Freedom from reoperation at 10 years was similar (AADA group: 98±2%, control group: 97±3%, P=0.99). Multivariable Cox’s proportional hazards model could not identify an independent predictor for late reoperation but advanced age for late death.
Conclusions: Long-term stability of remodeling was comparable between patients with and without AADA.
The primary goal of surgical intervention for acute aortic dissection type A (AADA) should unquestionably be to save the patient’s life. Reconstitution of the aortic wall layers with tubular aortic replacement is therefore widely accepted as the standard care in this setting and acceptable early and long-term results have been reported.1–4 However, in cases of preexisting root dilatation, this type of operation exposes the patient not only to potential risk of future proximal reoperation because of further dilatation of the root with or without aortic valve regurgitation (AR) but also the risk of postoperative bleeding from a very thin aortic wall. Therefore, more liberal use of an aggressive approach to the aortic root has been proposed by some groups, especially for patients with connective tissue disease.5 The Bentall operation using a mechanical composite prosthesis implies, however, lifelong need for anticoagulation, which might have a negative effect on patients requiring future distal reoperation.6 In addition, it has been reported that the Bentall operation has a negative effect on thrombosis of the distal false lumen.7 Another alternative using a biological prosthesis (e.g., a stentless valve) seems less suitable for young patients with regard to structural valve deterioration.8 Therefore, valve-preserving root replacement has gained increasing attention in treatment for this cohort.
Nonetheless, surgeons are still reluctant to preserve the aortic valve (AV) for these critically ill patients. Recent reports have demonstrated that the Bentall operation does not increase operative deaths in the setting of AADA,9,10 although it is still controversial.11,12 Valve-preserving root replacement is definitively more technically demanding and time-consuming operation than the Bentall operation; thus only reports with mixed results from experienced institutions of cases with AADA have been published.13–18 We published our experience of valve-preserving root replacement for AADA in 2000,19 and updated it in 2016 by focusing on the aortic root remodeling (remodeling) technique alone in a larger number of patients and with longer follow-up.20 We concluded that remodeling was not associated with increased risk in terms of both early mortality/morbidities and long-term outcomes (e.g., survival and reoperation) compared with standard alternatives. However, these studies do not solve the question of whether remodeling can offer the same quality outcome for patients with AADA as well as for those with stable aneurysm. Normally, most of the patients with AADA have near-normal AV morphology, so it can theoretically be preserved more easily than a stretched one. Therefore 2 comparable groups with regard to root dimension and cusp morphology are essential to evaluate the role of valve-preserving root replacement for AADA. In the current study we sought to compare long-term valve stability and survival after remodeling between patients with AADA and a propensity score-matched cohort without AADA.
Between October 1995 and December 2013, 776 patients underwent valve-preserving root replacement, of whom 66 with AADA underwent either remodeling (n=59) or AV reimplantation (reimplantation) (n=7) in the emergency setting. During the same period, 215 patients underwent surgical intervention for AADA, of whom 26 underwent root replacement using a composite graft and 66 had valve-preserving aortic root replacement. The definition of AADA was surgery within 2 weeks from onset of symptom regardless of early thrombosis of the false lumen. Another 710 patients with stable chronic aneurysm also underwent either remodeling (n=688) or reimplantation (n=22) electively. The 59 patients with AADA who underwent remodeling (AADA group) was further analyzed and compared with 59 patients with stable chronic aneurysm who underwent remodeling and were selected by a propensity score-matching as described later (control group) (Figure 1). The institutional ethical committee approved the anonymous use of patients’ data. Mean age was slightly higher in the control group (60±16 years) compared with the AADA group (56±16 years) (P=0.15). Majority of patients were male in both groups (81% in the AADA group; 69% in the control group, P=0.13). One patient in the AADA group (2%) had undergone previous coronary artery bypass grafting through a median sternotomy and 3 patients in the control group (5%) had a history of previous coronary artery bypass grafting, mitral valve repair, and commissurotomy of the AV (P=0.31). Marfan syndrome and bicuspid AV (BAV) anatomy were present in 3 (5%) and 7 (12%) patients in the AADA group and in 1 (2%) and 8 (14%) patients in the control group, respectively (P=0.31 and 0.78). Preoperative mean AR grade was similar between the groups (2.3±0.7 in the AADA group and 2.2±0.8 in the control group, P=0.83). Baseline characteristics of the 2 groups were comparable as shown in Table 1.
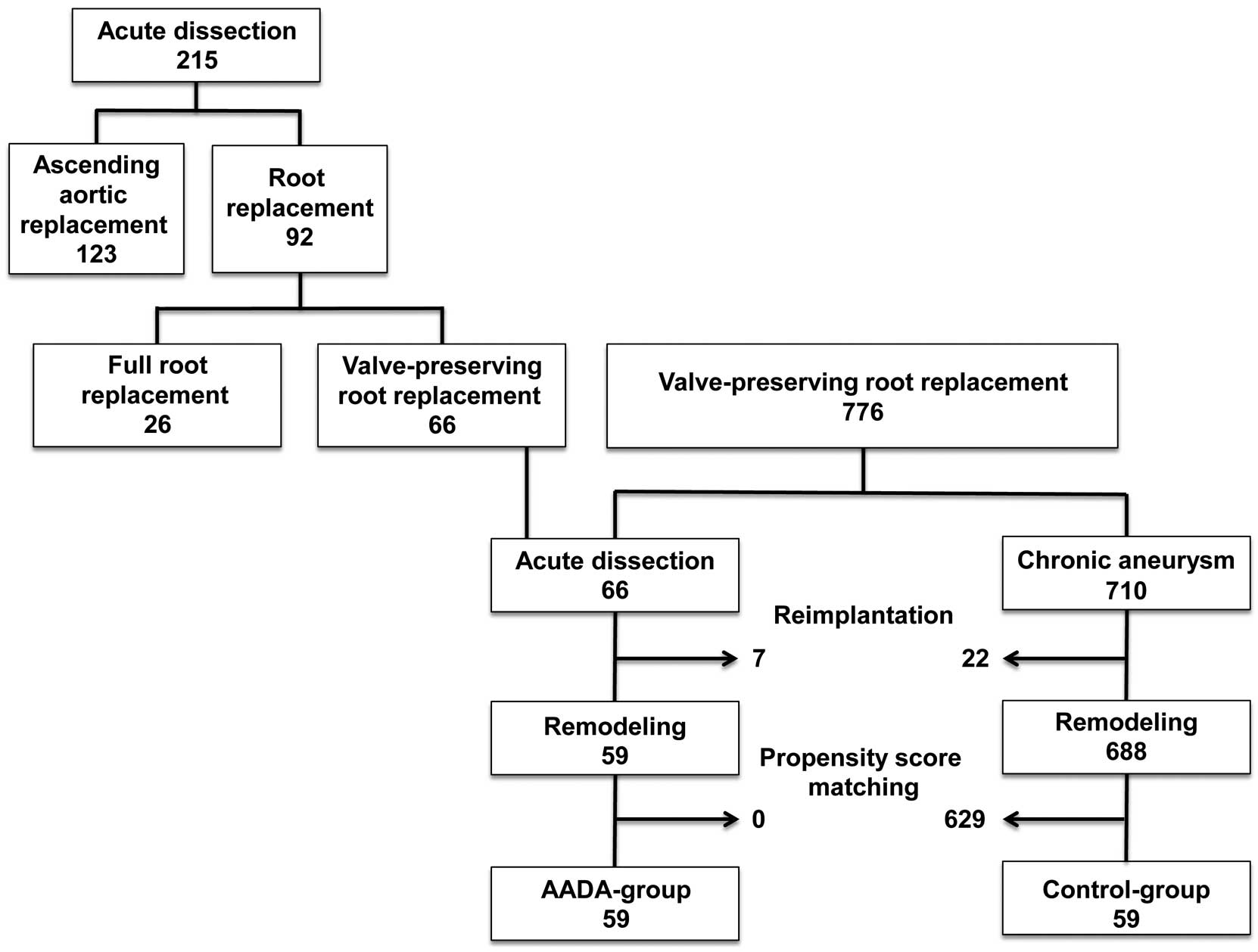
Flowchart of the study patients who underwent valve-preserving root replacement.
| Chronic aneurysm | AADA (n=59) |
P value | ||
|---|---|---|---|---|
| Unmatched (n=688) |
Matched (n=59) |
|||
| Baseline characteristics | ||||
| Sex (male) | 562 (82%) | 41 (69%) | 48 (81%) | 0.13 |
| Age (years) | 54±15 | 60±16 | 56±16 | 0.15 |
| Body height (cm) | 177±10 | 175±8 | 178±9 | 0.15 |
| Body weight (kg) | 83±16 | 85±18 | 86±17 | 0.72 |
| Body surface area (m2) | 2.0±0.2 | 2.0±0.2 | 2.1±0.2 | 0.79 |
| Bicuspid aortic valve | 283 (41%) | 8 (14%) | 7 (12%) | 0.78 |
| Marfan syndrome | 26 (4%) | 1 (2%) | 3 (5%) | 0.31 |
| Operated year since 2004 | 466 (68%) | 33 (56%) | 26 (44%) | 0.20 |
| Previous cardiac/aortic operation | 39 (6%) | 3 (5%) | 1 (2%) | 0.31 |
| AR grade | 2.5±0.8 | 2.2±0.8 | 2.3±0.7 | 0.83 |
| Root geometry | ||||
| AVJ diameter (mm) | 29±4 | 28±3 | 28±3 | 0.74 |
| Valsalva sinus diameter (mm) | 51±8 | 52±9 | 54±6 | 0.25 |
| STJ diameter (mm) | 39±6 | 38±6 | 39±5 | 0.30 |
| Operative procedures | ||||
| Central cusp plication | 560 (81%) | 35 (59%) | 29 (49%) | 0.27 |
| External suture annuloplasty | 289 (42%) | 10 (17%) | 6 (10%) | 0.28 |
| Concomitant CABG | 107 (16%) | 4 (7%) | 4 (7%) | NA |
| Partial arch replacement | 81 (12%) | 57 (97%) | 55 (93%) | 0.40 |
| Total arch replacement | 29 (4%) | 1 (2%) | 4 (7%) | 0.17 |
| Duration of CPB (min) | 105±30 | 118±38 | 148±54 | <0.01 |
| Duration of AXC (min) | 77±17 | 84±19 | 95±25 | <0.01 |
| Duration of circulatory arrest (min) | 11±8 | 10±9 | 17±7 | <0.01 |
| Prosthesis (mm) | 25±1 | 25±1 | 25±1 | 0.29 |
AADA, acute aortic dissection type A; AR, aortic valve regurgitation; AVJ, aortoventricular junction; AXC, aortic cross-clamping; CABG, coronary artery bypass grafting; CPB, cardiopulmonary bypass; NA, not applicable; STJ, sinotubular junction.
However, because of the underlying nature of the disease, patients in the AADA group had more severe morbidities than the control group. The median duration from onset of symptom to the operation was 9 h and 25 patients (42%) were operated within 6 h of the onset of symptoms, 20 patients (34%) between 6 and 24 h, and 10 patients (17%) between 1 and 14 days (4 unknown exact time of onset). Preoperative hypotension caused by cardiac tamponade was observed in 21 patients (36%), of whom 2 required cardiopulmonary resuscitation as salvage (1 patient survived the operation, the other died of stroke on the 7th postoperative day). A total of 15 patients (25%) had malperfusion of the brain (n=3), coronary artery (n=3), upper extremity (n=1), lower extremities (n=8), or spinal cord (n=2).
Choice of Root ProcedurePreoperatively all patients underwent transesophageal echocardiography (TEE; ATL HDI-3000TM, Philips Ultrasound, Bothell, WA, USA, or Sequoia 256TM, Acuson, Mountain View, CA, USA). The diameter of the sinuses of Valsalva, aortoventricular junction (AVJ), and sinotubular junction (STJ) were measured and their mean diameters were comparable between the groups (Table 1).
When the aortic root was not dilated (<42–45 mm according to body size), a tubular ascending aortic replacement±valve repair was chosen. When the aortic root was dilated, it was replaced by either composite-valved conduit in the presence of AV degeneration or valve-sparing technique if the cusps were pliable. The degree of AR, the presence of cusp prolapse or fenestration, and the size of aortic root were not considered as exclusion criteria for valve preservation. Coronary dissection was also not a contraindication for valve preservation, which was seen in 3 patients in the AADA group. The aortic root was dissected in all patients, but primary entry was found in the aortic root in 8 patients (14%). Originally, we performed remodeling in cases of AVJ ≤29 mm and reimplantation with a larger AVJ. Since January 2008, we have only applied remodeling.
Anesthesia and Operative TechniqueOur routine technique of valve-sparing root replacement and anesthesia has been described in detail.21 Briefly, all 3 sinuses are excised in all instances. In the AADA group, the dissected wall layers of the root were adapted by biologic glue in the early series (n=18), but thereafter no adhesive was applied to the root (n=41). A Dacron graft (Intergard, MAQUET GmbH & Co. KG, Rastatt, Germany) was chosen with a diameter similar to that of the native AVJ, taking the body size of the patient into consideration. In the AADA group, 24- and 26-mm grafts were selected similarly (n=30, 28, respectively; a 22-mm graft was used in 1 patient), whereas the 26-mm graft was predominantly used in the control group (22-, 24-, 26-, and 28-mm graft was used in 2, 23, 31, and 3 patients, respectively). We cut 3 tongues in the graft and sutured these into the aortic root close to the cusp insertion lines. In cases of BAV, 2 tongues were created in 180-degree configuration. Care was taken to preserve the maximum height of the commissures. In 16 patients (AADA group: 6, control group: 10) since January 2009 an external suture annuloplasty using a CV-0 expanded polytetrafluoroethylene suture was added (W. L. Gore & Associates, Flagstaff, AZ, USA).22 The suture was tied around a Hegar dilator (23- or 25-mm according to body size).
After completion of root replacement the aortic cusp configuration was assessed carefully. Before 2004, prolapse was evaluated by visual inspection. Thereafter the height difference between the central coaptation of the cusp margin and the nadir of aortic insertion (effective height) was measured routinely and an effective height <9 mm was considered as prolapse and corrected to 9–10 mm in each cusp.23 Cusp prolapse was present in almost half of the patients (49% in the AADA group, 59% in the control group) and corrected by central plication of the free margin using a single 5-0 or 6-0 polypropylene suture (ProleneTM; Ethicon, Hamburg, Germany).24 This was more frequently performed after 2004 (23/26, 88% in the AADA group; 28/33, 85% in the control group) compared with before (6/33, 18% in the AADA group; 7/26, 27% in the control group, P<0.01 for both group). There was no statistical difference in the degree of preoperative AR between the patients requiring cusp plication or not (2.3±0.7 vs. 2.5±0.7, P=0.38 in the AADA group; 2.2±1.0 vs. 2.3±0.5, P=0.45 in the control group). Average AVJ diameter was identical between groups (both 28±3 mm); however, patients with a large AVJ diameter (≥28 mm) was more frequent in the AADA group (n=31, 53%) than in the control group (n=22, 38%) without statistical power (P=0.10). The coronary ostia were always reimplanted using the button-technique. Intraoperative TEE was performed after discontinuation of cardiopulmonary bypass to confirm valve configuration and function.
A majority of the patients (n=55, 93% in the AADA group, n=57, 97% in the control group) underwent partial arch replacement with a short period of circulatory arrest and a nasopharyngeal temperature of 18±1℃. In 4 patients in the AADA group with complex entry in the distal aortic arch, replacement was extended into the total arch with an “elephant trunk” technique and reinforcement with Teflon felt (DuPont Pharmaceuticals, Wilmington, DE, USA). Only 1 patient in the control group with diffuse thoracic aneurysm underwent a total arch replacement. Gelatin resorcin formalin glue (Cardial, Technopole, Sainte-Etienne, France) was used to obliterate the false lumen in the aortic arch in the early series and BioglueTM (Cryolife International Inc., Kennesaw, GA, USA) was used in the recent series.
Propensity Score-Matching AnalysisUsing multivariable logistic regression analysis, the probability of being assigned to the AADA group over the control group was calculated from baseline characteristics and operative procedures (Appendix). P<0.10 was defined for selecting variables for entry into the final model. Using selected covariables, a propensity score was calculated for each patient. Each patient with AADA was matched to 1 patient with stable aneurysm with the closest propensity score. The mean difference of propensity score for matching was 0.10±0.07 (0–0.22). Using this technique, comparable patient cohorts (59 patients from each group) were identified for the final analysis (AADA group and control group). Baseline characteristics of propensity-matched pairs were almost similar for baseline characteristics, root geometry, and operative data excepting duration of the procedure (Table 1). All matched patients were operated on by a single surgeon (H.-J.S.).
Clinical EndpointsAll surviving patients were followed clinically with a mean follow-up time of 110±60 months (2–238 months, except for early death). There was no statistical difference between the groups in terms of follow-up time: 112±62 months in the AADA group and 108±60 months in the control group (P=0.74). For the AADA group, echocardiography and computed tomography or magnetic resonance imaging were scheduled at 3, 6, and 12 months postoperatively, then annually or biennially. For the control group, echocardiography was planned annually or biennially after the operation. Long-term outcomes with regard to reoperation on the AV or death were compared between groups. The factors influencing late valve stability and all-cause death were analyzed using Cox’s proportional hazard’s model.
Statistical AnalysisStatistical analysis was performed using the StatView 5.0 program (SAS Institute Inc., Cary, NC, USA) or the Statistical Program for Social Sciences for Windows (version 17.0; SPSS, Chicago, IL, USA). All values are expressed as mean±standard deviation, except for data from the Kaplan-Meier curves, which are expressed as mean±standard error. Kaplan-Meier curves were transected at 15 years because of the small number of patients at risk thereafter and compared between the groups using the log-rank test. P<0.05 was considered statistically significant. Factors listed in the Appendix were entered into the analysis of predictors for late death and freedom from reoperation. P<0.1 in the univariable analysis was defined for selecting variables for entry into the multivariable analysis in the Cox’s proportional hazards model for survival and freedom from reoperation.
There were no significant differences between the 2 groups regarding most parameters except for a significantly longer procedural time in the AADA group (Table 1). Coronary dissection occurred in 3 patients in the AADA group, necessitating coronary artery bypass grafting and intra-aortic balloon pumping for treatment of myocardial dysfunction. Partial cavopulmonary shunt for right ventricular unloading was performed in 2 of these cases;25 1 patient died 3 days postoperatively but the other 2 survived the operation. Re-exploration for bleeding was performed in 10 patients in the AADA group (17%, 8% since 2007) and in 7 patients (12%, 4% since 2007) in the control group (P=0.43). The mean total postoperative discharge from the mediastinal drainage tube was 1,082±802 mL in the AADA group and 761±337 mL in the control group (P=0.07). A total of 3 patients (5%) in the AADA group and 2 in the control group (3%) developed postoperative permanent stroke (P=0.65). Only 1 patient in the AADA group (2%) required postoperative temporary hemodialysis, compared with none in the control group (P=0.32). The mean postoperative ventilation time was 1.3±3.2 days in the AADA group and 0.9±4.3 days in the control group (P=0.63) (ventilation time <24 h was defined as 0 days) (Table 2).
| Control (n=59) |
AADA (n=59) |
P value | |
|---|---|---|---|
| Re-exploration for bleeding | 7 (12%) | 10 (17%) | 0.43 |
| Discharge from drainage tube (mL) | 761±337 | 1,082±802 | 0.07 |
| Permanent stroke | 2 (3%) | 3 (5%) | 0.65 |
| Temporary hemodialysis | 0 | 1 (2%) | 0.32 |
| Ventilation time (days) | 0.9±4.3 | 1.3±3.2 | 0.63 |
| 30-day mortality | 2 (3%) | 4 (7%) | 0.40 |
In the AADA group 4 patients died within 30 days after surgery (7%) vs. 2 (3%) in the control group (P=0.40). Since 2002, no patients in the AADA group have died within 30 days after surgery. The causes of early death in the AADA group were cardiac (n=2), stroke (n=1), and acute pulmonary embolism (n=1). The cause of the 2 early deaths in the control group was both non-occlusive mesenteric ischemia. There were 12 and 7 late deaths in each group, respectively. The causes of late deaths were 7 cardiovascular, 2 non-cardiovascular, and 3 unknown in the AADA group, and 1 cardiovascular, 2 non-cardiovascular, and 4 unknown in the control group. Actuarial survival at 10 years in the AADA group (72±6%) was lower than in the control group (83±5%), although the difference was not significant (P=0.16) (Figure 2).

Late survival in patients with (red line) and without (blue line) acute aortic dissection type A (AADA).
Only 1 patient in each group underwent reoperation on the AV; the patient in the AADA group underwent AV replacement because of recurrent cusp prolapse at 1 year postoperatively and the other in the control group underwent AV replacement for cusp restriction at 5.5 years after the initial operation. The operations were performed in 2003 and 1997, respectively, when cusp configuration was still assessed visually. Actuarial freedom from reoperation on the AV at 10 years was thus quite similar: 98±2% in the AADA group and 97±3% in the control group (P=0.99) (Figure 3).

Freedom from reoperation on the aortic valve in patients with (red line) and without (blue line) acute aortic dissection type A (AADA).
In the AADA group, 4 patients underwent distal reoperation for persistent enlargement of the false lumen: 2 of the patients underwent replacement of the descending aorta at 4 months after partial aortic arch replacement and 4 years after total aortic arch replacement, respectively, and the other 2 patients underwent replacement of the total aortic arch and proximal descending aorta at 13 months and 14 years, respectively, after partial aortic arch replacement. All 4 patients survived the distal reoperations.
Cox’s Proportional Hazards ModelOur Cox’s proportional hazards model revealed no independent predictor for reoperation on the AV, because of the small incidence of reoperation. Univariable analysis identified 6 variables as significant predictors for late death, but only advanced age was significant in the multivariable analysis using 7 variables with P<0.1 (Table 3).
| Survival | OR | 95% CI | ||
|---|---|---|---|---|
| Univariate | Multivariate | |||
| Age | <0.01 | <0.01 | 1.068 | 1.024–1.114 |
| Body height | <0.01 | 0.59 | ||
| Body weight | 0.05 | 0.79 | ||
| Body surface area | 0.02 | 0.58 | ||
| Central plication | <0.01 | 0.31 | ||
| Concomitant CABG | 0.01 | 0.12 | ||
| Operated since 2004 | <0.01 | 0.45 | ||
CABG, coronary artery bypass grafting; CI, confidence interval; OR, odds ratio.
Although excellent long-term outcomes of valve-preserving root replacement have been reported from experienced institutions, surgeons are still reluctant to preserve the AV at the time of root replacement. From the 2014 Annual Report of the Japanese Association for Thoracic Surgery, the AV was preserved in only one-quarter of patients undergoing root replacement (276 of 1,142, 24%).12 According to a report from the Society of Thoracic Surgeons (STS) database, the AV was preserved less frequently (1,918 of 13,743, 14%).26 However, the proportion of patients with aortic stenosis (AS) was unknown in the Japanese report and was 38% (n=5,175) in the STS database, so the real frequency of valve-preserving root replacement for patients without AS is unknown.12,26 According to our original nationwide survey during 2014, valve-preserving root replacement was performed in only one-third (34%) of elective aortic root surgeries for pure AR in Japan (236 of 699).27 Nonetheless, valve-sparing root surgery was associated with the same postoperative mortality rate as an alternative,26,28,29 maybe because it was indicated for relatively low-risk patients (i.e., younger age) and performed in experienced institutions.30 Therefore, multi-institutional comparison of both approaches within homogeneous cohorts is essential to validate the role of valve-preserving root replacement.
In the setting of AADA, this trend is further accelerated. According to the IRAD international registry, aortic root replacement was performed in 35% of patients with AADA, consistent with other reports (26–40%).9,10,31,32 European surgeons were more aggressive (35–40%) than USA surgeons (30–35%), and Japanese surgeons were very conservative (8%).9,12 The majority of reports have revealed that root replacement was associated with the same or better short- and long-term survival compared with conservative tubular ascending aortic replacement. However, in the 2014 Annual Report of the Japanese Association for Thoracic Surgery, root replacement was associated with more than twice the in-hospital mortality (19.3%) compared with replacement of the ascending aorta with or without the aortic arch (8.1%), which might be the reason for the conservative attitude of Japanese surgeons towards root replacement.12 Of course, these results cannot simply be compared with ours because our cohort was relatively young and approximately one-quarter were operated on beyond 24 h from the onset of symptoms. In addition, a nationwide survey in Iceland clarified that in 17.6% of AADA cases the patient died prior to hospital arrival. This might also be the case in our study and one of the reasons for our favorable outcomes with selected candidates.33 Root replacement unquestionably requires a longer duration of myocardial ischemia, which seems unfavorable for critically ill patients with AADA. Therefore, the more time-consuming valve-preserving root replacement procedure in the setting of AADA has been performed for only selected patients in experienced institutions. Reimplantation has been performed in the majority of reports and associated with better mortality rates without increasing the risk of bleeding compared with the Bentall procedure despite the longer procedural duration.15,18 However, all reports compared 2 techniques in the small number of consecutive patients with limited follow-up period and without adjusting the operative risk, thus the real effect of valve-preserving root replacement in cases of AADA is unknown.
We have recently updated our experience of remodeling in the setting of AADA with a larger number of patients and longer follow-up.20 Our main message is that remodeling can be performed safely in these high-risk patients with acceptable early- and long-term outcomes compared with other standard alternatives. Contrary to surgeons’ expectations, the risk of bleeding was not increased with remodeling. However, the major limitation was the lack of a control group because the other alternatives were used in cases of different root dimensions and/or cusp pathology. In the current study, remodeling for patients with AADA was, therefore, compared with those without AADA by matching root geometry and cusp pathology using a sophisticated statistical method. Most importantly, freedom from reoperation was quite similar between groups. The initial operations of the 2 patients who required reoperation on the AV were performed before 2004 when cusp configuration was still assessed visually. Since 2009, we have routinely performed external suture annuloplasty,22 which may further improve late root stabilization. Long-term survival was also slightly inferior in AADA group because of the inherent nature of the disease, but AADA was not identified as an independent predictor for late death in the Cox’s proportional hazards model.
A previous report pointed out the inferior late results of remodeling compared with reimplantation for AADA patients,13 but recent reports present contradictory findings.16 Remodeling does not require extensive dissection of the root and only 1 suture line, so can be performed with a shorter duration of myocardial ischemia, which is advantageous for patients with AADA.16 In addition, visual inspection of the cup configuration and lack of annular stabilization might contribute to the inferior late results of remodeling in the early series. We abandoned comparing the 2 techniques because of small number of patients at risk of reimplantation operated in the emergency setting (n=7). Freedom from reoperation on the AV was quite inferior after reimplantation (64±21% at 10 years), although the patients were not comparable (unpublished data).
The indication for root replacement in the setting of AADA is preexisting root dilatation, extensive root destruction, or a known connective tissue disorder. These patients generally have a near-normal cusp, so are optimal candidates for valve-preserving options. On the other hand, extensive edema and hematoma of the aortic root might make the manipulation of the aortic root more difficult. We believe external suture annuloplasty is more suitable than external ring annuloplasty in this situation. Exact intraoperative judgment of root pathology is mandatory because of the lack of detailed preoperative diagnosis in the emergency setting. Owing to this trade-off, valve-preserving root replacement in cases of AADA should be performed in experienced institutions performing these techniques routinely on an elective basis.
Study LimitationsSeveral limitations were inherent in this study. First, this was not a randomized study but a retrospective study with consecutive patients. The operative technique has evolved in detail over time. However, the apparent difference in the underlying etiology prevented randomization. The consistent participation of a single surgeon (H.-J.S.) for both groups and a sophisticated statistical method may minimize the drawback of the retrospective nature of the current study. Second, the number of patients was still small and late adverse events occurred very infrequently to assess real differences between groups. Subgroup analysis within patients at high risk for recurrence (e.g., Marfan syndrome, BAV, larger annulus) may be of great interest. A multi-institutional registry should be mandatory, although inter-institutional technical differences might become another concern. Nonetheless, we believe we have proven the appropriateness of applying remodeling to patients with AADA with the same quality of outcome as those with stable root dilatation.
The long-term valve stability after remodeling was similar between patients with and without AADA. Advanced age was the only independent predictor for late death after remodeling.
The authors thank Mr. Frank Theisohn and Ms. Lucie Morgenthaler for their assistance with collecting the data.
The authors declare no conflicts of interest.
Factors entered into the propensity-score matching analysis to assign acute aortic dissection type A over non-dissection or the analysis of predictors for late aortic valve stability and late death using Cox’s proportional hazards model. Bold formatting indicates selected variable for entry into the final model for propensity score-matching.
Baseline Characteristics
Age
Sex
Body height
Body weight
Body surface area
Aortic valve insufficiency grade
Bicuspid aortic valve
Previous cardiac/aortic operation
Marfan syndrome
Operated on since 2004
Root Geometry
Aortoventricular junction diameter
Sinotubular junction diameter
Valsalva sinus diameter
Operative Procedures
Central cusp plication
External suture annuloplasty
Partial arch replacement
Total arch replacement
Concomitant coronary artery bypass grafting
Prosthesis size