2021 Volume 85 Issue 4 Pages 345-350
2021 Volume 85 Issue 4 Pages 345-350
Background: When an internal iliac artery (IIA) has to be embolized during endovascular aneurysm repair (EVAR), buttock claudication sometimes poses problems. However, there is no established method to evaluate intraoperative blood flow to the gluteal muscles.
Methods and Results: Gluteal regional oxygen saturation (rSO2) was monitored using near-infrared spectroscopy (NIRS) during surgery, and changes in rSO2 were compared with treatment results. Twenty-seven patients who underwent EVAR and IIA embolization at our institution between April 2019 and May 2020 were included in this study. The association between intraoperative changes in rSO2 and postoperative incidence of buttock claudication was analyzed. Furthermore, the presence or absence of communication between the superior and inferior gluteal arteries and the intraoperative changes in rSO2 were compared to ascertain whether rSO2 reflects blood flow change. Postoperative buttock claudication occurred in 4 of 19 patients (21%) with unilateral occlusion of IIA and in 4 of 8 patients (50%) with bilateral occlusion of IIAs. rSO2 was found to decrease significantly further in patients with buttock claudication than in patients without buttock claudication (−15±12% vs. −4±16%, P<0.05). In addition, rSO2 was predominantly lower in patients without the communication between the superior and inferior gluteal arteries than in those with the communication.
Conclusions: Gluteal rSO2 is useful as an indicator of intraoperative gluteal blood flow.
In cases of abdominal aortic aneurysms, it is common for the lesion to extend into the iliac artery and form a series of aneurysms. Unilateral and bilateral iliac aneurysms are associated with 40% of abdominal aortic aneurysm cases.1–3 Endovascular aneurysm repair (EVAR) for such cases requires internal iliac artery embolization to prevent type II endoleak from the internal iliac artery. Although it has been reported that pelvic visceral ischemia and buttock claudication may occur even with unilateral embolization of the internal iliac artery, there is no method of intraoperative blood flow assessment of the internal iliac artery system.4–6
Editorial p 351
Previous studies reported that muscle oxygenation and blood flow to regions including the gluteal muscle could be successfully evaluated using near-infrared spectroscopy (NIRS), which enables the comparison of subjects with different adipose tissue thicknesses by physiological calibration.7,8
The purpose of this study was to evaluate the usefulness of NIRS for monitoring the regional oxygen saturation (rSO2) of gluteal artery blood flow during EVAR by comparing changes in rSO2 with treatment results.
Of the 86 patients who underwent EVAR at our institution between April 2019 and May 2020, 27 patients were included and 2 bedridden patients with a Clinical Frailty Score of ≥7 were excluded from 29 patients with concomitant internal iliac artery embolization. Intraoperative changes in the rSO2 and postoperative incidence of buttock claudication were compared, and an assessment was performed to determine if changes in rSO2 are predictive of buttock claudication. Furthermore, the presence or absence of communication between the superior and inferior gluteal arteries, as well as the intraoperative changes in rSO2, were compared, and analysis was performed to determine whether the change in blood flow to the gluteal muscles at the site of embolization of the internal iliac artery was reflected by rSO2.
An INVOS 5100C oximeter (Medtronic) was used to measure rSO2. The sensor was placed symmetrically at the level of the supracaudal border 5 cm from the center line, and rSO2 was monitored continuously in the gluteal tissue and recorded at the start of anesthesia, at the start of surgery, at the end of embolization, at the end of surgery, and at the end of anesthesia.
Stent grafting was performed using a corporate stent graft. During internal iliac artery embolization, we embolized the central part of the internal iliac artery as much as possible to preserve flow in the superior and inferior gluteal arteries. However, we embolized the peripheral part of the internal iliac artery or the superior and inferior gluteal arteries if there was a complication of an internal iliac artery aneurysm. After embolization was completed, the sheath was replaced with a large-caliber sheath, and the stent graft was implanted. In general, the operation was performed under general anesthesia, but in cases of hypopnea, the operation was performed under local anesthesia. The presence or absence of gluteal claudication was determined by interviewing patients at hospital discharge and at the first outpatient visit after hospital discharge.
The NIRS INVOS 5100C oximeter is equipped with 2 light-emitting diodes that emit near-infrared light at 2 different wavelengths (730 and 810 nm) and 2 photodiodes that detect transmitted light, and signals from 2 photoreceptors located at different distances (3 and 4 cm) from the light emitter are used to determine signal information such as shallow skin. The rSO2 value denotes the oxygen saturation of blood in microvessels, and the local perfusion state can be evaluated by determining the change in the local oxygen demand and supply balance.7,9,10
Statistical AnalysisThe data are expressed as the mean±standard deviation, and the chi-squared test was used for statistical analysis. P<0.05 was considered to be statistically significant.
The mean age of the patients was 76±7 years, and 20 patients (74%) were men. The mean body weight was 60±13 kg, and the mean body mass index was 23±4 kg/m2. Eleven patients had an abdominal aortic aneurysm, 15 patients had an internal iliac aneurysm, and 1 patient had an abdominal aortic aneurysm with an internal iliac aneurysm. The mean maximum diameters of the abdominal aortic and internal iliac aneurysms were 52±10 and 39±10 mm, respectively (Table). Unilateral internal iliac artery embolization was performed in 22 patients and bilateral internal iliac artery embolization was performed in 5 patients. One patient underwent embolization with a plug and a coil, and 26 patients underwent embolization with only a coil. Three patients had unilateral internal iliac artery occlusion before surgery (Figure 1). The following devices were used: EXCLUDER C3 (W.L. Gore & Associates, USA) in 18 patients (67%), ENDURANT (Medtronic, USA) in 2 patients (7%), AFX (Endologix, Inc., USA) in 6 patients (22%), and Aorfix (Lombard Medical, Inc., USA) in 1 patient (4%). Iliac branch endoprosthesis (IBE; W.L. Gore & Associates, USA) was used in 2 patients, and we were able to preserve the internal iliac artery in both patients. Including patients with preoperative occlusion of the iliac artery, there were 19 patients with unilateral internal iliac artery occlusion and 8 patients with bilateral internal iliac artery occlusion (5 patients underwent bilateral embolization, and 3 patients underwent unilateral embolization and contralateral occlusion) (Figure 1). Buttock claudication was observed in 4 patients (21%) with unilateral occlusion and in 4 patients (50%) with bilateral occlusion (Figure 2). The communication between the superior and inferior gluteal arteries was preserved in 8 of the 22 patients (36%) who underwent unilateral embolization. Of the patients who underwent bilateral embolization, the communication was preserved bilaterally in 1 patient and unilaterally in 2 of 3 patients, but there was bilateral non-preservation of the communication in 1 patient (Figure 3). It was observed that rSO2 on the side of the proposed embolization began to decrease at the time of coil embolization, decreased most at the end of surgery, and recovered slowly at the end of anesthesia. The mean rSO2 values during EVAR in patients with and without buttock claudication were −15±12% and −4±16%, respectively (P<0.05) (Figure 4). The mean rSO2 values of patients with and without preserved communication between the superior and inferior gluteal arteries were 0±10% and −12±14%, respectively (P<0.05) (Figure 5). There was no case of intestinal ischemia or perioperative death.
| Characteristics | Values |
|---|---|
| Number of patients (n) | 27 |
| Age (years) | 76±7 |
| Gender, male | 20 |
| BW (kg) | 60±13 |
| BMI (kg/m2) | 23±4 |
| Clinical Frailty Score | 3±1 |
| Hypertension (%) | 22 (76) |
| Hyperlipidemia (%) | 9 (31) |
| Diabetes mellitus (%) | 2 (7) |
| Smoker (%) | 11 (38) |
| Maximum diameter of aortic aneurysm (mm) | 52±10 |
| Maximum diameter of iliac aneurysm (mm) | 39±10 |
| Devices used (n) | |
| Excluder C3 (IBE) | 18 (2) |
| Endurant | 2 |
| AFX | 6 |
| Aorfix | 1 |
| Unilateral IIA embolization (n) | 22 |
| Bilateral IIAs embolization (n) | 5 |
BMI, body mass index; BW, body weight; IBE, iliac branch endoprosthesis; IIA, internal iliac artery.
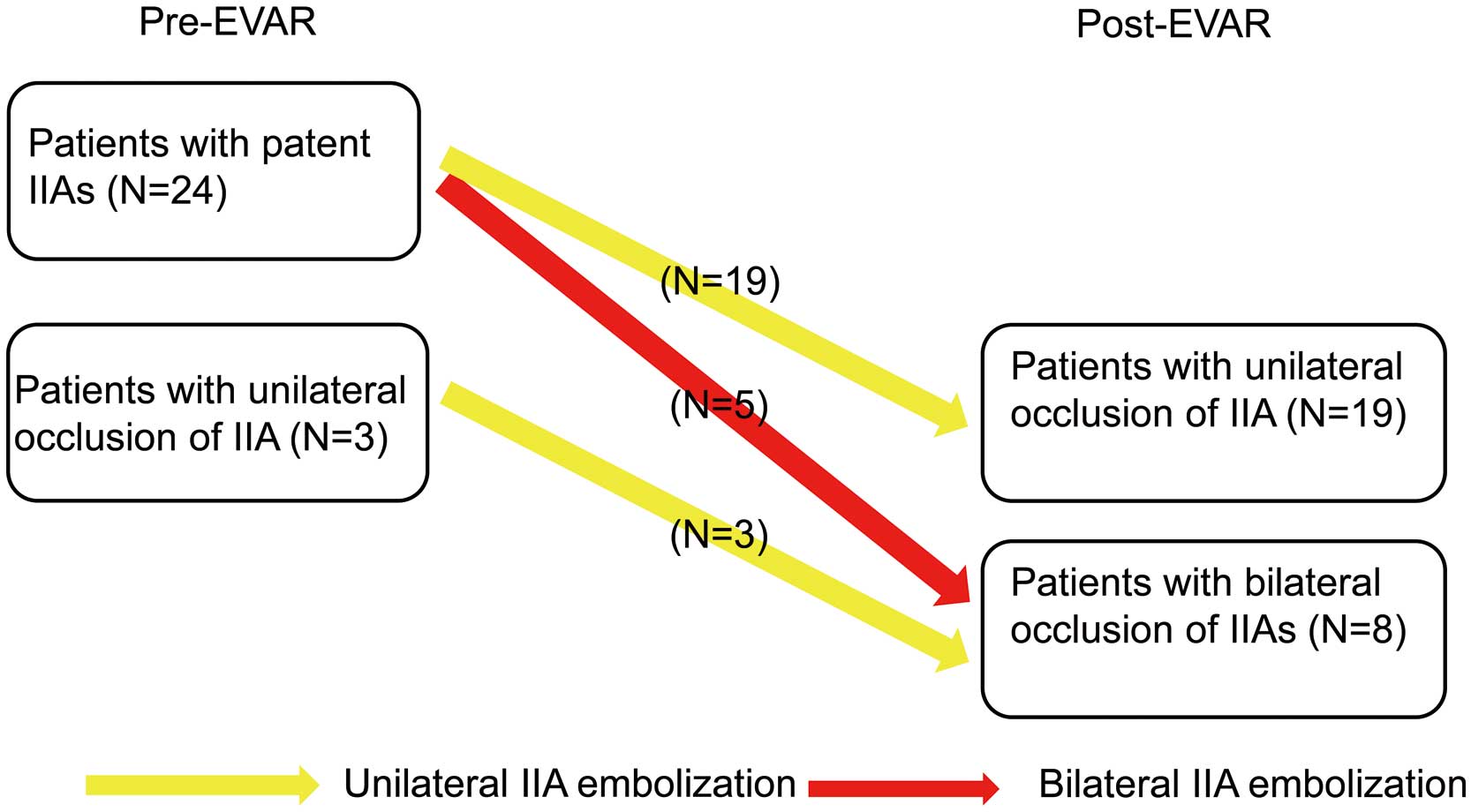
Preoperative and postoperative occlusion of the internal iliac arteries in patients undergoing endovascular aneurysm repair with internal iliac artery embolization. IIA, internal iliac artery.

Postoperative status of the internal iliac arteries and buttock claudication in patients undergoing endovascular aneurysm repair with internal iliac artery embolization. IIA, internal iliac artery.

Occlusion of the iliac arteries, communication between the superior and inferior gluteal arteries and postoperative buttock claudication in patients undergoing endovascular aneurysm repair with internal iliac artery embolization. SGA, superior gluteal artery; IGA, inferior gluteal artery. SGA-IGA communication (+), bilateral SGA-IGA communications are patent; SGA-IGA communication (+/−), unilateral SGA-IGA communication is patent and contralateral communication is absent; SGA-IGA communication (−), SGA-IGA communication is absent.
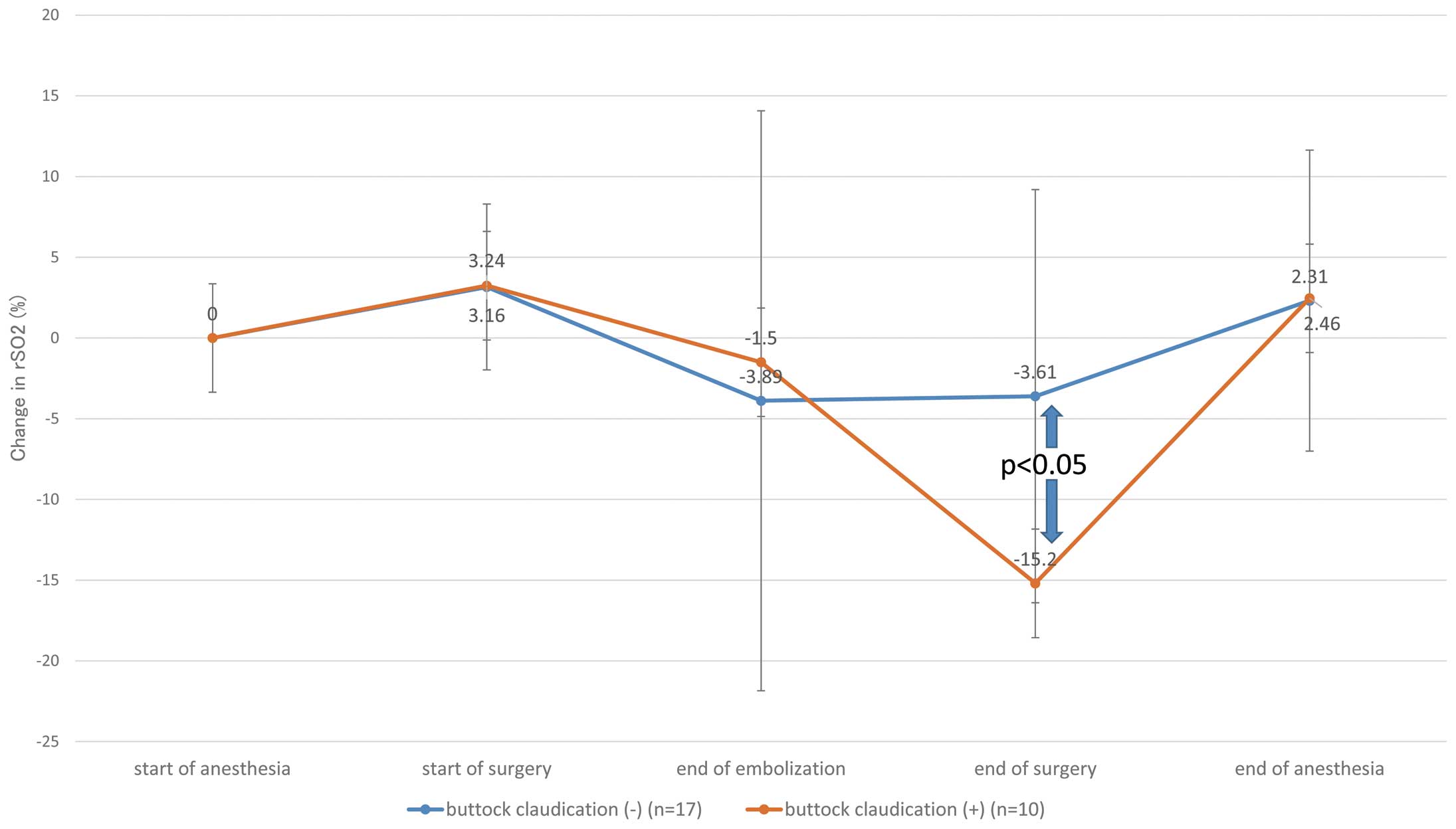
Change in gluteal regional oxygen saturation during surgery in patients with or without postoperative buttock claudication who underwent endovascular aneurysm repair with internal iliac artery embolization.

Change in gluteal regional oxygen saturation during surgery and communication between the superior and inferior gluteal arteries in patients undergoing endovascular aneurysm repair with internal iliac artery embolization. Thirty-two limbs with 22 unilateral and 5 bilateral IIA embolization were included in the study. SGA-IGA communication (+), SGA-IGA communication is patent; SGA-IGA communication (−), SGA-IGA communication is absent.
When abdominal aortic aneurysms are accompanied by iliac artery aneurysms, EVAR is performed with internal iliac artery embolization. However, it has been reported that pelvic visceral ischemia and buttock claudication can occur even with unilateral internal iliac artery embolization.5 Internal iliac artery embolization causes buttock claudication in ~30% of patients.3–6 Although there are many reports of improvement in claudication symptoms in the follow-up period, many patients are believed to suffer from persistent ischemic symptoms.6 However, there is no indication criteria for internal iliac artery reconstruction. For patients with unilateral internal iliac artery occlusion who require contralateral or bilateral embolization, it is reasonable to try to preserve blood flow as much as possible in the peripheral part of the internal iliac artery. High technical success rates and good short-term results have been reported with IBE;11–14 however, internal iliac artery occlusion of nearly 7% has also been reported in medium-term results.12 Anatomical unsuitability for IBE has also been reported in nearly 40% of patients.12,14 In this study, we measured rSO2 in the buttocks as an indicator of blood flow in the internal iliac artery. The collateral network concept proposed by Grippe et al states that all collateral vessels around the spinal cord affect spinal cord perfusion, and NIRS is used to measure the rSO2 of the spinal cord and its collateral vessels, which reflects the state of spinal cord perfusion.15–19 Similarly, we propose that continuous monitoring of rSO2 is useful for monitoring gluteal perfusion. It is rare for a single iliac artery to become severely ischemic because of a single occlusion, as the inferior mesenteric artery, the contralateral internal iliac artery, and the deep femoral artery form a network to maintain blood flow, and rSO2 in the gluteal tissues is considered a reflection of the perfusion status of this internal iliac artery system. It has been reported that coil embolization at the proximal part of the internal iliac artery can reduce the incidence of buttock claudication by preserving the communication between the superior and inferior gluteal arteries.5,6,20 In this study, rSO2 was found to be predominantly lower in the patient group without preserved communication; this suggests that blood flow in the internal iliac artery system can be maintained by preserving the communication between the superior and inferior gluteal arteries. In patients with buttock claudication, the demand for oxygen in the gluteal muscles has been reported to increase during exercise, resulting in ischemia and a decrease in rSO2 in the buttocks.10 In this study, intraoperative rSO2 was found to be significantly lower in patients with postoperative buttock claudication than in patients without postoperative buttock claudication. The decrease in rSO2 during EVAR even at rest is thought to be due to the obstruction of blood flow to the external iliac artery caused by the thick sheath of the stent graft and the decrease in blood flow from the deep femoral artery to the internal iliac artery system. Intraoperatively, the decrease in rSO2 meant a decrease in the blood supply capacity of the internal iliac artery network, which was reduced significantly in patients without preserved communication between the superior and inferior gluteal arteries and in patients with buttock claudication. In this study, rSO2, which was decreased at the time of EVAR, was found to recover after sheath removal, and no intestinal or spinal ischemic symptoms were observed. It was reported that buttock claudication occurred in a group with no reserve for acute pelvic ischemia.21 The intraoperative reduction in rSO2 observed in our study may suggest the absence of reserve for ischemia.
Study LimitationsThis study has several limitations. First, this is a single-center retrospective study. Second, the number of patients with gluteal claudication was low and not suitable for multivariate analysis. Third, subcutaneous fat thickness may have affected the NIRS signal.
The measurement of rSO2 in the buttocks using NIRS is useful for monitoring blood flow in the internal iliac artery system, and intraoperative reduction of rSO2 may be a predictor of gluteal claudication.
All the authors and co-authors have no conflicts of interest.
This study was approved by Kitasato University Hospital IRB (B18-143).