Abstract
Background:
The new guideline (NG) published by the Japanese Circulation Society (JCS) places emphasis on previous arrhythmic syncope and inducibility of ventricular fibrillation (VF) by ≤2 extrastimuli during programmed electrical stimulation (PES) for deciding the indication of an implantable cardioverter-defibrillator in patients with Brugada syndrome (BrS). This study evaluated the usefulness of the NG and compared it with the former guideline (FG) for risk stratification of patients with BrS.
Methods and Results:
This was a multicenter (7 Japanese hospitals) retrospective study involving 234 patients with BrS who underwent PES at baseline (226 males; mean age at diagnosis: 44.9±13.4 years). At diagnosis, 46 patients (20%) had previous VF, 100 patients (43%) had previous syncope, and 88 patients (37%) were asymptomatic. We evaluated the difference in the incidence of VF in each indication according to the new and FGs. During the follow-up period (mean: 6.9±5.2 years), the incidence of VF was higher in patients with Class IIa indication according to the NG (NG: 16/45 patients [35.6%] vs. FG: 16/104 patients [15.4%]), while the incidence of VF in patients with other than class I or IIa indication was similarly low in both guidelines (NG: 2/143 patients [1.4%] vs. FG: 2/84 patients [2.4%]).
Conclusions:
This study validated the usefulness of the NG for risk stratification of BrS patients.
Brugada syndrome (BrS) is an established high-risk factor for syncope or sudden cardiac death (SCD) in individuals with structurally normal hearts.1
A number of studies have noted a high recurrence rate of ventricular fibrillation (VF) in patients with BrS and a previous cardiac arrest.2–4
However, risk stratification of BrS patients without a history of VF or cardiac arrest has not been well evaluated.5
Editorial p ????
The new guideline (NG) from the Japanese Circulation Society (JCS) for the management of patients with BrS was published in 2018.6
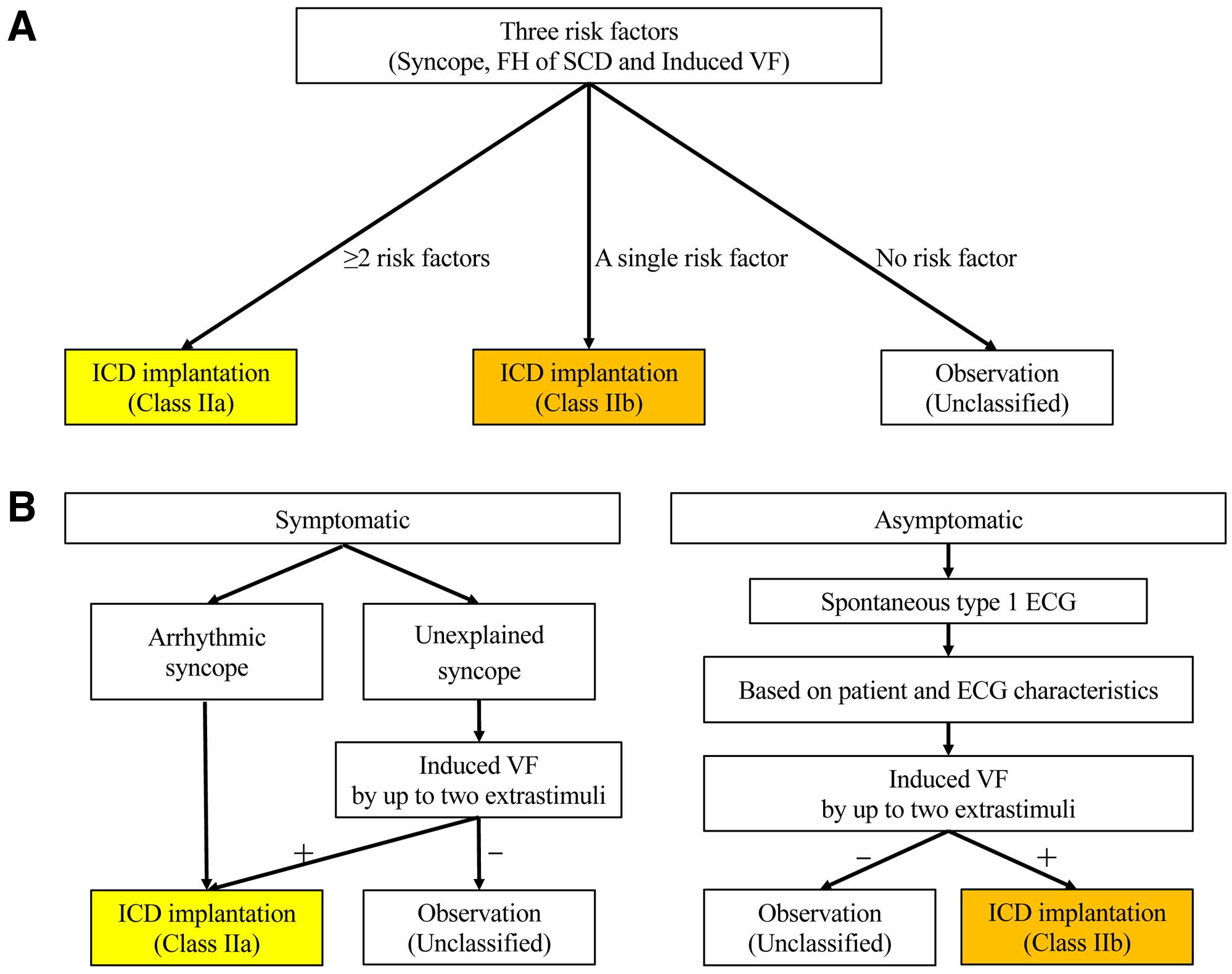
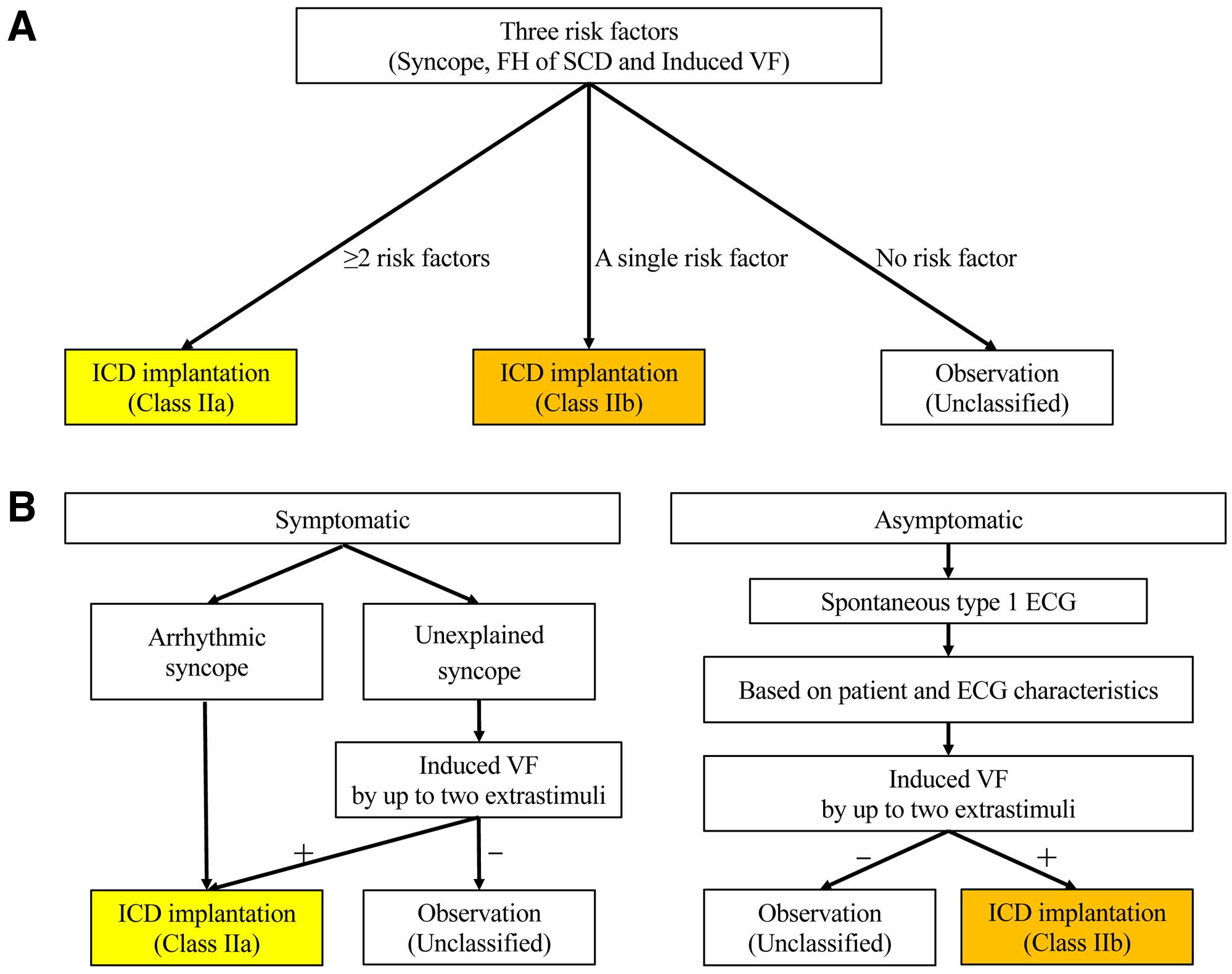
The former guideline (FG) recommended an implantable cardioverter-defibrillator (ICD) for primary prevention of SCD in patients with BrS based on the presence of 3 risk factors of equal importance: syncope, inducibility of VF by programmed electrical stimulation (PES), and family history of SCD.7
Implantation of an ICD was categorized as a Class IIa indication for patients with ≥2 risk factors and as Class IIb indication for patients with a single risk factor. The NG places more emphasis on previous arrhythmic syncope and inducibility of VF by ≤2 extrastimuli in PES for risk stratification.
The purpose of this study was to evaluate the usefulness of the NG and compare it with the FG for risk stratification of patients with BrS.
Methods
Study Population
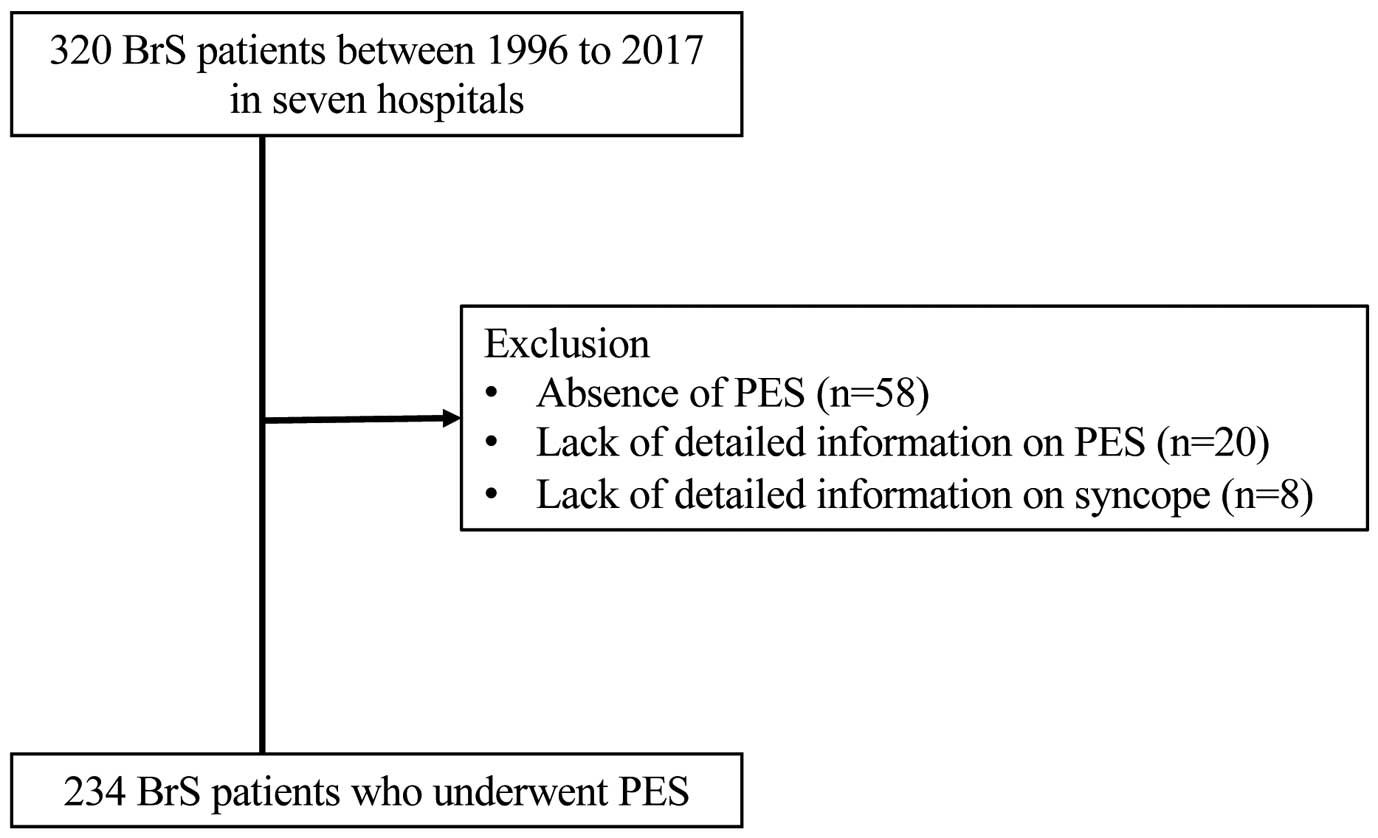
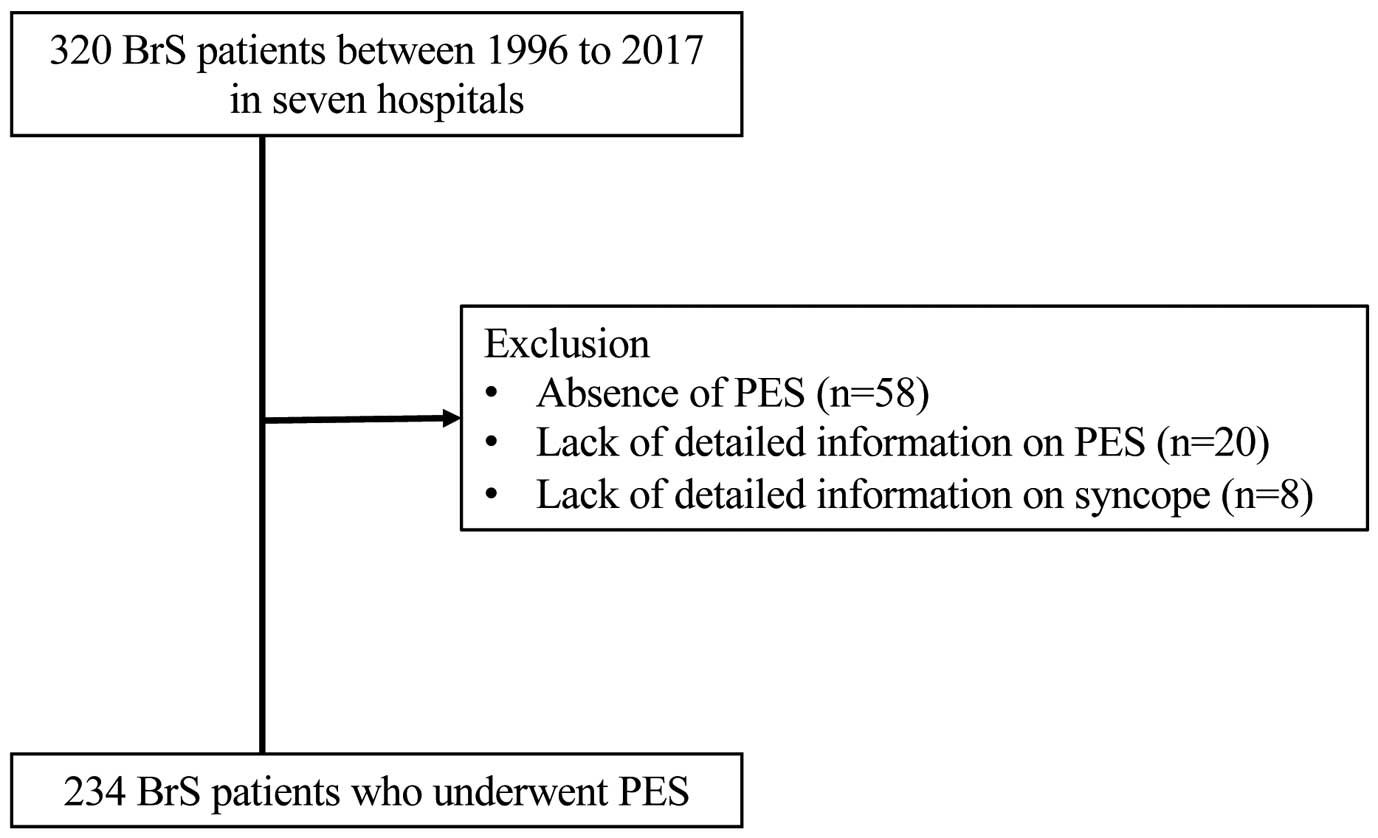
This study included 234 of 320 patients diagnosed with BrS between 1996 and 2017 in 7 hospitals in Japan. All patients underwent PES to evaluate the suitability of ICD implantation. None of the patients had structural heart disease. The 86 patients excluded from this study either did not undergo PES (n=58) or lacked detailed information on PES (n=20) and syncope (n=8) (Figure 1). This study was approved by the institutional research board of each participating hospital (M22-031-5).
BrS was diagnosed by the presence of type 1 ST-segment elevation, occurring spontaneously or after intravenous administration of a sodium channel blocker in ≥1 right precordial lead (V1
and V2), which was placed in a standard or superior position (up to the 2nd intercostal space).8
Type 1 ECG was defined as a coved-type J-point or ST elevation ≥0.2 mV, followed by a negative T wave.9
Drug provocation tests were conducted using pilsicainide (1 mg/kg body weight injected at a rate of 5–10 mg/min) or disopyramide (1.5 mg/kg; rate: 10 mg/min) during standard and high intercostal (2nd and 3rd) ECG recordings. All ECGs were recorded at 25 mm/s and 10 mm/mV. Following independent analyses of the ECG recordings by 2 cardiologists (W.A. and T.K.), a consensus was reached on the diagnosis for each patient.
Clinical Data
Clinical data, including age at diagnosis, sex, family history of SCD, and prognosis, were collected for all patients. We evaluated the ICD indications according to the former and NGs in all patients (Figure 2A,B). Arrhythmic events were defined as documented VF by conventional ECG, SCD, or appropriate shock delivery by an ICD. The follow-up period commenced at the time of diagnosis of BrS. The diagnosis of arrhythmic syncope was reached when syncope occurred with sudden onset without prodromes, without triggers for reflex or situational syncope, or when syncope was associated with nocturnal agonal respiration, seizure, or urinary incontinence.10
Syncope likely due to reflex syncope or orthostatic hypotension was regarded as non-arrhythmic syncope. It was associated with ≥1 typical prodrome and ≥1 trigger. Prodromes were nausea, vomiting, pallor, or yawning. Typical triggers were emotional distress, prolonged standing, or being in a crowded or hot place. Syncope was classified as unexplained when the physician faced difficulty in distinguishing between arrhythmic and non-arrhythmic syncope.
PES was performed at the right ventricular apex and outflow tract. Unless ventricular arrhythmia was induced or the ventricular effective refractory period was reached, 1–3 extrastimuli were used with a minimal coupling interval of 180–200 ms. Inducibility was defined as the provocation of VF requiring cardioversion to terminate the arrhythmia by ≤3 extrastimuli in the FG, and by ≤2 extrastimuli in the NG.
Patients were followed up every 3–6 months for clinical review and device interrogation. Clinical profile, ECG characteristics, and recurrence of VF during the follow-up period (i.e., 6.9±5.2 years) were investigated.
Statistical Analysis
Data were analyzed using the Stata/SE 14.0 for MAC (StataCorp LP, College Station, TX, USA). Numeric values are presented as mean±standard deviation, and categorical variables are presented as percentages. Statistical significance was determined using the chi-squared test or Student’s t-test, as appropriate. Survival curves were constructed using the Kaplan-Meier method and compared using the log-rank test. Cardiac events were tested by means of receiver operating characteristic curves and calculation of the area under the curve (AUC). P<0.05 denoted a statistically significant difference between groups.
Results
Clinical Profile of the Study Population
The clinical characteristics of the patients are shown in
Table. The majority were male. At diagnosis, 46 patients (20%) had previous VF, 100 patients (43%) had previous syncope (24 patients with arrhythmic syncope, 4 patients with reflex syncope, and 10 patients with syncope due to orthostatic hypotension), and 88 patients (37%) were asymptomatic. All patients underwent PES, and VF was induced in 158 patients (68%). Of the 76 patients with a family history of SCD, 30 (13%) had a family history of SCD at <45 years of age in a 1st- or 2nd-degree relative. An ICD was implanted in 175 patients (75%).
Table.
Baseline Characteristics of the BrS Patients
| Patient characteristics (n=234) |
| Age (years) |
44.9±13.4 |
| Male, n (%) |
226 (96%) |
| Follow-up period (years) |
6.9±5.2 |
| Previous VF, n (%) |
46 (20%) |
| Previous syncope, n (%) |
100 (43%) |
| Arrhythmic, n (%) |
24 (24%) |
| Unexplained, n (%) |
62 (62%) |
| Reflex syncope or orthostatic hypotension |
14 (14%) |
| Asymptomatic, n (%) |
88 (37%) |
| Spontaneous type 1 ECG, n (%) |
174 (74%) |
| Family history of SCD, n (%) |
76 (32%) |
| Induction of VF by PES, n (%) |
158 (68%) |
| Single, n (%) |
10 (6%) |
| Double, n (%) |
87 (55%) |
| Triple, n (%) |
61 (39%) |
| ICD implantation, n (%) |
175 (75%) |
| Primary prevention, n (%) |
131 (75%) |
| Secondary prevention, n (%) |
44 (25%) |
BrS, Brugada syndrome; ICD, implantable cardioverter defibrillator; PES, programmed electrical stimulation; SCD, sudden cardiac death; VF, ventricular fibrillation.
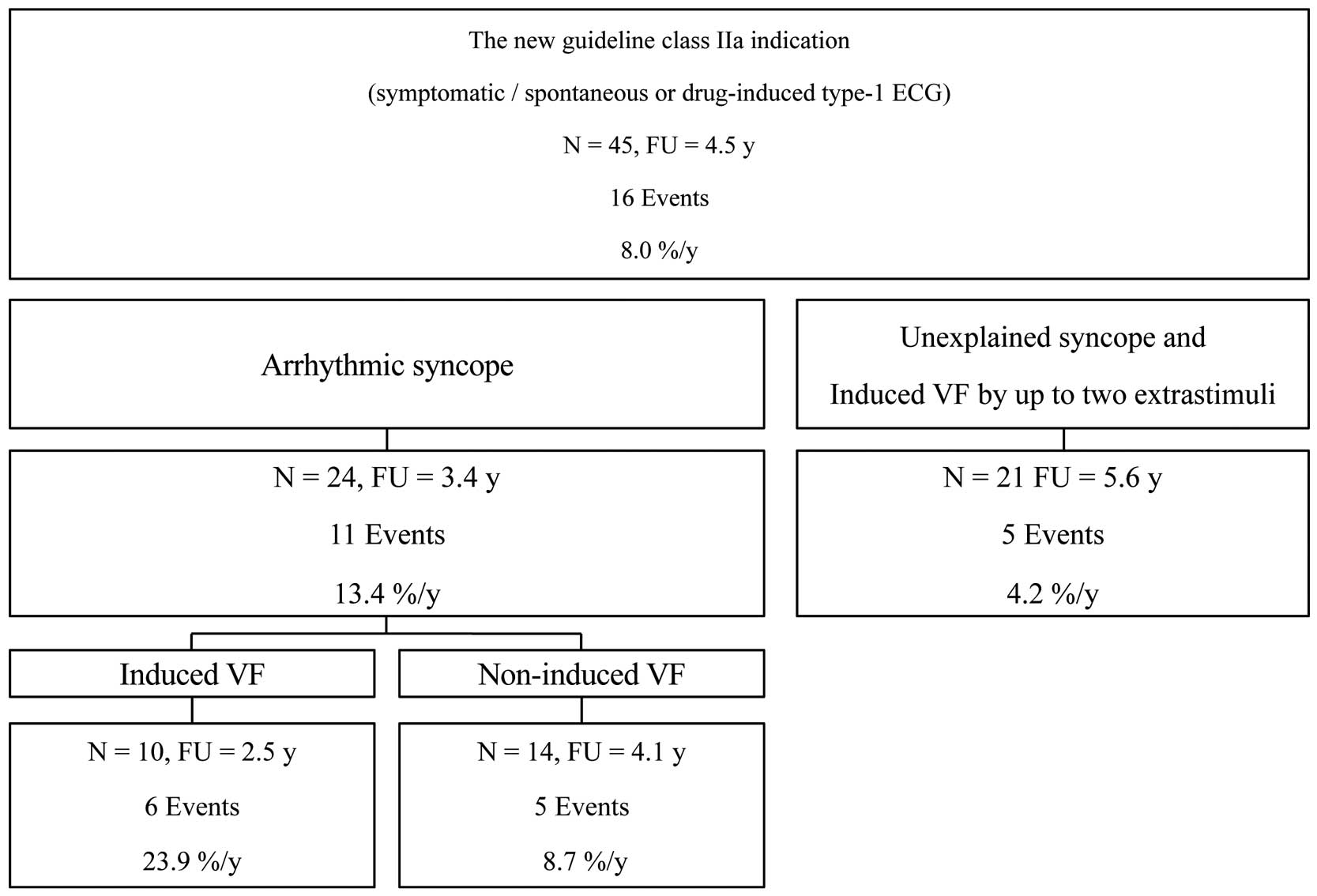
Of the 188 patients without previous VF, 104 and 74 met the Class IIa and IIb indications, respectively, for ICD implantation in the FG, whereas in the NG, 45 and 36 patients met the Class IIa and IIb indications, respectively, (Figures 3–5). The remaining patients were unclassified (10 patients [4%] for the FG and 107 patients [45%] for the NG). Of the104 patients with a Class IIa indication in the FG, 21 were Class IIb indication and 44 were unclassified in the NG (Figure 3). Among the 14 patients with non-arrhythmic syncope, 4 were classified as Class IIb indication and the remaining 10 were unclassified in the NG.


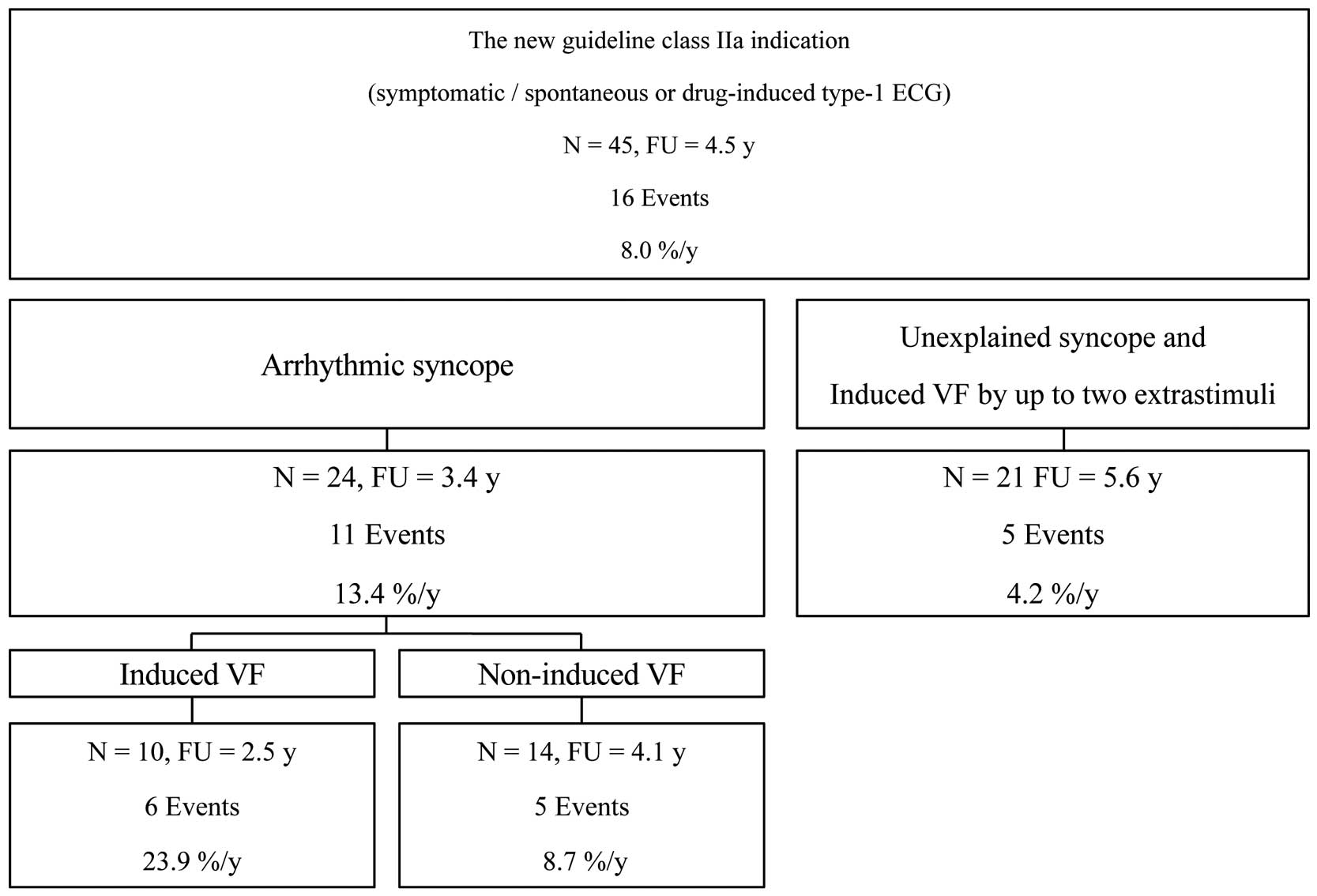
During the follow-up period (mean: 6.9±5.2 years), 220 patients (96%) were reviewed without administration of antiarrhythmic drugs; 10 patients were treated with bepridil, cilostazol, quinidine, or amiodarone after the initial VF attack; 4 patients without previous VF were treated with bepridil, cilostazol, quinidine, or disopyramide for prophylaxis against VF. A total of 42 patients (18%) experienced VF. There were no patient deaths reported during the follow-up period. Of the 46 patients with previous VF, 24 (52%) had recurrence. Under the criteria of the FG, 16 of the 104 patients (15.4%) with Class IIa indication and 2 of the 74 patients (2.7%) with Class IIb indication experienced VF (Figure 4A,B). The incidence of cardiac events per year was 3.0% and 0.4%, respectively (Figure 6). Under the criteria of the NG, 16 of the 45 patients (35.6%) with Class IIa indication and none of the 36 patients (0%) with Class IIb indication had VF (Figure 5). The incidence of cardiac events per year was 8.0% and 0.0%, respectively (Figure 6). Among 188 BrS patients without previous VF, receiver-operating characteristic curve analysis for the prediction of VF occurrence within 5 years showed that a Class IIa indication in the NG had higher sensitivity and specificity for predicting future VF than in the FG (sensitivity 92.3% vs. 92.3%; specificity 81.8% vs. 50.0%; AUC 0.87 vs. 0.71; 95% confidence interval 0.79–0.96 vs. 0.62–0.80, respectively; P<0.01) (Supplementary Figure). Of the 62 patients with unexplained syncope, 21 met the Class IIa indication in the NG based on inducible VF by ≤2 extrastimuli during PES. The incidence of VF was significantly higher in patients with inducible VF than in those without (Figure 7).

However, of the 107 patients without an indication for an ICD in the NG, 2 (1.9%) experienced VF. They met the Class IIb indication in the FG. One patient was an asymptomatic 53-year-old male with spontaneous type 1 ECG who had positive PES with VF induced by 3 extrastimuli from the right ventricular apex, and no family history of SCD. The other patient was a 38-year-old male with drug-induced type 1 ECG who had previous unexplained syncope, negative PES, and no family history of SCD. Both patients showed no QRS fragmentation in the right precordial leads and J waves in the inferolateral leads.
Discussion
Main Findings
The new JCS guideline places more emphasis on a history of arrhythmic syncope and VF induction by PES for risk stratification of BrS patients without previous VF. Currently, there are no data available regarding the validity of the new JCS guideline. The present study investigated the usefulness of the NG and showed that it could more accurately identify high-risk patients than the FG.
Risk Stratification of BrS Patients Without Previous VF
The annual risk of developing VF is approximately 2–6% in BrS patients with previous syncope and 0.3–0.5% in asymptomatic patients.3,4,11,12
Although the risk of developing VF in BrS patients without previous VF is low to moderate compared with that reported in patients with previous VF, a sophisticated method for risk stratification of these patients is lacking.
The former JCS guideline (published in 2012) recommended implantation of an ICD for primary prevention of SCD in patients with BrS according to the presence of ≥2 risk factors (i.e., syncope, VF induced by PES, and family history of SCD).7
The FG treated these 3 risk factors equally. This method of risk stratification was validated by Okamura et al13
and Delise et al.14
The etiology of syncope was not discriminated in the FG. However, the importance of detailed history taking related to syncope and inducibility of VF by fewer extrastimuli during PES was emphasized in the following years.10,15–19
In addition, a family history of SCD was demonstrated to have limited value in risk stratification.4,20–22
In the new Heart Rhythm Society, European Heart Rhythm Association, and Asia Pacific Heart Rhythm Society expert consensus statement published in 2016, implantation of an ICD is reasonable (Class IIa) in patients with presumably arrhythmic syncope and may be considered (Class IIb) in asymptomatic patients with inducible VF by ≤2 extrastimuli during PES. Although the new JCS guideline is consistent with the new consensus statement, it adds a Class IIa indication for patients with unexplained syncope and inducible VF by ≤2 extrastimuli during PES.
Significance of the New JCS Guideline
This study revealed that patients classified as Class IIa in the NG had a higher incidence of VF than those classified as Class IIa in the FG, which indicates that the NG more accurately identifies high-risk patients than the FG. In addition, none of the patients classified as Class IIb experienced VF. As expected, among patients with a Class IIa indication in the NG, the incidence of VF was high in patients with previous syncope presumably of arrhythmic origin.10,15–18
However, distinguishing between malignant and benign syncope remains a great challenge. It has been reported that reflex syncope occurs in 35% of patients with BrS.23
In addition, approximately 20% of BrS patients with VF experience prodromes prior to the onset of VF.10
Clinical features are not specific enough to distinguish between arrhythmic and non-arrhythmic syncope. Regarding this point, the NG proposes PES for risk stratification of patients with unexplained syncope. This study showed that the incidence of VF was not negligible in these populations and that PES could accurately stratify the risk, which validated the usefulness of the NG.
However, compared with the FG, the number of patients in whom the indication for an ICD was not allocated was higher in the NG. Among the study patients, 2 experienced VF during the follow-up period. VF was not induced by ≤2 extrastimuli in them. Although the rate of events was low, more sophisticated methods are needed to identify high-risk patients for VF among asymptomatic BrS patients.
Study Limitations
First, this study was restricted to patients with BrS who underwent PES and thus we may have included only high-risk patients. Second, the relatively small number of arrhythmic events during follow-up in asymptomatic patients limited the analysis in terms of identifying risk factors. Third, patients with BrS are linked to a lifelong risk of arrhythmias, and the follow-up period of 6.9 years may have been insufficient to fully evaluate the prognosis, especially for asymptomatic patients. Although none of the 36 patients with a Class IIb indication in the NG had VF events in this study, they have a risk of developing VF. Fourth, we may have underestimated the rate of cardiac events because the endpoint for patients without an ICD was based on symptoms or conventional ECG. Therefore, asymptomatic cardiac events during sleep may have been missed. Fifth, the incidence of unexplained syncope was higher than in previous studies,17,18
which might be because this study included only patients who underwent PES. Selection bias may limit the interpretation of the results. Prospective, multicenter studies including larger numbers of patients with BrS are warranted to confirm our findings.
Conclusions
The new JCS guideline more accurately identifies high-risk patients with BrS than the former guideline. This study validated the usefulness of the new JCS guideline for risk stratification in patients with BrS.
Disclosures
The authors have no disclosures or conflicts of interest to declare.
Funding
This work was supported by the Japan Society for the Promotion of Science (JSPS) through a Grant-in-Aid for Scientific Research (KAKENHI Grant no. JP17K09545), and the Suzuken Memorial Foundation.
Supplementary Files
Please find supplementary file(s);
http://dx.doi.org/10.1253/circj.CJ-19-0910
References
- 1.
Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome. J Am Coll Cardiol 1992; 20: 1391–1396.
- 2.
Takagi M, Aonuma K, Sekiguchi Y, Yokoyama Y, Aihara N, Hiraoka M, et al. The prognostic value of early repolarization (J wave) and ST-segment morphology after J wave in Brugada syndrome: Multicenter study in Japan. Heart Rhythm 2013; 10: 533–539.
- 3.
Kamakura S, Ohe T, Nakazawa K, Aizawa Y, Shimizu A, Horie M, et al. Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1–V3. Circ Arrhythm Electrophysiol 2009; 2: 495–503.
- 4.
Probst V, Veltmann C, Eckardt L, Meregalli PG, Gaita F, Tan HL, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation 2010; 121: 635–643.
- 5.
Adler A, Rosso R, Chorin E, Havakuk O, Antzelevitch C, Viskin S. Risk stratification in Brugada syndrome: Clinical characteristics, electrocardiographic parameters, and auxiliary testing. Heart Rhythm 2016; 13: 299–310.
- 6.
JCS Joint Working Group. Guidelines for diagnosis and management of inherited arrhythmias (JCS 2017). Tokyo: JCS, 2018; 1–79.
- 7.
JCS Joint Working Group. Guidelines for diagnosis and management of patients with long QT syndrome and Brugada syndrome (JCS 2012). Tokyo: JCS, 2012; 1–49.
- 8.
Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 2015; 36: 2793–2867.
- 9.
Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, et al. Brugada syndrome: Report of the second consensus conference: Endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 2005; 111: 659–670.
- 10.
Olde Nordkamp LR, Vink AS, Wilde AA, de Lange FJ, de Jong JS, Wieling W, et al. Syncope in Brugada syndrome: Prevalence, clinical significance, and clues from history taking to distinguish arrhythmic from nonarrhythmic causes. Heart Rhythm 2015; 12: 367–375.
- 11.
Priori SG, Gasparini M, Napolitano C, Della Bella P, Ottonelli AG, Sassone B, et al. Risk stratification in Brugada syndrome: Results of the PRELUDE (PRogrammed ELectrical stimUlation preDictive valuE) registry. J Am Coll Cardiol 2012; 59: 37–45.
- 12.
Casado-Arroyo R, Berne P, Rao JY, Rodriguez-Manero M, Levinstein M, Conte G, et al. Long-term trends in newly diagnosed Brugada syndrome: Implications for risk stratification. J Am Coll Cardiol 2016; 68: 614–623.
- 13.
Okamura H, Kamakura T, Morita H, Tokioka K, Nakajima I, Wada M, et al. Risk stratification in patients with Brugada syndrome without previous cardiac arrest: Prognostic value of combined risk factors. Circ J 2015; 79: 310–317.
- 14.
Delise P, Allocca G, Marras E, Giustetto C, Gaita F, Sciarra L, et al. Risk stratification in individuals with the Brugada type 1 ECG pattern without previous cardiac arrest: Usefulness of a combined clinical and electrophysiologic approach. Eur Heart J 2011; 32: 169–176.
- 15.
Makimoto H, Kamakura S, Aihara N, Noda T, Nakajima I, Yokoyama T, et al. Clinical impact of the number of extrastimuli in programmed electrical stimulation in patients with Brugada type 1 electrocardiogram. Heart Rhythm 2012; 9: 242–248.
- 16.
Sroubek J, Probst V, Mazzanti A, Delise P, Hevia JC, Ohkubo K, et al. Programmed ventricular stimulation for risk stratification in the Brugada syndrome: A pooled analysis. Circulation 2016; 133: 622–630.
- 17.
Take Y, Morita H, Toh N, Nishii N, Nagase S, Nakamura K, et al. Identification of high-risk syncope related to ventricular fibrillation in patients with Brugada syndrome. Heart Rhythm 2012; 9: 752–759.
- 18.
Sacher F, Arsac F, Wilton SB, Derval N, Denis A, de Guillebon M, et al. Syncope in Brugada syndrome patients: Prevalence, characteristics, and outcome. Heart Rhythm 2012; 9: 1272–1279.
- 19.
Antzelevitch C, Yan GX, Ackerman MJ, Borggrefe M, Corrado D, Guo J, et al. J-Wave syndromes expert consensus conference report: Emerging concepts and gaps in knowledge. J Arrhythm 2016; 32: 315–339.
- 20.
Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Giordano U, et al. Natural history of Brugada syndrome: Insights for risk stratification and management. Circulation 2002; 105: 1342–1347.
- 21.
Eckardt L, Probst V, Smits JP, Bahr ES, Wolpert C, Schimpf R, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation 2005; 111: 257–263.
- 22.
Gehi AK, Duong TD, Metz LD, Gomes JA, Mehta D. Risk stratification of individuals with the Brugada electrocardiogram: A meta-analysis. J Cardiovasc Electrophysiol 2006; 17: 577–583.
- 23.
Yokokawa M, Okamura H, Noda T, Satomi K, Suyama K, Kurita T, et al. Neurally mediated syncope as a cause of syncope in patients with Brugada electrocardiogram. J Cardiovasc Electrophysiol 2010; 21: 186–192.