- J-STAGE home
- /
- Circulation Reports
- /
- Volume 2 (2020) Issue 1
- /
- Article overview
- /
- Full view
-
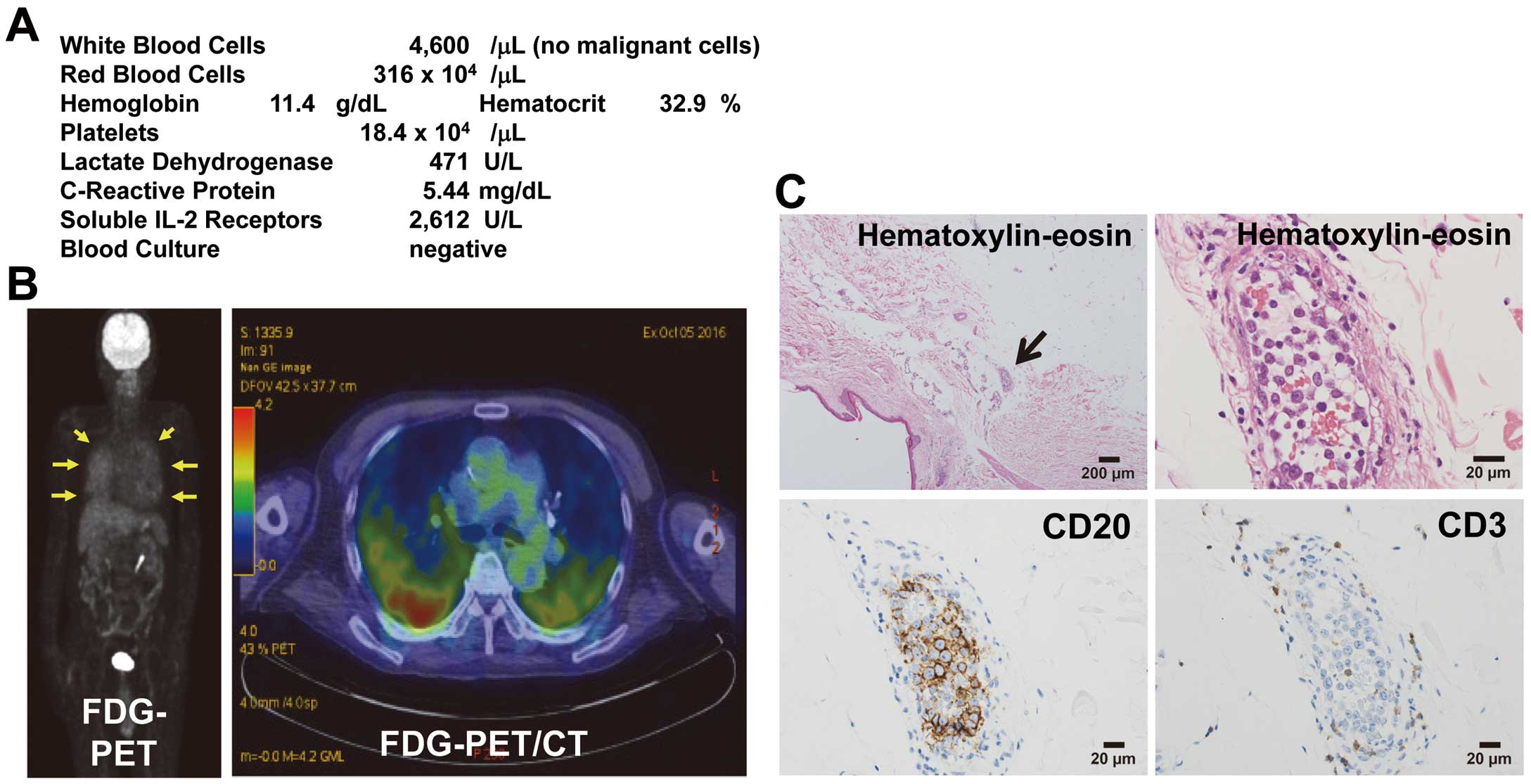
Hisashi Kai
Department of Cardiology, Kurume University Medical Center [Japan]
-
Hitoshi Hamamura
Department of Cardiology, Kurume University Medical Center [Japan]
-
Hiroshi Niiyama
Department of Cardiology, Kurume University Medical Center [Japan]
-
Atsushi Katoh
Department of Cardiology, Kurume University Medical Center [Japan]
-
Fumihiko Mouri
Division of Hematology and Oncology, Department of Medicine, Kurume University School of Medicine [Japan]
-
Koji Nagafuji
Division of Hematology and Oncology, Department of Medicine, Kurume University School of Medicine [Japan]
-
Koichi Ohshima
Department of Pathology, Kurume University School of Medicine [Japan]
-
Rin Yamaguchi
Department of Pathology and Laboratory Medicine, Kurume University Medical Center [Japan]
-
Kei Mukohara
Department of General and Family Medicine, Kurume University Medical Center [Japan]
2020 Volume 2 Issue 1 Pages 69-70
- Published: January 10, 2020 Received: November 17, 2019 Released on J-STAGE: January 10, 2020 Accepted: November 18, 2019 Advance online publication: December 12, 2019 Revised: -
(compatible with EndNote, Reference Manager, ProCite, RefWorks)
(compatible with BibDesk, LaTeX)