2019 Volume 66 Issue 5 Pages 475-483
2019 Volume 66 Issue 5 Pages 475-483
We studied cytological specimens of conventional papillary thyroid carcinoma (PTC), follicular variant papillary thyroid carcinoma (FVPTC), and noninvasive follicular thyroid tumor with papillary-like nuclear features (NIFTP) (formerly noninvasive FVPTC) to identify useful cytological parameters for their differentiation. Cytological findings of invasive FVPTC and NIFTP were very similar to each other but differed from those of conventional PTC. Intranuclear cytoplasmic inclusions, true papillary cell clusters, monolayered cell sheets, ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background were the observed characteristic features of conventional PTC. Microfollicular cell clusters and dense globules of colloids were characteristic features of invasive FVPTC and NIFTP. Scoring the eight parameters (intranuclear cytoplasmic inclusions, nuclear grooves, powdery chromatin, true papillary cell clusters, ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background) readily distinguished NIFTP from conventional PTC, but could not distinguish NIFTP from invasive FVPTC. The average total score of NIFTP, invasive FVPTC, and conventional PTC were 2.60 ± 0.55, 2.63 ± 0.62, and 4.57 ± 0.99, respectively. The difference between conventional PTC and NIFTP or invasive FVPTC was statistically significant (p < 0.001, Student’s t-test). Individuals with more than three of the identified parameters likely harbor conventional PTC, rather than NIFTP. In this way, 87.5% (112/128) of conventional PTCs could be differentiated from NIFTP, and definitively diagnosed as malignant by cytology.
NONINVASIVE FOLLICULAR VARIANT PAPILLARY THYROID CARCINOMA (FVPTC), recently renamed noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTPs), is considered an indolent thyroid tumor because of its better clinical course relative to conventional papillary thyroid carcinoma (PTC) [1-5]. This renaming has had a huge impact on the histological and cytological diagnosis of PTC. In particular, the proportion of FVPTC may be decreased in the histological diagnosis of PTC, which may decrease the risk of malignancy in the Thyroid Bethesda System [6]. Furthermore, this may increase the rate of false-positive diagnoses in thyroid cytology. The cytological characteristics of NIFTP and invasive FVPTC are nearly indistinguishable [7-11]. Therefore, it is important to distinguish conventional PTC from both NIFTP and invasive FVPTC by fine-needle aspiration cytology (FNAC).
We previously reported that conventional PTC can be distinguished from FVPTC and NIFTP based on the cytological findings of cell clusters and smear backgrounds, rather than nuclei [12]. However, only a few cases with NIFTP and FVPTC were included in the previous study. More information from NIFTP and FVPTC cases are needed to confirm this finding.
In this study, we included 206 patients with NIFTP, FVPTC, and conventional PTC, compared their cytological characteristics, and devised a cytological scoring system to differentiate conventional PTC from FVPTC, including NIFTP.
To investigate the cytological features of FVPTC, including NIFTP and conventional PTC, we reviewed the cytological smears of 60 patients with conventional PTC, five with invasive FVPTC, and two with NIFTP. All cases were histologically confirmed after undergoing surgical procedures in Aichi Cancer Centre Hospital, Nagoya, Japan. Additionally, we also reviewed the cytological smears of 68 patients with conventional PTC, 38 with invasive FVPTC, and 33 with NIFTP, which were also histologically confirmed after surgical procedures in Kuma Hospital, Kobe, Japan. Overall, samples from 128 patients with conventional PTC, 43 with invasive FVPTC, and 35 with NIFTP were used in this study. NIFTP cases are diagnosed histologically according to Nikiforov’s criteria [1, 2]. We did not conduct gene analysis.
Of the 128 patients with conventional PTC, 99 were women and 29 were men. Their ages ranged from 14 to 84 years (mean, 54.1 years). The 43 patients with invasive FVPTC comprised 35 women and eight men. Their ages ranged from 30 to 80 years (mean, 60.3 years). There were 35 patients with NIFTP (23 women, 12 men; 28 to 79 years of age, mean age, 58.6 years).
Cytological specimens in Aichi Cancer Center Hospital were stained using both Papanicolaou and Diff-Quik methods, and those in Kuma Hospital were stained only using the Papanicolaou method. All smears were used for the assessment of cytological findings. We microscopically evaluated the cytological specimens of 128 patients with conventional PTC, 43 with invasive FVPTC, and 35 with NIFTP for the presence of 11 representative cytological characteristics: nuclear inclusions, nuclear grooves, powdery chromatin, true papillary cell clusters, monolayered cell sheets, microfollicular cell clusters, dense globules of colloids, ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background. Nuclear inclusions, nuclear grooves, and powdery chromatin are the most important cytological characteristics of PTC. Also important in the definitive diagnosis of PTC are the appearance of cell clusters and smear background [5, 13-17].
SPSS version 23 for Windows (SPSS Inc., Chicago, IL., USA) was used for statistical analysis.
Nuclear findingsNuclear inclusions (intranuclear cytoplasmic inclusions) are one of the most typical cytological characteristics of PTC. True nuclear inclusions contain cytoplasmic content and are surrounded by aggregated chromatin. Nuclear pseudo-inclusions without cytoplasmic content cannot be considered. Nuclear grooves are also typical cytological features of PTC, but are not specific and are not useful if their numbers are small. Cells showing at least two grooves per nucleus were therefore considered positive for this study, and cells with only one groove per nucleus were not. Powdery chromatin, an important characteristic of PTC, refers to very fine, watery nuclear chromatin in cytological smears, identical to Orphan Annie eye nuclei in histology.
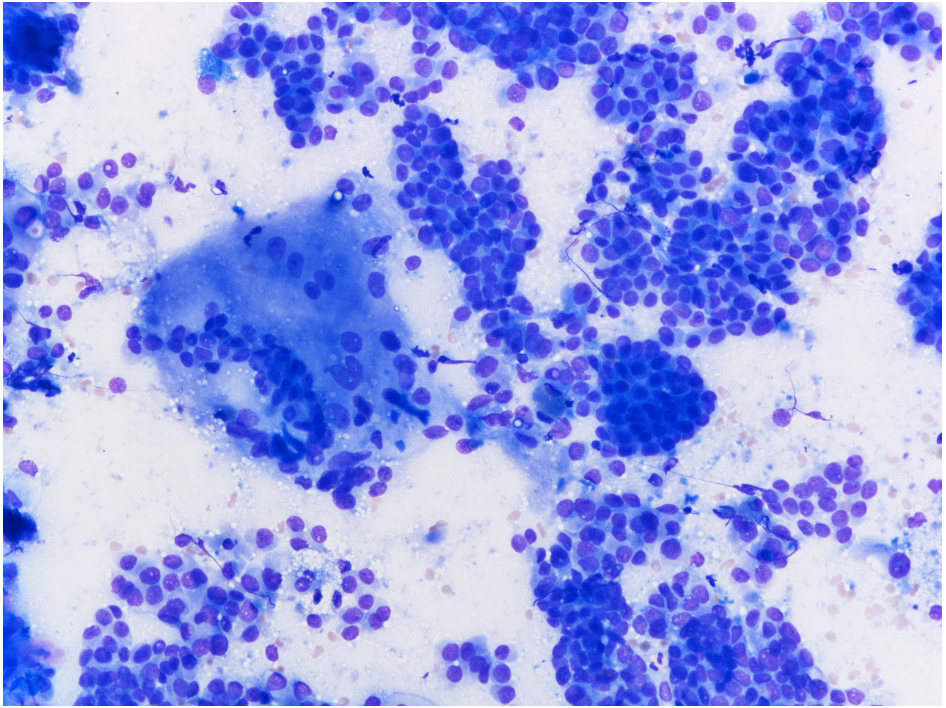
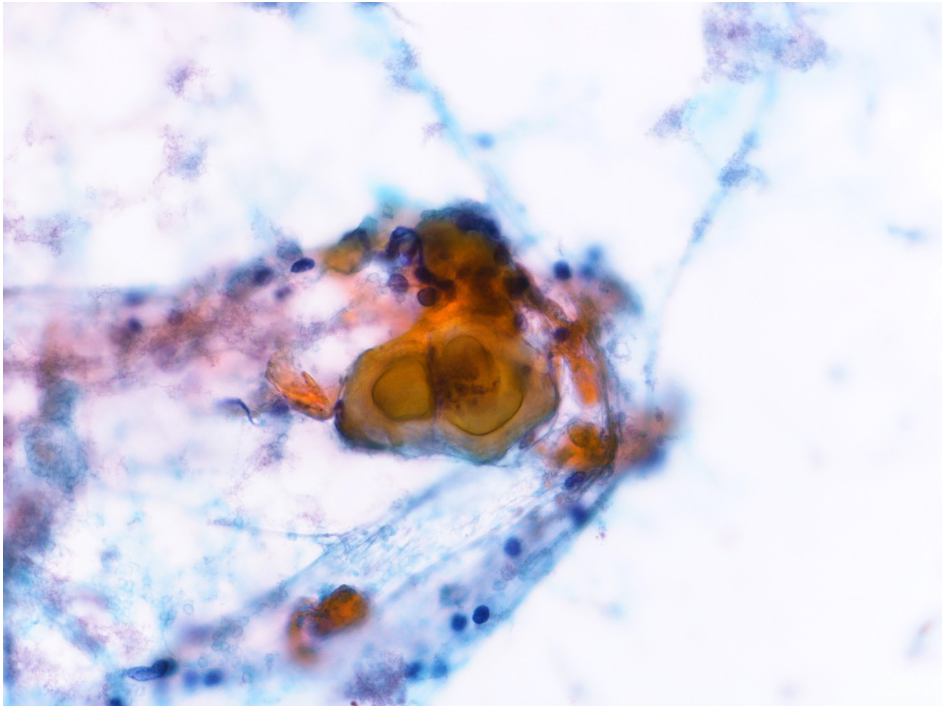
Cell clustersPapillary cell clusters are the most essential signs of PTC. Papillary clusters with a fibrovascular core (Fig. 1) are true papillary cell clusters. Those without a fibrovascular core are pseudo-papillary cell clusters. They are often difficult to distinguish from syncytial aggregates of microfollicular cell clusters and are not counted. Papillary fibrovascular stroma (Fig. 2) is another distinctive characteristic and often forms a fingerlike radial structure. Although fibrovascular stroma is also seen in FVPTC and NIFTP as well as follicular neoplasm, it appears as a meshwork rather than a papillary or radial structure. Monolayered cell sheets are the most frequent cell clusters in PTC smears. They are flat single-layer cell clusters without nuclear overlap. Microfollicular cell clusters are seen in some PTC smears, especially FVPTC. They are not characteristic signs of conventional PTC. Nuclei are arranged like small circles in microfollicular clusters. Microfollicular clusters appear as either single cells or syncytial aggregates. Syncytial aggregates of microfollicular cells sometimes form large clusters with or without meshwork-like fibrovascular stroma. They look like papillary cell clusters and are sometimes difficult to distinguish. In cases where it was not clear whether the cell cluster is microfollicular or papillary, it was not included in the analysis.
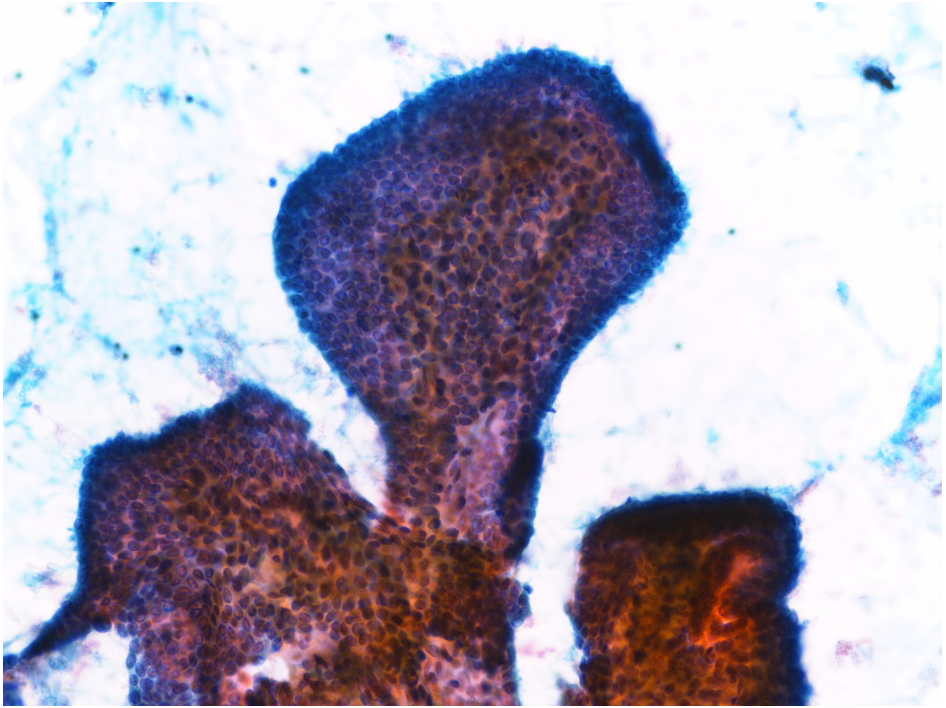
True papillary cluster of conventional papillary thyroid carcinoma. Papanicolaou staining, ×20 magnification
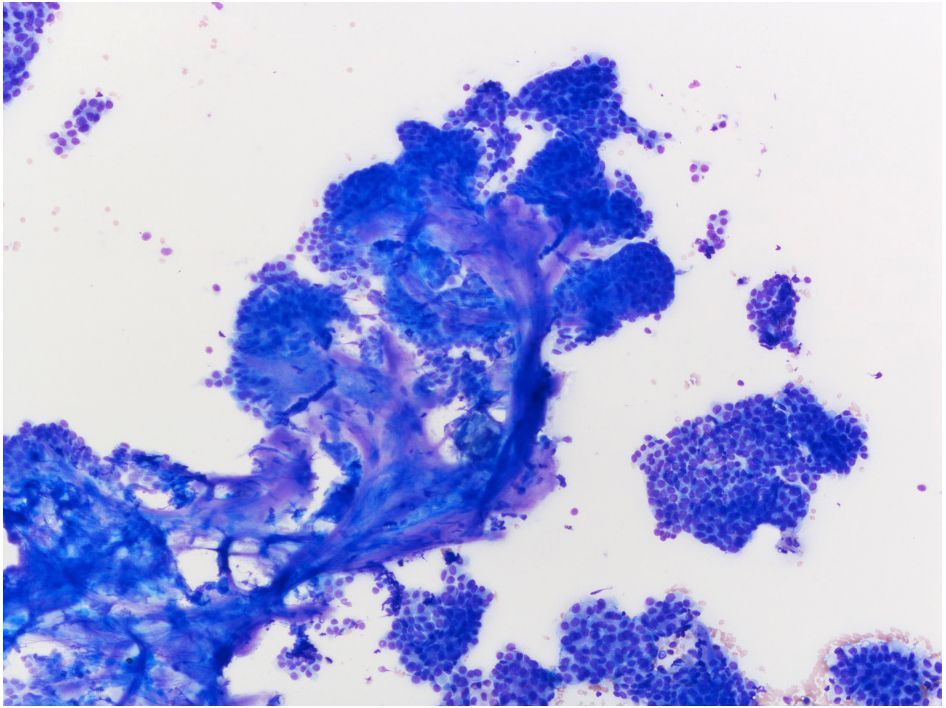
True papillary clusters with fingerlike radial stroma of conventional papillary thyroid carcinoma. Diff-Quik staining, ×10 magnification
Dense globules of colloids (Fig. 3) are round or oval-shaped condensed colloids. They are usually seen in the smear background but are sometimes visible in the center of microfollicular cell clusters. Ropy colloids (also termed chewing gum colloids) (Fig. 4) are long stretched colloids. Multinucleate giant cells (Fig. 5) are histiocytic giant cells. They are sometimes confused with multinucleate foamy macrophages. These cell types can be distinguished because the cytoplasm of multinucleate giant cells is smooth and homogeneous, not foamy as in foamy macrophages. Psammoma bodies (Fig. 6) are concentric calcified bodies and are highly suggestive of PTC, but they are not frequently observed in individuals with PTC. Some patients with PTC develop degenerative cystic changes. Many foamy macrophages are seen in the background.
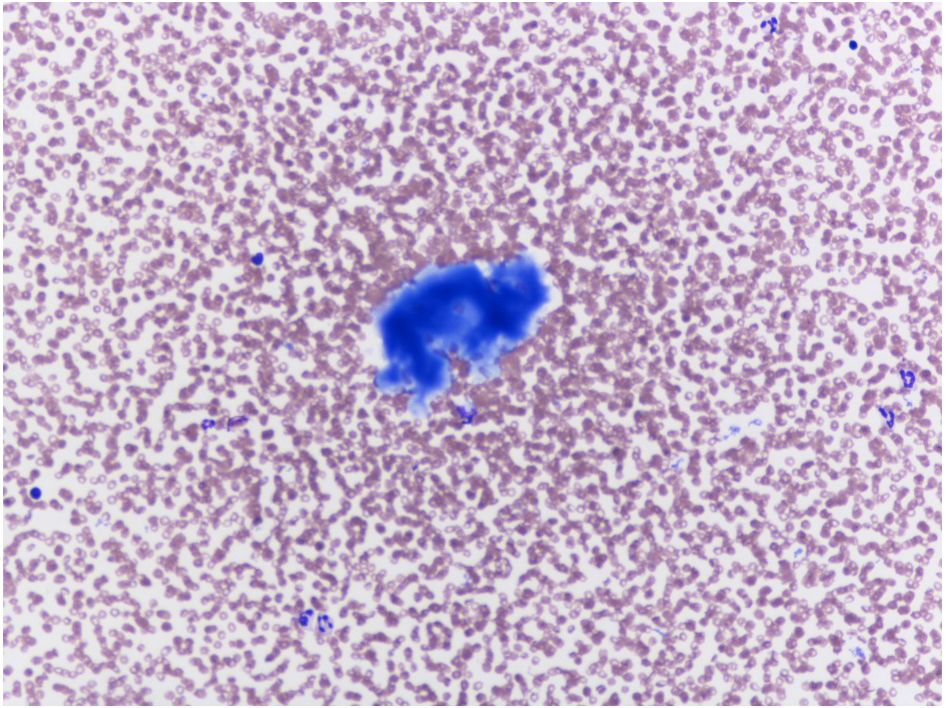
A dense globule of colloids of follicular variant papillary thyroid carcinoma. Diff-Quik staining, ×20 magnification
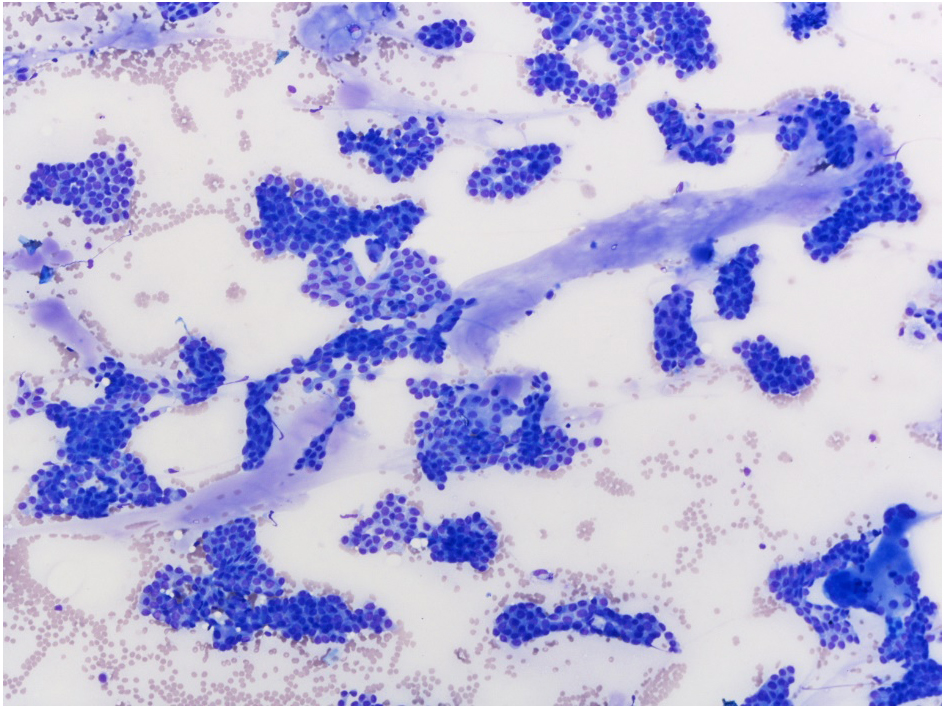
Ropy colloids, so-called chewing gum-like colloids, between tumor cells of conventional papillary thyroid carcinoma. Diff-Quik staining, ×10 magnification
A multinucleate giant cell (left center) of conventional papillary thyroid carcinoma. Diff-Quik staining, ×20 magnification
Psammoma bodies of conventional papillary thyroid carcinoma. Papanicolaou staining, ×40 magnification
The results of routine cytological diagnosis based on the Thyroid Bethesda System [6] are shown in Table 1. Of 128 patients with conventional PTC, 122 (95%) were diagnosed with malignant PTC. Twenty-one (49%) of 43 patients with invasive FVPTC and 23 (66%) of 35 patients with NIFTP were diagnosed with malignant PTC. These results suggest that there were many false positive diagnoses as NIFTP in our routine cytodiagnosis practice.
| Diagnostic category according to the Thyroid Bethesda System | NIFTP | Invasive FVPTC | Conventional PTC |
|---|---|---|---|
| Malignant | 23 | 21 | 122 |
| SFM | 3 | 7 | 5 |
| FN/SFN | 3 | 0 | 0 |
| AUS/FLUS | 5 | 11 | 1 |
| Benign | 1 | 3 | 0 |
| Unsatisfactory | 0 | 1 | 0 |
| Total Cases | 35 | 43 | 128 |
SFM, Suspicious for malignancy; FN/SFN, Follicular neoplasm or suspicious for follicular neoplasm; AUS/FLUS, Atypia of undetermined significance or follicular lesion of undetermined significance
Nuclear findings, including nuclear inclusions, nuclear grooves, and powdery chromatin, were frequently seen in conventional PTC, as were true papillary cell clusters and monolayered sheets of tumor cells. Microfollicular cell clusters were not frequently seen in conventional PTC. Background features, such as ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background, were more frequently seen in conventional PTC than in NIFTP or FVPTC.
FNAC smears of FVPTC were primarily composed of microfollicular cell clusters with or without dense globules of colloids, which were very similar to a follicular neoplasm at low-power view [5, 13-17]. At high-power view, however, nuclear inclusions, nuclear grooves, and powdery chromatin were recognized. While nuclear grooves and powdery chromatin were more frequently seen, nuclear inclusions were less frequent and were observed in 65% of patients with invasive FVPTC.
The cytological findings of NIFTP, formerly noninvasive FVPTC, were similar to those of invasive FVPTC. No obvious cytological differences were observed between them. Thus, it may be very difficult or impossible to distinguish the difference between NIFTP and invasive FVPTC through FNAC.
Cytological characteristics of NIFTP, invasive FVPTC, and conventional PTC are shown in Table 2. The frequency of these 11 cytological characteristics was very similar between NIFTP and invasive FVPTC. No significant differences were apparent by the Pearson’s chi-square test (Table 2). Regarding conventional PTC, with the exception of nuclear grooves and powdery chromatin, the frequency of these characteristics was different from that of NIFTP and invasive FVPTC (Table 2).
| Cytological Findings | NIFTP | Invasive FVPTC | Conventional PTC | Chi-square test* | Chi-square test** |
|---|---|---|---|---|---|
| Nuclear inclusions | 63% (22/35) | 65% (28/43) | 93% (119/128) | p = 0.836 | p < 0.001 |
| Nuclear grooves | 100% (35/35) | 93% (40/43) | 100% (128/128) | p = 0.111 | ND |
| Powdery chromatin | 97% (34/35) | 98% (42/43) | 99% (127/128) | p = 0.883 | p = 0.322 |
| Papillary cell clusters | 0% (0/35) | 0% (0/43) | 62% (79/128) | ND | p < 0.001 |
| Monolayered cell sheets | 57% (20/35) | 40% (17/43) | 100% (128/128) | p = 0.121 | p < 0.001 |
| Microfollicular cell clusters | 100% (35/35) | 100% (43/43) | 46% (59/128) | ND | p < 0.001 |
| Dense globules of colloids | 86% (30/35) | 79% (34/43) | 41% (53/128) | p = 0.447 | p < 0.001 |
| Ropy colloids | 0% (0/35) | 0% (0/43) | 29% (37/128) | ND | p < 0.001 |
| Multinucleate giant cells | 0% (0/35) | 2% (1/43) | 48% (62/128) | p = 0.364 | p < 0.001 |
| Psammoma bodies | 0% (0/35) | 0% (0/43) | 8% (10/128) | ND | p = 0.088 |
| Cystic background | 0% (0/35) | 5% (2/43) | 18% (23/128) | p = 0.196 | p = 0.007 |
*, NIFTP vs. invasive FVPTC; **, NIFTP vs. conventional PTC; ND, Not detected
About nuclear findings, the frequency of nuclear inclusions was different between conventional PTC and NIFTP or invasive FVPTC. They were more frequently seen among patients with conventional PTC (100%) than among those with invasive FVPTC (65%) or NIFTP (63%). The differences were considered significant by Pearson’s chi-square test (p < 0.001, Table 2). In contrast, the frequency of nuclear grooves and powdery chromatin were almost identical among these three groups. The differences between conventional PTC and NIFTP or FVPTC were not considered significant (ND and p = 0.322, respectively; Table 2).
Concerning cell clusters, true papillary cell clusters were seen in more than half of patients with conventional PTC, but not seen in those with NIFTP or invasive FVPTC. The difference was considered significant (p < 0.001, Table 2). Monolayered cell sheets were seen in all patients with conventional PTCs but were less frequent among those with NIFTP (57%) and invasive FVPTC (40%). The difference was considered significant (p < 0.001, Table 2). By contrast, microfollicular cell clusters were more frequent among patients with NIFTP (100%) and invasive FVPTC (100%) than among those with conventional PTC (46%). The difference was considered significant (p < 0.001, Table 2). Therefore, true papillary cell clusters and monolayered cell sheets are characteristic features of conventional PTC, whereas microfollicular cell clusters are characteristic features of NIFTP or invasive FVPTC.
As regards smear background, ropy colloids and multinucleate giant cells, psammoma bodies, and cystic background were more frequently seen among patients with conventional PTCs than among those with NIFTP or invasive FVPTC. The differences, except for psammoma bodies, were considered significant (p < 0.001, p < 0.001, and p = 0.007, respectively; Table 2). Although psammoma bodies were not significant statistically (p = 0.088, Table 2), they were still considered a useful finding for conventional PTC because they were not observed in patients with NIFTP and invasive FVPTC. By contrast, dense globules of colloids were more frequently seen in patients with NIFTP or invasive FVPTC than in those with conventional PTC. The difference was considered significant (p < 0.001, Table 2). Accordingly, ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background, as well as psammoma bodies, are characteristics of conventional PTC, and dense globules of colloids is a characteristic of NIFTP or invasive FVPTC.
NIFTP and invasive FVPTC show very similar cytological features. The two cannot be clearly distinguished by cytological findings. Conventional PTC, however, shows different cytological features, especially in terms of cell clusters and smear background, from NIFTP and invasive FVPTC.
The 2nd edition monograph of the Thyroid Bethesda System recommends that a definitive malignant diagnosis of PTC should be reserved in patients who present, in addition to other characteristics, at least one of the following features: papillary architecture, psammoma bodies, and intranuclear inclusions [5]. Thus, we evaluated the presence of these parameters. The results are shown in Table 3. Approximately 98% (126/128) of patients with conventional PTC and 63% (22/35) of those with NIFTP had at least one of these parameters. However, two or three parameters were seen only in patients with conventional PTC, and none in those with NIFTP. Therefore, approximately 58% (74/128) of conventional PTC patients with two or three parameters can be diagnosed as malignant PTC, not NIFTP.
| Nuclear inclusions True papillary clusters Psammoma bodies |
NIFTP | Invasive FVPTC | Conventional PTC |
|---|---|---|---|
| Three of three findings | 6% (8/128) | ||
| Two of three findings | 52% (66/128) | ||
| One of three findings | 63% (22/35) | 65% (28/43) | 41% (52/128) |
| None of three findings | 37% (13/35) | 35% (15/43) | 2% (2/128) |
To semi-quantitatively distinguish NIFTP from conventional PTC, we examined the scoring of their cytological characteristics. The following eight cytological characteristics were used as the parameters for calculation: nuclear inclusions, nuclear grooves, powdery chromatin, true papillary clusters, ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background (Table 4). The presence of these parameters was counted as one point (per parameter). Three of these characteristics concerning nuclei (nuclear inclusions, nuclear grooves, and powdery chromatin) are important for PTC diagnosis. Five of these findings about cell clusters and smear background (true papillary clusters, ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background), were observed in patients with conventional PTC, but not in patients with NIFTP, and so are considered important parameters to distinguish conventional PTC from NIFTP.
| Cytological parameters | Score |
|---|---|
| (1) Nuclear inclusions | 1 |
| (2) Nuclear grooves | 1 |
| (3) Powdery chromatin | 1 |
| (4) True papillary cell clusters | 1 |
| (5) Ropy colloids | 1 |
| (6) Multinucleate giant cells | 1 |
| (7) Psammoma bodies | 1 |
| (8) Cystic background | 1 |
The scores of these eight parameters are shown in Table 5. All patients with NIFTP showed a total score of three or less. By contrast, 87.5% (112/128) of patients with conventional PTC showed a total score of more than three. The average total score of NIFTP, invasive FVPTC, and conventional PTC were 2.60 ± 0.55, 2.63 ± 0.62, and 4.57 ± 0.99, respectively. The difference between conventional PTC and NIFTP or invasive FVPTC was statistically significant (p < 0.001 by Student’s t-test). If the cut-off value of the difference between NIFTP and conventional PTC was more than three points, the sensitivity was 87.5% (112/128) and the specificity was 100% (35/35). A total score of more than three meant that more than three of the eight parameters were detected in a single patient. This would allow cytologists to easily make a definitive diagnosis even in routine cytodiagnosis practice by determining the number of parameters present. By this method, NIFTP can be clearly distinguished from conventional PTC.
| Total Score | NIFTP | Invasive FVPTC | Conventional PTC |
|---|---|---|---|
| 7 | 2% (3/128) | ||
| 6 | 13% (17/128) | ||
| 5 | 38% (48/128) | ||
| 4 | 2% (1/43) | 34% (44/128) | |
| 3 | 63% (22/35) | 63% (27/43) | 11% (14/128) |
| 2 | 34% (12/35) | 30% (13/43) | 2% (2/128) |
| 1 | 3% (1/35) | 5% (2/43) | |
| Average | 2.60 ± 0.55 | 2.63 ± 0.62 | 4.57 ± 0.99 |
Sensitivity for conventinal PTC: 87.5% (112/128), cut-off by score 3
FVPTC is the most common subtype of PTC [18]. The prevalence of FVPTC among PTC cases has varied considerably between studies. There is a tendency toward higher prevalence in Western countries and lower prevalence in Asian countries. The prevalence of NIFTP in Western countries was reported to be 10–30% of all PTCs, while those in Asian countries were average 4.0% (range: 2.2%–9.8%) of all PTCs [7, 19]. The largest study in Japan on FVPTC and NIFTP was conducted in Kuma Hospital [7]; a prevalence of 2.8% for FVPTC and 0.8% for NIFTP was reported. Differences of NIFTP prevalence between Western countries and Asian countries are considered partly due to results of differences in morphological diagnostic criteria for NIFTP [7, 20].
The nuclear features of invasive FVPTC and NIFTP are not as obvious as in conventional PTC [5, 8, 21] and hence are not always sufficient for identification of malignancy by cytology. Therefore, some invasive FVPTCs and NIFTPs are not classified as malignant [22-25]. Such cases are classified as indeterminate Thyroid Bethesda System categories of atypia of undetermined significance or follicular lesion of undetermined significance, follicular neoplasm or suspected follicular neoplasm, or suspicious for malignancy. A considerable number of NIFTPs and invasive FVPTCs, however, were classified as malignant in our study (Table 1). Regarding NIFTP, 23 (66%) of 35 patients were diagnosed as having malignancy. Renaming of noninvasive FVPTC to NIFTP resulted in more false-positive diagnoses of these cases. Thus, the differentiation of conventional PTC from NIFTP and FVPTC is crucial in the cytological diagnosis of PTC.
The cytological characteristics of NIFTP are nearly the same as those of invasive FVPTC. No distinguishing characteristics of noninvasive FVPTC are known at present [7-11]. However, another study suggested that the cytological findings of NIFTP differ from those of FVPTC [22]. In addition, according to our previous study [12], nuclear inclusions of NIFTP were less frequent than invasive FVPTC. Our previous study only included a few patients with NIFTP and invasive FVPTC, which limited the strength of the results. Hence, in this study, we added 71 patients with NIFTP and invasive FVPTC, examined their nuclear findings, confirmed that the nuclear findings were very similar, and that there was nearly no difference between NIFTP and invasive FVPTC.
Cytological discrimination between NIFTP and invasive FVPTC may be very difficult or impossible. Some studies reported that there are no reliable cytological features that distinguish NIFTP from invasive FVPTC [7-11]. Therefore, patients with possible NIFTP or invasive FVPTC should be differentiated from those with conventional PTC and excluded from malignant diagnosis. To prevent overtreatment, cytologists should not include potential NIFTP cases into the malignant category and should limit this category to conventional PTC. The 2nd edition Thyroid Bethesda System recommended that cases with potential NIFTP should be classified under follicular neoplasm category.
The Thyroid Bethesda System also recommends papillary architecture, psammoma bodies, and intranuclear inclusions as cytological parameters of PTC [5]. Especially, true papillae and psammoma type calcification were described as exclusion criteria for histological diagnosis of NIFTP [2, 20]. These parameters can help distinguish NIFTP from conventional PTC to some extent. Using these parameters, 58% (74/128) of conventional PTCs were definitively diagnosed as malignant (Table 3). However, this result is not sufficient, because more than 40% of conventional PTCs were diagnosed as indeterminate. Therefore, we have add other 5 parameters for clear differentiation in this study and obtained results that 87.5% of conventional PTCs were definitely diagnosed as malignant. Our results are better than the differential method recommended by the Thyroid Bethesda System (87.5% vs. 58%).
About distinguishing conventional PTC from NIFTP, we previously reported that cytological findings other than the nuclear features would be useful markers [12]. In this study, we focused on five non-nuclear features, which were observed in conventional PTC, but not in NIFTP, in addition to three nuclear features. For this reason, we used a total of eight parameters to differentiate conventional PTC from invasive FVPTC or NIFTP. Three nuclear features alone cannot differentiate between conventional PTC and invasive FVPTC or NIFTP. By contrast, they were clearly distinguished using these eight parameters; and 87.5% of conventional PTCs could be diagnosed as malignant.
Ultrasonography is effective at differentiating NIFTP and invasive FVPTC [7, 26]. By ultrasonography, NIFTP appears as a well-demarcated benign-looking nodule, while invasive FVPTC appears as a vague nodule with an indistinct border because of the associated invasion. Therefore, it is important for cytologists to refer to the ultrasound findings when making a cytological diagnosis. Clinicians are also able to prevent overtreatment by considering not only cytological diagnosis but also ultrasound findings. Higuchi M, et al. [27] reported that active surveillance (follow-up without surgical resection) is an acceptable option for thyroid nodules having favorable benign clinical findings or benign part of the low-risk group.
Gene analysis is also useful for discrimination of NIFTP from invasive FVPTC. NIFTP is related to RAS gene mutation, like follicular adenoma and carcinoma. In contrast, BRAF V600E mutation is related to invasive FVPTC and conventional PTC [5, 28]. Therefore, RAS and BRAF gene analysis may help in the differential diagnosis between NIFTP and invasive FVPTC. We did not conduct gene analysis in this study and therefore, cannot comment on how many cases with RAS or BRAF mutation were included in our NIFTP cases.
To date, there is no reliable method to distinguish NIFTP from invasive FVPTC by cytology. Consequently, it is better to not classify FVPTC cases into the malignant category to avoid false-positive diagnosis.
In this study, cytological differences among NIFTP, invasive FVPTC, and conventional PTC were studied, and a method for differentiating NIFTP and invasive FVPTC from conventional PTC was devised. To make the discrimination easier, we propose a simple scoring method using the following eight parameters: nuclear inclusions, nuclear grooves, powdery chromatin, true papillary cell clusters, ropy colloids, multinucleate giant cells, psammoma bodies, and cystic background. Using these parameters, NIFTP and invasive FVPTC can be clearly distinguished from conventional PTC. Cases with more than three of the eight parameters are almost always conventional PTC, and never NIFTP. On the contrary, cases with three or less than three of the eight parameters might indicate possible NIFTP, and should not be classified as malignant, to avoid a false-positive diagnosis, as well as overtreatment.
We would like to thank Editage (www.editage.jp) for English language editing.
The authors declare that they have no conflicts of interest.