2023 Volume 70 Issue 5 Pages 459-464
2023 Volume 70 Issue 5 Pages 459-464
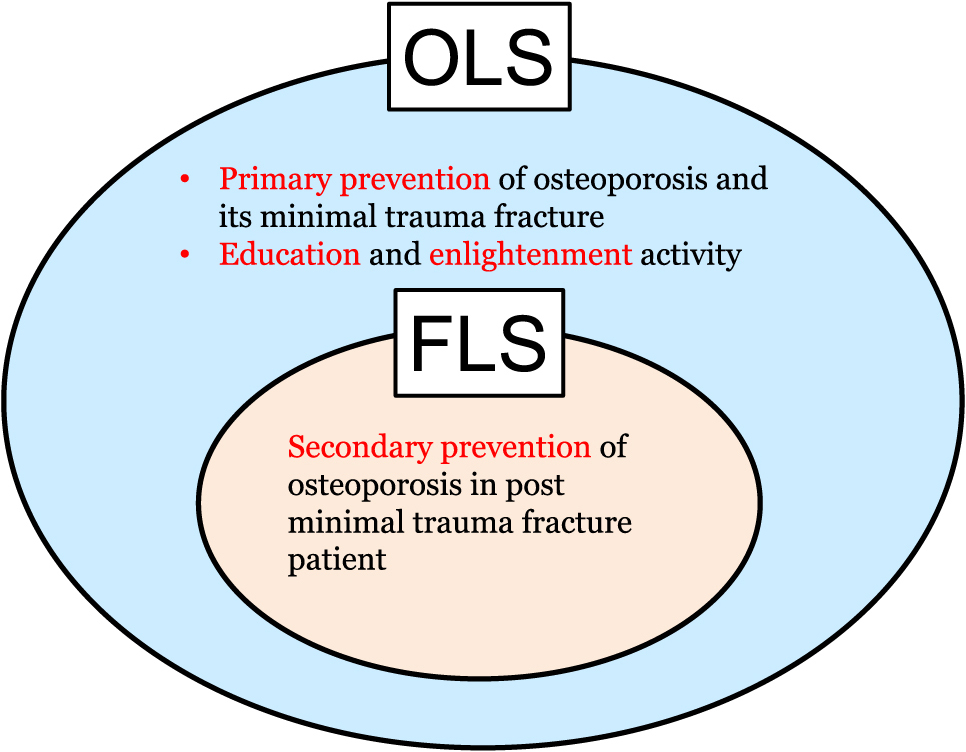
The prevalence of osteoporosis has increased in super-aging societies. To prevent subsequent fractures from occurring after initial osteoporotic fracture, coordinator-based systems called fracture liaison service (FLS) have been implemented worldwide. In Japan, the osteoporosis liaison service (OLS) including FLS was launched in 2011 in order to reduce the incidence of both primary and secondary fractures in osteoporosis patients. Multidisciplinary management by an OLS coordinator aims to support patient care, monitor medicine adherence, and improve quality of life of the elderly. A framework such as OLS-7 has been proposed to provide comprehensive support regardless of the expertise of each medical staff.
Osteoporosis has become more common in super-aging societies such as Japan, affecting one in three women and one in five men over the age of 50 worldwide [1-3]. Fragility fracture resulting from osteoporosis impairs quality of life (QOL) and activity of daily living (ADL) in elderly patients [4], and an initial fracture is known to be a major risk factor for subsequent new ones [5]. However, the implementation rate of secondary fracture prevention is low, hence secondary fracture prevention programs led by coordinators were started in Europe in the late 1990s [6, 7]. This program called fracture liaison service (FLS) has been reported to reduce fragility fractures and improve the survival rate of post-fracture patients [8-11]. In Japan, Japan Osteoporosis Society (JOS) launched an osteoporosis liaison service (OLS) program including FLS in order to solve the clinical problems related to osteoporosis treatment, education, and enlightenment (Fig. 1) [12].
Concept of Fracture Liaison Service (FLS) and Osteoporosis Liaison Service (OLS)
When JOS started their OLS in 2011, the medical staff members who were in charge of OLS activity were certified as OLS coordinators by JOS [12]. In FLS in other countries, the medical staff to support the program are mainly nurses who are called liaison nurses. As OLS covers not only post-fracture care but also the enlightenment and education of osteoporosis, the OLS coordinators consist of several types of healthcare professionals including nurses [13] (Table 1). Candidate OLS coordinators should be medical staff who are engaged in medical, healthcare, and educational practices at hospitals, clinics, nursing care facilities, academic institutions, or governmental agencies. The OLS coordinator certification is given to those who have enrolled in a specific lecture course and passed a qualification test. A total of 3,450 people have been certified as OLS coordinators as of March 2022, and of these 51% were nurses, 19% pharmacists, 16% physical therapists, 6% radiological technologists, 3% registered dietitians, 2% occupational therapists, and 3% were others [13].
| Public health nurse |
| Midwife |
| Nurse |
| Radiological technologist |
| Medical technologist |
| Physical therapist |
| Occupational therapist |
| Clinical engineer |
| Speech-language-hearing therapist |
| Pharmacist |
| Registered dietitian |
| Certified social worker |
| Certified care worker |
| Mental health social worker |
| Certified orthoptist |
OLS: osteoporosis liaison service
OLS coordinators consist of a variety of health care professionals each of which belong to their own specialized field. The International Osteoporosis Foundation offers a Best Practice Framework (BPF) to identify what kind of activity is necessary in an FLS institution by its Capture-the-FractureTM program [14] (Table 2). The BPF promotes a coordinator-based FLS model of care and aims to set a benchmark for FLS with an eye to improving the available services. Structured as a series of 13 standards, the BPF addresses elements that are essential to FLS. Each standard gives criteria and targets that are broken down into three levels of achievement: gold, silver, and bronze. FLS contains a “5I” model of identification, investigation, information, intervention, integration [15]. As OLS covers not only secondary prevention but also primary prevention of osteoporotic fracture, 7 elements for OLS services by health care professionals, called as OLS-7, was tentatively proposed [16] (Table 3). The level of each element had three levels: basic, standard, and expert. Basic level is for the non-specialist and offers minimal services. Standard level is for the medical staff who are not specialized in each field and provides necessary information of guidance in each element. Expert level is for healthcare professionals specialized in each field and offers ideal services with quantitative indicators if applicable.
| 1. | Patient identification |
| 2. | Patient evaluation |
| 3. | Post-fracture assessment timing |
| 4. | Vertebral fracture |
| 5. | Assessment guidelines |
| 6. | Secondary cause of osteoporosis |
| 7. | Falls prevention services |
| 8. | Multifaceted health and lifestyle risk factor assessment |
| 9. | Medical initiation |
| 10. | Medication review |
| 11. | Communication strategy |
| 12. | Long-term management |
| 13. | Database |
| Elements | Level 1 (Expert) | Level 2 (Standard) | Level 3 (Basic) | |
|---|---|---|---|---|
| 1 | Fracture risk assessment | • FRAXTM and other risk assessment tool | • Height, body weight, age, family history, and past history • Check decreased height • (if female) FOSTA |
• Check decreased height • (if female) FOSTA |
| 2 | Prevalent fracture and other causes of secondary osteoporosis | • Check the history of prevalent fracture and (if exists) fracture site • Check the history to exclude the comorbidities or medication which cause secondary osteoporosis |
• Check the history of prevalent fracture and (if exists) fracture site • Medication review to look for cause of secondary osteoporosis (especially for glucocorticoid) |
• Check the history of prevalent fracture and (if exists) fracture site |
| 3 | Nutrition | • Registered nutritionist or nutritional support team assesses nutritional status with guidance on nutrition | • Check decreased appetite which results in frailty • General nutritional education by non-specialist |
• Check decreased appetite which results in frailty |
| 4 | Fall risk and exercise | • Fall risk assessment and prevention program • Physical activity is quantified by medical staff (e.g., grip strength, single leg standing time). • Education for exercise by specialist |
• Fall risk assessment and education • Education for exercise by non-specialist |
• Check the history of fall during last year |
| 5 | Medication review and guidance | • Pharmacist checks leftover medicine, double dose, and medication adherence, and provides medication guidance. | • Non-pharmacist check leftover medicine, double dose and medication adherence | • Confirm medication adherence |
| 6 | QOL and ADL | • Medical staff quantifies QOL and ADL by assessment tool such as JOQOL and SF-36TM. | • Medical staff assesses ADL and QOL with a tool such as checking sheet. | • Ask ADL and QOL to the patients and their families |
| 7 | Database | • Liaison service works under interactive medical cooperation with database | • Liaison service works under interactive medical cooperation. | • Patients are listed in each hospital |
FRAXTM: fracture risk assessment tool, FOSTA: Female Osteoporosis Self -Assessment Tool for Asia, QOL: quality of life, ADL: activity of daily living, JOQOL: Japanese Osteoporosis Quality of Life Questionnaire, SF-36TM: Short-Form 36-Item Health Survey.
Although bone mineral density (BMD) is necessary to diagnose osteoporosis except for the patients with hip or vertebral fracture [17], we cannot examine the BMD in all patients without prevalent fracture. The initial assessment of the risk of osteoporosis is decreased stature and low body mass index. As bone loss is age-dependent, a formula is available to calculate it for females using age and body weight (FOSTA, Female Osteoporosis Self-Assessment Tool for Asia) [18]. Family history of osteoporotic fracture is also a risk factor which reflects the genetic background of bone health. Fracture assessment tools such as FRAXTM are popular indicators to assess future risk of fracture in both major osteoporotic fracture and hip fracture [19].
Prevalent osteoporotic fracture and other causes of osteoporosisAgain, prevalent osteoporotic fracture is very important to assess the future risk of subsequent fracture. In addition, the fracture site is necessary to diagnose primary osteoporosis, that is, the patients with hip or vertebral fracture are diagnosed as osteoporosis regardless of their BMD, but those with fractures at other sites are diagnosed when their BMD are below 80% of young adult mean [17]. In the elderly, co-existence of chronic diseases is common, and the medication for these conditions could affect bone health. In particular, persistent glucocorticoid (over 3 months) is a high risk factor for osteoporosis and more attention needs to be paid to treat glucocorticoid-induced osteoporosis [20]. Medication review is necessary especially when a patient visits multiple hospital or clinics. Furthermore, other causes of secondary osteoporosis such as endocrinological, nutritional, and genetic disorders need to be ruled out, and, if they should exist, the cause has to be treated as well as bone loss [21].
Nutritional assessment and educationAdequate nutrition, including appropriate calcium and vitamin D intake, are essential elements to maintain bone health and BMD [22]. In the elderly, poor food intake results in frailty and induces high fracture risk [23]. Therefore, assessment of food intake with sufficient amount of energy and protein intake is necessary. In addition to calcium and vitamin D, other nutrients and vitamins are also important for bone metabolism [24]. The nutritional assessment and guidance by a registered dietitian and/or nutritional support team encourages lifestyle changes (in particular balanced nutrient intake) and could contribute to the reduction of fracture risk.
Fall and physical activityMany osteoporotic fractures occur with falls, and the patient’s past history of falls is a major risk factor for the next fall. First of all, we should ask about the history of falls in daily life and assess the fracture risk using questionnaires [25]. Many patients with high fall risk have frailty, and appropriate physical therapy is important to keep up their physical activity and reduce their fall risk [26, 27]. Physical activity could be quantified by several tests such as grip strength, single-leg standing time, timed up-and-go test, which are included in part in guidelines for diagnosis of sarcopenia [28].
Medication review and guidance to maintain medication adherenceNowadays, there are several anti-osteoporotic medicines to reduce fragility fracture available, but the medication adherence and persistence rate is still lower than expected [6]. To obtain good efficacy of fracture prevention by medication, high adherence of as much as over 80% in bisphosphonate is necessary [29]. However, even after the surgical treatment of fracture, more than 50% of patients discontinue taking the medicine within 1 year after surgery [30, 31]. Therefore, continuous effort to maintain medication adherence by medical staff is necessary to reduce subsequent fracture. Some patients have leftover medicine and checking their stock of leftover medicine and receiving guidance by a pharmacist could help to emphasize the importance of medicine adherence to the patients.
QOL and ADLLife expectancy has been increasing in Japan’s super-aging society, but healthy life expectancy is still about 10 years shorter than life expectancy itself [32]. To achieve better QOL and ADL in the elderly, the assessment of these aspects is necessary in order to find out the problems in their daily life, which could contribute to setting up a plan of better care and assistance. To evaluate their QOL, quantitative assessment such as JOQOL (Japanese Osteoporosis Quality of Life Questionnaire) [33] and SF-36TM (Short-Form 36-Item Health Survey) [34, 35] could be effective. Close cooperation between hospitals, clinics, and nursing care facilities is also necessary to improve both QOL and ADL.
DatabaseThe prevalence of osteoporosis and its fracture increase exponentially along with age, and continuous support for these patients should be performed on database [6, 7, 14]. After the surgery for osteoporotic fracture, imminent risk of secondary fracture increases. Therefore, these patients should be registered to the database to set up an FLS program for them to prevent secondary fracture.
To achieve better longevity, bone health should be regarded as so essential as to extend OLS coverage to include both primary and secondary fracture prevention. Although there is a medical check-up system for osteoporosis provided by the local government in Japan, the rate of specific check-up for osteoporosis is very low, approximately 4.5% in 2020 [36]. Both education and awareness for the prevention of osteoporosis is not so popularly promoted as it could be, due to the lack of concern and misconceptions about osteoporosis. In addition, primary fracture prevention even in osteoporosis patients is not so cost-effective as secondary prevention, and the measurement of its efficacy in general population is challenging. In April 2022, the Japanese government started the reimbursement for prevention of secondary fracture by FLS in osteoporosis patients who had surgical treatment of hip fracture [37]. For this reimbursement, the patients must have assessment and treatment in a registered acute care hospital. In the case that an FLS program started in an acute care hospital, their continued patient care in a convalescence rehabilitation hospital and outpatient clinic can also be reimbursed. FLS program to prevent secondary fracture should be performed according to the national Guidelines for Prevention and Treatment of Osteoporosis (2015) [38] and the Japanese clinical standard for FLS [39].
The goal of OLS is to prevent the first fracture and stop the chain reaction of secondary fractures in osteoporosis patients. Multidisciplinary approach with OLS coordinators would contribute to support their lives and achieve better QOL and ADL in super-aging societies such as Japan.
AS has previously received consulting fees and lecture fees outside the submitted work from Amgen Inc., Asahi Kasei Pharma Corp., Daiichi Sankyo Co. Ltd., Eli Lilly Japan K.K., Kyowa Kirin Co. Ltd., Novo Nordisk Pharma Ltd., Sumitomo Pharma Co. Ltd., and Teijin Pharma Ltd. AS has also received research funding outside the submitted work from Chugai Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Taisho Pharmaceutical Co., Ltd., and Takeda Pharmaceutical Co., Ltd.