2020 年 37 巻 4 号 p. 111-115
2020 年 37 巻 4 号 p. 111-115
Anesthesiologists have routinely administered supplementary oxygen to prevent maternal hypoxemia and improve fetal oxygenation during cesarean delivery under spinal anesthesia. Some reports have indicated an increase in fetal free radicals due to prophylactic oxygen administration. The risk factors for hypoxemia during cesarean delivery still remain unclear. Therefore, in this retrospective study, we investigated the incidence of intraoperative hypoxemia and its associated risk factors in 155 patients receiving spinal anesthesia for cesarean delivery. Our study demonstrated that the incidence of intraoperative hypoxemia was high (32.3%) in patients receiving spinal anesthesia for cesarean in the absence of supplemental oxygen. It also indicated that spinal block levels higher than T3 or more were associated with intraoperative hypoxemia. Therefore, it is important to carefully observe parturients intraoperatively and prepare to promptly administer oxygen and other treatments if necessary.
Compared to general anesthesia, spinal anesthesia has been commonly performed for cesarean delivery since reduces the incidence of maternal mortality associated with airway complications [ 1]. Many studies have showed that supplementary oxygen improved fetal oxygen pressure from the 1980s to 1990s [ 2, 3]. Thus, many anesthesiologists have routinely administered supplementary oxygen to prevent maternal hypoxemia and to improve fetal oxygenation during cesarean delivery under spinal anesthesia. However, definite benefits of prophylactic oxygen administration have not been established [ 4]. Moreover, some reports have shown data of increased fetal free radicals by prophylactic oxygen administration [ 5]. Therefore, recently, many anesthesiologists have not been using prophylactic oxygen in elective cesarean delivery. But maternal hypoxemia has often found in ordinary clinical settings without prophylactic oxygen. In addition, the risk factors for hypoxemia during cesarean delivery are still not clear.
In this retrospective study, we investigated the incidences of hypoxemia and associated risk factors during cesarean delivery under spinal anesthesia.
This study was approved by Institutional Review Board Approval (Shimane University Institutional Committee, No.20170817-1). The subjects were patients who underwent elective cesarean delivery under spinal anesthesia at Shimane University Hospital from January 2015 to August 2017. Exclusion criteria were as follows; conversion to general anesthesia, prophylactic oxygen administration, use of intravenous sedative drugs (midazolam or propofol), or intravenous fentanyl. We reviewed anesthetic records retrospectively.
In this study, the primary outcome was all incidences of intraoperative hypoxemia events. The definition of hypoxemia is whenever SpO2 dropped below 90% or whenever there was a decrease of more than 5% compared to before anesthesia was performed. SpO2 was continuously recorded using saturation probe (Nellcor™ Oxisensor™Ⅲ, Covidien Co. Japan). And to determine the variables associated with intraoperative hypoxemia as secondary outcomes, we investigated as follows secondary outcomes included; patients’ characteristics (age (35 years or older), height, BMI (30 or more) and smoking history), the amount of blood loss, the presence of intrathecal (i.t.) fentanyl and morphine, intravenous pentazocine and the level of spinal anesthesia.
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics. 6 A p value of less than 0.05 was defined as statistical significance. For the secondary outcomes, an odds ratio (OR) with 95% confidence interval (CI) was calculated. Continuous variables were showed as mean ± standard deviation or median (interquartile range). Comparison was performed by unpaired t-test. Fisher's exact test were used to suggest the predictor variables. Since some data were not recorded for anesthetic levels and weight gain rate, and the defects were considered to be completely random defects that were not affected by other factors, statistical analyses associated with anesthetic levels were calculated after pairwise deletion.
The total number of cases during study period was 330. 15 cases were excluded because the anesthetic techniques were converted from spinal anesthesia to general anesthesia due to inadequate sensory block level or patients’ request. And 77 patients were administrated any sedative drugs or fentanyl. 83 patients were excluded from the analysis because of prophylactic oxygen administration for prevention of hypoxemia due to hypotension or sedative drugs at the discretion of each anesthesiologist. Finally, we actually analyzed 155 cases overall. ( Fig. 1) Hypoxemia as a primary outcome in this study was observed in 50 cases, which is equal to 32.3% of total cases. In these cases, there were 19 cases in which the SpO2 level dropped below 90%. And in 31 cases, SpO2 decreased more than 5% compared to before anesthesia was performed. As shown in Table 1, there were no significant differences about the patients’ ages, height, body mass index between hypoxemia group and no hypoxemia group. When we evaluated the risk factors for hypoxemia, some data of anesthetic level were deficient, the number about anesthetic level was 9 in the hypoxemia group and 15 in the non-hypoxemia group. The risk factors associated with hypoxemia detected in this study was anesthetic level (Th3 or more) after spinal anesthesia (OR = 2.50, 95% CI, 1.07–5.85; p = 0.026). As shown in Table 2, there were no significant differences in other factors that age (the ratio of patients 35 over, OR = 1.96, 95% CI, 0.89–4.52; p = 0.077), BMI (30 or more, OR = 0.622, 95% CI, 0.10–4.42; p = 0.682), the amount of blood loss (t (153) = 0.04, p = 0.960), smoking history (OR = 0.77, 95% CI, 0.24–2.76; p = 0.778), intravenous pentazocine (OR = 1.08, 95% CI, 0.28–5.04; p = 1), intrathecal fentanyl (OR = 0.51, 95% CI, 0.22–1.12; p = 0.077), intrathecal morphine and fentanyl (OR = 0.94, 95% CI, 0.40–2.29; p = 1) between two groups. In all 50 hypoxemia cases, there was not one case requiring intubation.
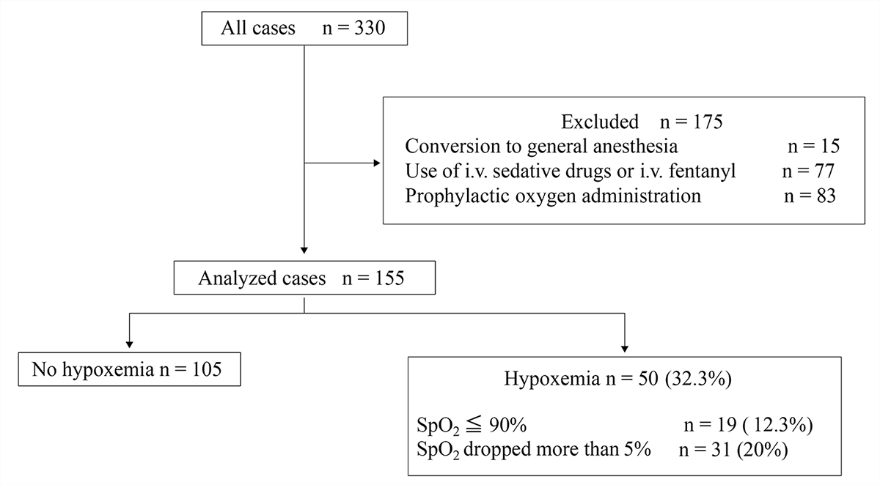
Fig. 1. The CONSORT diagram is shown. Of the 330 recruited cases, 175 cases were excluded for each reason and 155 were included in the final analysis. There are 50 cases of hypoxemia, and the details are showed. i.v : intravenous
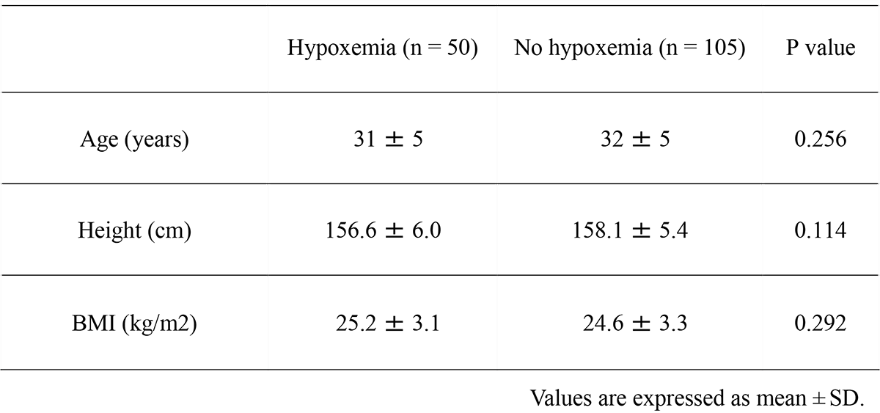
Table 1. There was no significant difference in patient background between the two groups, hypoxemia and no hypoxemia. Values are expressed as mean ± SD. A p value of less than 0.05 was defined as statistical significance.

Table 2 shows risk factors associated with hypoxemia. There was a significant difference in anesthetic level (T3 or more) between the two groups. Some data of anesthetic level were deficient, the number about anesthetic level was 9 in the hypoxemia group (※1) and 15 in the non-hypoxemia group (※2). A p value of less than 0.05 was defined as statistical significance. I.v : intravenous, I.t : intrathecal
Our study demonstrated that the incidence of hypoxemia had a high rate (32.3%) after spinal anesthesia for cesarean delivery without supplemental oxygen. As a factor associated with hypoxemia, it was detected that higher spinal anesthetic level than T3 or more. On the other hand, there were no significant differences about age (35 years or older), BMI (30 or more) and smoking history, the presence of intrathecal (i.t.) fentanyl, i.t. fentanyl and morphine, intravenous pentazocine.
Few reports have been reported about the frequency of hypoxemia during cesarean delivery. Siriussawakul and colleagues reported a hypoxemia frequency of 7.4% in no prophylactic oxygen group during cesarean delivery [ 7]. They defined hypoxemia by a reduction of oxygen saturation below 94% for more than 30 seconds. Furthermore, they showed that patients with hypoxemia had a high frequency of hypotension. In our study, the definition of hypoxemia was whenever SpO2 dropped below 90% or whenever there was a decrease of more than 5% compared to before anesthesia was performed. The reason of such a standard is because it was close to the standard for anesthesiologists to intervene such as oxygen administration in clinical practice. About blood pressure, detailed data were not analyzed, but no patient had severe hypotension, and there was no significant difference in blood loss between the groups of hypoxemia and non-hypoxemia.
Possible reasons for hypoxemia during cesarean delivery are that the reduction of respiratory function due to spinal anesthesia and the increase of maternal oxygen consumption. Ungern-Sternberg and colleagues performed spirometry preoperative period, after spinal anesthesia and mobilization. There were significant decrease in all spirometric parameters that vital capacity, forced expiratory volume in 1 s, peak expiratory flow rate after spinal anesthesia [ 8]. Spinal anesthesia with higher sensory level of T3 or more induces muscle paralysis of the intercostal and abdominal muscles. Our study also showed that SpO2 decline significantly in patients administered higher level of spinal anesthesia than T3 or more. Intrathecal opioids could be other cause of SpO2 decline [ 9], but there were no significant differences in this study. Hypoxemia during cesarean delivery may also be affected especially by intrathecal fentanyl, the short-acting, fat-soluble opioid. There have been a few case reports of respiratory depression considered to be due to fentanyl during cesarean delivery, but no studies have showed any significant difference [ 10]. Furthermore, the low dose (10–25 mcg) of fentanyl may be the reason why intrathecal opioids were not detected as factors of respiratory depression. Many studies have been reported about intrathecal morphine after cesarean delivery, morphine is water-soluble, and with respiratory depression that appears early and late and it is considered to occur between 30 and 90 minutes after intrathecal administration. However, the low dose of morphine used in recent years is considered to cause little respiratory depression at such an early phase [ 11]. Therefore, it is considered that there is little effect on respiratory depression at an early phase during surgery.
There were limitations in this study. First, this study is a retrospective study and the number of cases is rather small. The frequency of hypoxemia was more frequent during cesarean delivery, but the small number of cases may also be related to the lack of significant difference in intrathecal opioids, which was thought to affect hypoxemia. Second, data artifacts cannot be completely removed. When processing the data, we confirmed the actual SpO2 and respiratory rate graph data, but considered that the missing data for an extremely short time and the unstable signal before and after it were obvious artifacts caused by SpO2 sensor displacement, and excluded them. However, since it is difficult to exclude artifacts completely. Finally, it is not possible with this study design to reveal the frequency of true hypoxemia during cesarean delivery in all pregnant women. Pregnant women who have obvious obesity before surgery or have respiratory complications (e.g. obstructive sleep apnea syndrome) are considered to have a high risk of hypoxemia during surgery and are given oxygen prophylactically.
In conclusions, the frequency of hypoxemia during cesarean delivery is higher than previously reported, especially in patients with high anesthetic levels after spinal anesthesia. It is important to carefully observe intraoperatively and prepare to promptly administer oxygenation and other treatments if necessary.