2020 年 37 巻 4 号 p. 133-140
2020 年 37 巻 4 号 p. 133-140
Carotid artery stenting (CAS) was recommended for the treatment of severe carotid artery stenosis. One problem associated with CAS is cerebral infarction due to embolic events. Vulnerable plaque with bleeding and neovascularization is a risk factor for such events. Bleeding in plaque has been evaluated by ultrasonography and MRI. However, detection of neovascularization in plaque has not been established. We measured the intraplaque microcirculatory blood flow of 6 patients who underwent CAS with superb micro-vascular imaging (SMI). We compared the SMI signal and the embolic events following CAS. Case 3 had an SMI-positive signal with clear Doppler flow in the affected plaque; he subsequently showed plaque protrusion and asymptomatic embolic events. Another patient showed no Doppler signal. Doppler flow detected by SMI was found to be related to neovascularity of plaque. This finding might indicate the plaque vulnerability.
Internal carotid artery stenosis accounts for approximately 20% of all cases of cerebral infarction; the major cause of stenosis is atheromatous plaque. The current treatments for carotid artery stenosis include medical treatment and surgical treatment. If carotid artery stenosis is severe or symptomatic, carotid artery stenting (CAS) or carotid endarterectomy (CEA) is recommended as an evidence-based treatment for carotid stenosis.
Embolic events occur as perioperative complications when performing CAS. Emboli are caused by debris generated from vulnerable plaque. Debris may be generated in CAS procedures, such as the passing a guidewire or device through a stenotic location, stent placement, and/or balloon dilation. Alternatively, the debris may occur when plaque is pushed out of the mesh of the stent; this is called plaque protrusion.
Preoperative vulnerable plaque is currently attracting attention as a risk factor for embolic complications. Plaque vulnerability is associated with intraplaque hemorrhage and neovascularization within the plaque. We have already evaluated plaque bleeding by carotid ultrasound and magnetic resonance (MR) carotid plaque imaging. However, no method of evaluation has been established for the examination of neovascularization in plaque. In order to examine neovascularity, contrast-enhanced ultrasound (CEUS) studies have been conducted; however, the use of contrast agents in Japan poses problems, such as lack of insurance coverage for carotid artery imaging, and possible side effects associated with the use of contrast agents [ 1, 2]. On the other hand, superb micro-vascular imaging (SMI) is a recent ultrasound technology that can display images comparable to CEUS [ 3, 4].
SMI is a new blood flow imaging technique with high sensitivity, high resolution, and low artifact [ 5, 6]. The technique can effectively separate blood flow signals and overlapping tissue motion artifacts by the adaptive calculation method, and accurately detect low-speed blood flow signals [ 7].
We are investigating the possibility of assessing and quantifying plaque vulnerability, which is a risk factor for CAS, by capturing the microblood flow of neovascularization around the plaque and measuring Doppler signaling by carotid ultrasonography without contrast medium.
Patients
This was a single-center, prospective observational study. The subjects included 6 consecutive patients who underwent CAS for internal carotid artery stenosis at Shimane University from January 2018 to April 2018. Patients who could not undergo carotid ultrasound, CAS, or filter protection were excluded.
The CAS procedure was performed using a modified Parodi method by special neuro-endovascular doctors (FN and YA). A 9-Fr guiding catheter with a balloon was placed in the common carotid artery and the external carotid artery was occluded by a Percusurge Occlusion Balloon™ (Medtronic, Minneapolis, MN,. USA), and a Filter Wire EZ™ (Boston Scientific, Natick, MA, USA) was used as a filter protection device. Precise ProRX™ (Cordis, Miami, FL, USA) was used as the stent. The diameter of stent was a target blood vessel diameter of +1 to 2 mm and the stent was designed for stenosis of ≥+2 cm in length.
The present study was improved by the institutional review board of the Shimane University Medical Ethics Committee (Management number: 20171114-1, approval number: 2950), and participants received a written informed consent.
Methods
An Aplio i900™ (Canon Medical Systems Corporation, Tochigi, Japan) ultrasound machine was used. The probe used was the same model as the wideband linear probe PLI-705BX™. The ultrasound was performed as a preparative test for CAS. The following parameters were measured: peak systolicflow velocity (PSV), end-diastolic velocity (EDV), mean flow velocity (MFV), inner diameter of blood vessel, and maximum intima-media thickness (maxIMT) of the internal carotid artery. The stenosis rate was calculated using the ECST method and the area method. In addition to these measured values, ultrasound micro-flow imaging by SMI was performed. It was considered that a high echo signal on SMI indicated neovascularization in the plaque [ 1]. Then, if a clear Doppler signal was detected at the each high echo signal site of SMI, we captured a clear blood flow signal and defined it as a positive Doppler signal. In order to unify the ultrasound procedure, measurements were taken by the same neurosonographer (HN) and the results were confirmed by two doctors (FN and HN).
In addition, as a preoperative evaluation, ulcer formation was evaluated by measuring the diameter, length, and shape of the stenosis on 3D-CT angiography (CTA). Vulnerability was evaluated based on the presence or absence of intra-plaque bleeding by MR carotid plaque imagingand time-of-flight (TOF)-MR angiography. The angiographic findings and cone beam CT were used to evaluate plaque protrusion. Moreover, the occurrence of a region of high signal intensity was evaluated by postoperative MR- diffusion-weighted imaging (DWI).
We investigated and analysed the preoperative items (ultrasound, MRI, and CTA), the intraoperative findings (cerebral angiography), and the postoperative items (MR-DWI).
One of the six patients who participated in the study was excluded due to difficulty in stent placement. The remaining 5 cases included 4 males and 1 female, with an average age of 75.2 years; all patients had unilateral lesions ( Table 1). Each item was measured for 10 blood vessels, with the blood vessels treated with CAS defined as the target blood vessels and the untreated blood vessels defined as controls ( Table 2).
In the target blood vessels, the average flow velocity was 223.8 cm/s (42.3–337.3 cm/s) for PSV, 76.6 cm/s (19.0–165.6 cm/s) for EDV, and 86.9 cm/s (27.5–125.5 cm/s) for MFV. The average stenosis rate was 72.2% (65–82%) in ECST and 87.75% (79–97%) in area. The average plaque thickness was 4.4 mm (3.1–5.5 mm) at max IMT. A positive of the high echo signal of SMI in the plaque was detected in all 5 cases. A clear Doppler signal at the SMI-positive site could not be detected in the plaque, with the exception of Case 3. A clear Doppler signal was detected in this case, which was only bidirectional during systole ( Fig. 1).
In the control blood vessels, the average flow velocities were 89.5 cm/s (67.7–129.3 cm/s) for PSV, 31.0 cm/s (22.9–39 cm/s) for EDV, and 51.5 cm/s (42.2–74.5 cm/s) for MFV. The stenosis rate was not calculated for the control blood vessels. The average plaque thickness was 2.8 mm (1.7–5.2 mm) at max IMT. The high echo signal of SMI was negative in all 5 cases and there was no apparent hyperintensity in the plaque ( Tables 1 and 2).
The preoperative examination of the target vessels revealed ulceration by CTA in 3 of 5 cases, and MR plaque imaging suggested bleeding in 2 of 5 cases.
Intraoperative plaque protrusion was only seen in 1 (Case 3) of 5 cases. Case 3, postoperative MRI revealed high intensity spots on DWI. On the other hand, preoperative CTA was revealed no ulceration, and MR plaque imaging showed some high signals in the plaque. Case 3, SMI showed positive high echo signals and positive Doppler signals in the plaque ( Fig. 1). In this plaque protrusion case, the Doppler signal findings were observed at the three sites of SMI high echo signal ( Figs. 1 and 2). In addition, for comparison with MR plaque imaging, the corresponding positions of the three sites of SMI high echo signal were shown. ( Figs. 1 and 2 and 3). However, there was no apparent relationship among the SMI high echo signal, the SMI Doppler signal, and the high intensity spot on MR-DWI.
| Case | 1 | 2 | 3 | 4 | 5 | Average | |
|---|---|---|---|---|---|---|---|
| Age | 74 | 73 | 82 | 70 | 77 | 75.2 | |
| Gender | M | F | M | M | M | ||
| Disease side | Left | Right | Left | Left | Left | ||
| Blood vessel inner diameter (mm) | 5.9 | 6.8 | 5.6 | 5.6 | 6.4 | 6.1 | |
| maxIMT (mm) | 4.2 | 4.2 | 5.5 | 5.0 | 3.1 | 4.4 | |
| PSV (cm/s) | 337.3 | 42.3 | 222.8 | 315.5 | 201.0 | 223.8 | |
| EDV (cm/s) | 165.6 | 19.0 | 72.1 | 68.7 | 57.6 | 76.6 | |
| Vmean (cm/s) | - | 27.5 | 125.5 | - | 107.7 | 86.9 | |
| ECST (%) | 76 | 68 | 82 | 70 | 65 | 72.2 | |
| Area (%) | 97 | - | 90 | 85 | 79 | 87.8 | |
| Echo brightness | Low | High | High | Low | Low | ||
| SMI high echo signal | + | + | + | + | + | ||
| SMI Doppler signal | - | - | + | - | - | ||
| CTA ulceration | + | + | - | + | - | ||
| MR TOF | ISO | LOW | ISO | HIGH | LOW | ||
| plaque image | T1WI | - | ISO | ISO~HIGH | ISO | ISO~HIGH | |
| T2WI | - | ISO | ISO~HIGH | HIGH | ISO~HIGH | ||
| Plaque Protrusion | - | - | + | - | - | ||
| Postoperative DWI | - | - | + | - | - | ||
| Case | 1 | 2 | 3 | 4 | 5 | Average |
|---|---|---|---|---|---|---|
| Contralateral side | Right | Left | Right | Right | Right | |
| Blood vessel inner diameter (mm) | 5.2 | 6.6 | 5 | 4.6 | 5.4 | 5.4 |
| maxIMT (mm) | 2.6 | 2.8 | 5.2 | 1.7 | 1.8 | 2.8 |
| PSV (cm/s) | 81.6 | 67.7 | 84.2 | 129.3 | 84.8 | 89.5 |
| EDV (cm/s) | 22.9 | 31.2 | 35.7 | 39 | 26 | 31.0 |
| Vmean (cm/s) | 43.3 | 51.6 | 42.2 | 74.5 | 45.7 | 51.5 |
| Echo brightness | HIGH | HIGH | HETEROGENOUS | LOW | HIGH | |
| SMI high echo signal | - | - | - | - | - | |
| SMI Doppler signal | - | - | - | - | - |

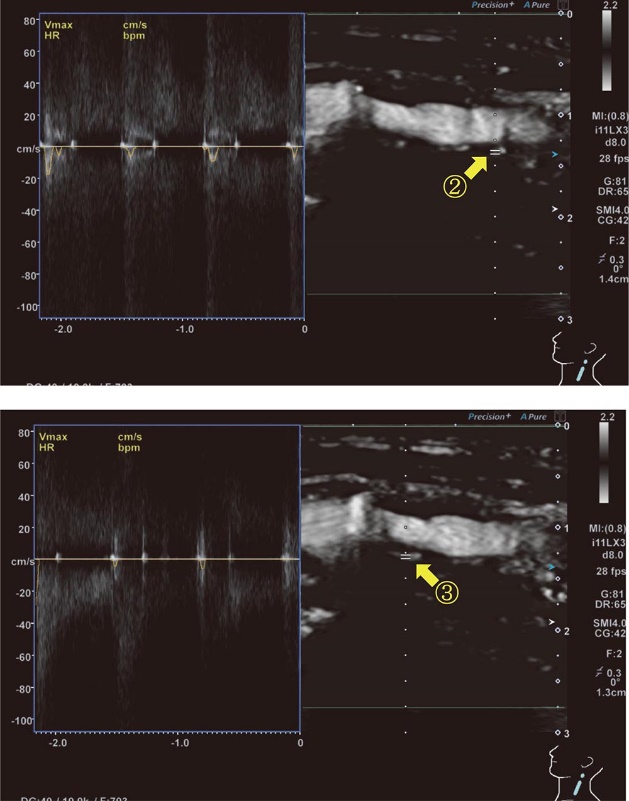
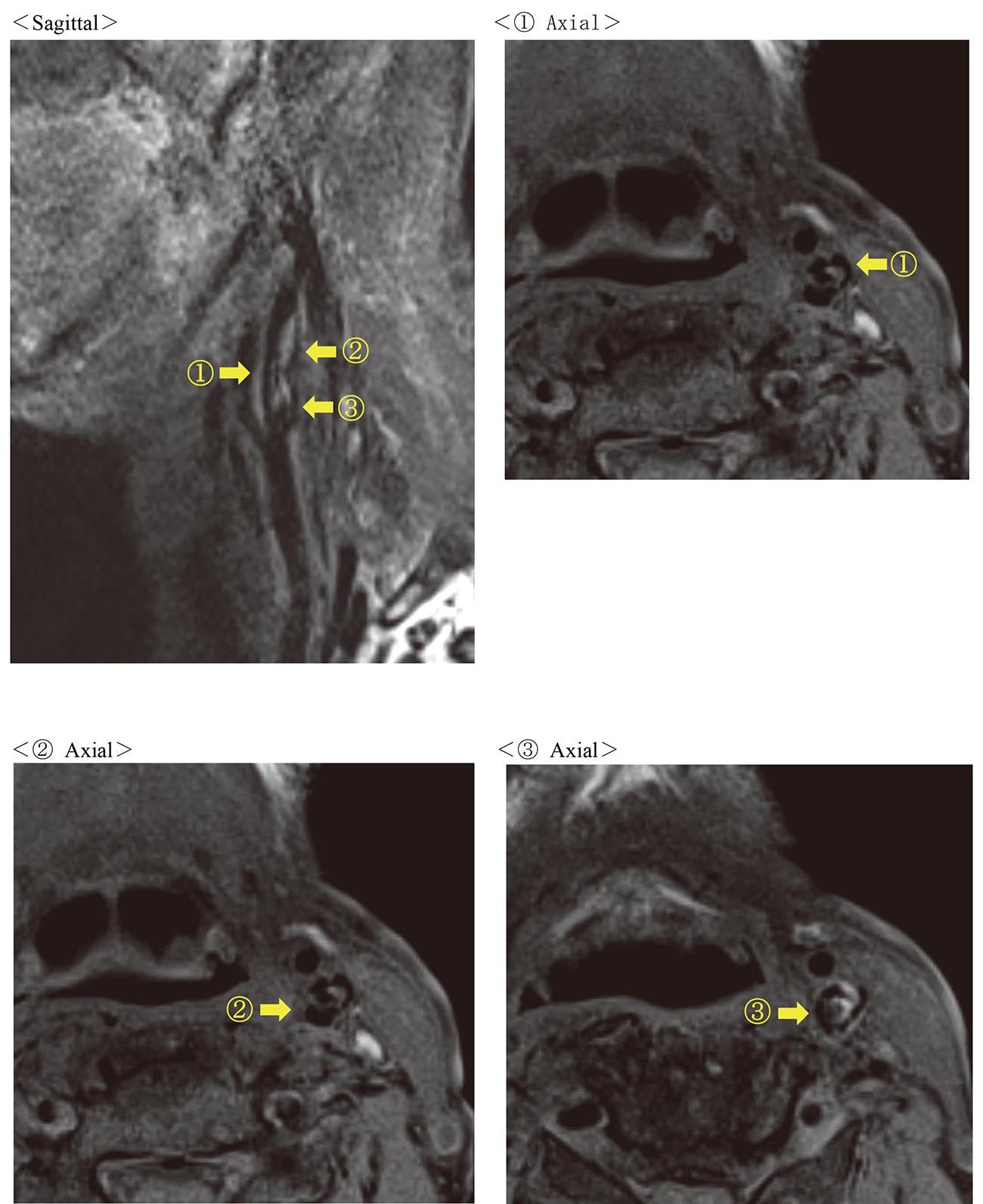
①Shows the Doppler signal-positive part in Fig.1.
② and ③ Show the Doppler signal-negative parts in Fig.2.

Carotid artery stenting was recommended for severe carotid stenosis with atheromatous plaque. Carotid plaques not only cause the stenosis and the occlusion of blood vessels, but also cause arterial embolism due to plaque vulnerability [ 8, 9]. Vulnerable plaque was one of the surgical indications for CAS and CEA, even in cases in which the stenosis ratio was not so severe. Conversely, vulnerable plaque is associated with a high risk of stroke during the stenting procedure. It is also known that vulnerable plaque is prone to complications when performing CAS, including plaque protrusion, distal embolus, and clogging of the filter, which was a distal embolus protection device. For this reason, it is important to understand how to easily detect vulnerable plaque in preparation for CAS. The pathological findings of vulnerable plaque were characterized as intraplaque bleeding, necrotic tissue, and fibrous cap rupture. On CTA vulnerable plaque showed ulceration, which was a sign that represented plaque rupture. MR plaque imaging show signal intensity on T1 and T2, which represents bleeding. The reported ultrasound findings of carotid vulnerable plaque include low echo brightness, ulceration, and mobile plaque. [ 10, 11]. These findings from the evaluation of carotid plaque vulnerability by carotid ultrasound depended on the performance of the ultrasonic equipment, the frequency of the probe, and the professional skill of the sonographer.
Yamamoto et al. noted, “The SMI had made it possible to extract clinically necessary slow blood flow information by identifying features specific to motion artifacts and enhancing their ability to eliminate them. As a result, the boundary with the blood flow cavity could be made clearer than the conventional blood flow display method, and the morphology and shape could be evaluated in more detail” [ 12]. Therefore, the morphology of the carotid plaque could be evaluated more easily and in detail using SMI. In addition to the superiority in the evaluation of the plaque morphology, SMI has been attracting attention as a test that can visualize low-flow blood flow without using contrast medium [ 3, 4]. Zhang et al. and Mahtab et al. noted, “A significant proportion of ischemic strokes are caused by emboli from unstable carotid artery plaques with intra-plaque neovascularization as a key feature of plaque instability. When intra-plaque neovascularization was evaluated using SMI and CEUS and compared with pathological findings, there was a correlation between the density of intra-plaque neovascularization and the findings of SMI and CEUS” [ 1, 13]. Intra-plaque neovascularization was reported to be associated with the promotion of the inflammatory reaction, increased permeability of the fibrous cap, increase of the atheroma core, and intra-plaque hemorrhage [ 14]. These findings of neovascularization are suggested to be possible causes of plaque vulnerability.
In this study, routine imaging modalities such as CTA, MR plaque imaging and carotid ultrasonography did not reveal any specific results in any of the 5 cases. Thus, we did not think that all patients had a high risk of CAS before surgery. However, in Case 3, plaque protrusion occurred at the time of stent procedure, and asymptomatic embolic lesions were seen by DWI postoperatively. In this protrusion case, the preoperative findings included high echo plaque on carotid ultrasound, no ulceration on CTA, ISO intensity on MR-TOF, ISO to high intensity on T1WI of MR plaque imaging, and high echo signal on SMI. These findings were also observed in the other 4 cases. The present case differed from the other cases in the positive Doppler signal at the site of the plaque that showed a high echo signal on SMI. We hypothesized that the difficult conditions might have occurred for the following reasons. 1) The neovascularization could not be displayed directly by routine carotid ultrasound, CTA, MR-TOF or MR plaque imaging. 2) In this study we observed very low flow of the SMI high echo signal in the plaque in the affected vessel that was a candidate for CAS. It was reported that the SMI high echo signal was neovascularization [ 1]. Hence if it was suggested that the SMI high echo signal represented neovascularization, we thought that this was a relatively common condition in candidates for CAS. 3) However, if this signal included noise, the true neovascularization was indicated by a clear Doppler signal. Doppler signal assessment of intra-plaque neovascularization by SMI provides information on plaque vulnerability that cannot be detected by other tests.
The present study was associated with several limitations. It was performed in a single center study and the study population was small, so it lacks statistical power. However, being able to more accurately grasp plaque vulnerability using ultrasonic equipment with SMI, which can be easily performed in routine medical care, plays an important role in deciding the treatment policy. Thus, we would like to continue to collect cases and show their statistical effectiveness.
In conclusion, plaque with a positive SMI Doppler signal might indicate true neovascularization, and it was considered that the plaque with the clear SMI Doppler signal was highly vulnerable.