2024 Volume 262 Issue 3 Pages 157-162
2024 Volume 262 Issue 3 Pages 157-162
Pulmonary fibrosis (PF) is the major complication and death-related factor of acute respiratory distress syndrome (ARDS). This study evaluated the significance of miR-141-3p in ARDS and its complication of PF aiming to identify a potential biomarker for screening ARDS and predicting the occurrence of PF. A total of 137 ARDS patients and 69 healthy individuals were enrolled in this study and the serum samples were collected from all participants. The serum miR-141-3p levels were analyzed by polymerase chain reaction. The significance of miR-141-3p in the diagnosis and development of ARDS, and the occurrence of PF was evaluated by receiver operating curve, Chi-square test, and logistic regression analysis. MiR-141-3p was downregulated in ARDS patients and showed significant potential in its diagnosis. Reduced miR-141-3p was significantly associated with the increasing Murray and APACHEII score and the occurrence of PF in ARDS patients. MiR-141-3p, Murray score, and APACHEII score were identified as risk factors for the occurrence of PF in ARDS, and miR-141-3p was also found to be downregulated in ARDS patients with PF. Additionally, miR-141-3p could discriminate ARDS patients with PF and without PF, and was closely associated with the decreased total lung capacity, carbon monoxide diffusing capacity, and forced vital capacity of ARDS patients with PF. Downregulated miR-141-3p served as a biomarker for ARDS screening disease onset and indicating the severity. Reduced miR-141-3p was also identified as a risk factor for PF in ARDS patients and was associated with the severe progression of PF.
Acute respiratory distress syndrome (ARDS) is a kind of acute diffuse lung injury occurring in a short period of time. ARDS is usually induced by severe infection, trauma, shock, and other pulmonary and extrapulmonary factors, and the clinical symptoms are acute hypoxemia and exudative changes in both lungs indicated by chest imaging (Bos and Ware 2022; Gorman et al. 2022). In the past decades, the therapeutic strategies of ARDS have been greatly improved, but the mortality of ARDS remains high. Pulmonary fibrosis (PF) is one of the major factors causing mortality of ARDS patients and is always induced by mechanical ventilation, a routine treatment for ARDS (Cabrera-Benitez et al. 2014; Michalski et al. 2022). The interaction between antiprotease and inflammatory factors in ARDS patients increases the synthesis of collagen, accelerates the deposition of collagen, and further led to PF (Villar et al. 2019). The severity of PF is closely associated with the mortality and life quality of ARDS patients. PF could directly or indirectly induce adverse outcomes of ARDS patients and has been considered the major cause of death. However, the onset of PF is relatively covert, which increases the difficulty of diagnosis and results in adverse outcomes of ARDS patients. Therefore, there is an urgent need for exploring effective biomarkers to predict the occurrence of PF in ARDS patients.
The clinical significance of non-coding RNAs (ncRNAs) in the pathogen and development of human diseases has attracted huge attention in recent years. MicroRNAs (miRNAs) have become reliable biomarker candidates and research focus in recent studies. MiRNAs are critical members of ncRNAs with a length ranging 220-280 nt and could regulate target genes at posttranscription levels. Due to the relatively stable expression of miRNAs in various body liquids, miRNAs have been considered of great potential mediating disease development. Previously, there have been several studies focusing on the identification of biomarkers for PF and ARDS, such as miR-770-5p for the development of PF and miR-384-5p and miR-338-3p for the severity of ARDS (Liu et al. 2021; Yuan et al. 2021; Zhang et al. 2022), but few studies noticed the complications of ARDS, especially the occurrence of PF. The downregulation of miR-141-3p was observed in PF in a recent study, and miR-141-3p was also found to alleviate the development of disease via regulating epithelial cell growth, apoptosis, and epithelial-mesenchymal transition (Zhu et al. 2023). Moreover, miR-141-3p was also demonstrated to play roles in regulating the progression of gastric cancer, retinoblastoma, and osteosarcoma and indicating the malignant development and adverse prognosis of hepatocellular carcinoma (Liu et al. 2017; Chen et al. 2021a; Ge et al. 2022; Liu and Wen 2022). Whether miR-141-3p could indicate the onset of ARDS and predict the occurrence of PF remains unknown.
In this study, the significance of miR-141-3p in screening ARDS and predicting the risk of PF in ARDS patients was investigated, aiming to identify a potential biomarker for screening ARDS and risk assessment of PF.
This study included 137 ARDS patients at Guizhou Provincial People’s Hospital from 2019-2021 according to the following criteria: 1) patients meet the diagnostic criteria of ARDS (ARDS Definition Task Force et al. 2012) and showed different degrees of clinical symptoms of short breath and respiratory distress; 2) patients developed symptoms within 1 week; 3) the clinical records are completed. Patients with one of the following items were excluded: 1) patients combined with malignant tumors; 2) patients induced by chronic lung diseases; 3) patients with severe arrhythmia, acute myocardial ischemia or coagulation dysfunction; 4) patients combined with immune system diseases. The occurrence of PF in ARDS patients was assessed based on previous reports using high-resolution chest computed tomography (CT) (Fujimoto et al. 2012). The appearance of ground glass shadows, cellular changes in both lungs, fibroproliferation, and grid shadows indicated the occurrence of PF. According to the occurrence of PF, ARDS patients were further divided into the PF group and non-PF group to estimate the significance of miR-141-3p in predicting the risk of PF in ARDS patients.
Another 69 healthy individuals were enrolled from the physical examination center of our hospital and the results of the physical examination showed no abnormality. The study had been approved by the Ethics Committee of Guizhou Provincial People’s Hospital. All participants had signed informed consent. The clinicopathological features of study subjects were collected from clinical records and physical examination reports.
Sample collectionFasting venous blood samples were collected from all participants within 24 h of diagnosis. Collected blood samples were centrifugated at 5,000 r/min for 10 min with 2 h of sample collection to isolate serum. Isolated serum samples were stored at −80°C for the following analyses.
Real-time quantitative PCRTotal RNA was extracted from serum samples using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) and then reverse-transcribed to cDNA after evaluating concentration and purification. PCR amplification was conducted on the ABI PRISM 7900 PCR system (Applied Biosystem, Forster City, CA, USA) with SYBR Green qPCR SuperMix and the following primers: miR-141-3p forward 5´-ACACTCCAGCTGGGTAACACTGTCTGGTAA-3´, reverse 5´-CTCAACTGGTGTCGTGGAGTCGGCAATTCAGTTGAGCCATCTTT-3´; cel-miR-39 forward: 5´-UCACCGGGUGUAAAUCAGCUUG-3´, cel-miR-39 reverse: 5´-TCACCGGGTGTAAATCAGCTTG-3´. Cel-miR-39 was used as the internal reference, and the 2−ΔΔCT method was used to calculate the relative expression of miR-141-3p. The thermal cycle was performed as: 35 cycles at 98°C for 10 seconds, 50-60°C for 45 seconds, and 72°C for 45 seconds.
Statistical analysesAll data were expressed as mean ± standard deviation (SD) and analyzed by SPSS 23.0 software and GraphPad Prism 9.0 software. Difference comparison was performed with unpaired Student’s t-test (P < 0.05). The correlation of miR-141-3p with patients’ clinicopathological features was evaluated by the Chi-square test. The discrimination between ARDS patients, healthy individuals, and ARDS patients with PF by miR-141-3p was assessed by receiver operating characteristic (ROC) analysis [area under the curve (AUC) > 0.5 indicates the significant diagnostic potential]. Youden index was calculated by the summation of sensitivity and specificity. The sensitivity and specificity corresponding to the maximum Youden index are considered the diagnostic sensitivity and specificity of miR-141-3p. The logistic regression analysis was employed to estimate the potential of miR-141-3p in predicting the occurrence of PF in ARDS patients.
The healthy individuals were composed of 44 males and 23 females with an average age of 54.54 ± 9.85 years (mean ± SD). While the ARDS patients included 94 males and 45 females with an average age of 55.31 ± 9.63 years (mean ± SD). The sex and age composition of the two groups was matched with insignificant differences (data not shown).
The serum miR-141-3p levels of ARDS patients were significantly lower than that of healthy individuals (Fig. 1a). Reduced miR-141-3p could discriminate ARDS patients from healthy individuals with a sensitivity of 81.02% and a specificity of 78.26% (Fig. 1b).

Expression of miR-141-3p and its diagnostic significance in acute respiratory distress syndrome (ARDS).
(a) MiR-141-3p was downregulated in ARDS patients compared with healthy individuals. ****P < 0.0001. (b) Reduced miR-141-3p discriminates ARDS patients from healthy individuals with an AUC of 0.861.
According to the average serum miR-141-3p level in ARDS patients, a low-miR-141-3p group including 47 males and 22 females, and a high-miR-141-3p group composed of 45 males and 23 females were constructed. The low-miR-141-3p group showed higher Murray scores, APACHEII scores, and high incidence of PF, and the association of miR-141-3p with these clinicopathological features of ARDS patients was also significant (Table 1).
Moreover, serum miR-141-3p was also identified as a risk factor for the occurrence of PF in ARDS patients with the odds ratio (OR) value of 0.237 (95% CI = 0.104-0.538, Fig. 2a). Consistently, the expression of miR-141-3p was much lower in ARDS patients with PF than that in patients without the occurrence of PF (Fig. 2b). The lower serum miR-141-3p in ARDS could also distinguish ARDS patients with PF or without PF with a high specificity of 92.19%, but the sensitivity was unsatisfying (Fig. 2c). Also based on the average serum miR-141-3p levels, ARDS patients with PF were divided into the low-miR-141-3p and the high-miR-141-3p groups. There were no significant differences observed in the age and sex composition between the two groups. The lower serum miR-141-3p was associated with the lower TLC (P = 0.007), DLCO (P = 0.014), and FVC (P = 0.015) of PF patients, which are closely associated with the severity of PF (Table 2).
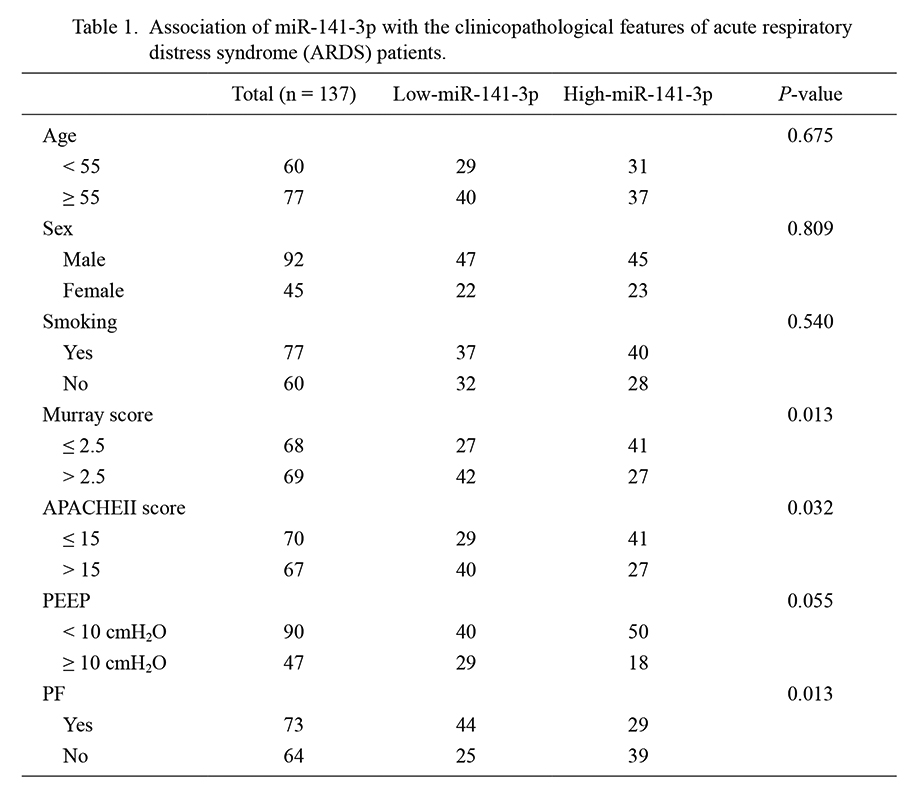
Association of miR-141-3p with the clinicopathological features of acute respiratory distress syndrome (ARDS) patients.
APACHEII, Acute Physiology and Chronic Health Evaluation; PEEP, positive end-expiratory pressure ventilation; PF, pulmonary fibrosis.

Significance of miR-141-3p in predicting and diagnosing pulmonary fibrosis (PF).
(a) MiR-141-3p was identified as a risk factor for the occurrence of PF in ARDS patients together with the Murray score and APACHEII score. (b) The expression of miR-141-3p was lower in the ARDS patients with PF than that in the patients without PF. ****P < 0.0001. (c) Reduced miR-141-3p could distinct PF patients with an AUC of 0.771.

Association of miR-141-3p with the clinicopathological features of acute respiratory distress syndrome (ARDS) patients with pulmonary fibrosis (PF).
TLC, total lung capacity; DLCO, carbon monoxide diffusing capacity/predict value; FVC, forced vital capacity.
Thanks to the development of molecular biology, an increasing number of studies noticed the significance of miRNAs in human diseases. MiR-141-3p was a functional miRNA located on chromosome 12q 13.31 and has been identified as a reliable biomarker for various human malignancies, such as colon cancer, hepatocellular carcinoma, and clear cell renal cell carcinoma (Liep et al. 2016; Tong et al. 2021; Wang et al. 2023). Additionally, miR-141-3p was also previously demonstrated to express in lung and regulate acute lung injury and lung fibroblasts (Jin et al. 2018; Xia et al. 2021). This study focused on the expression and significance of miR-141-3p in ARDS and observed its significant downregulation in the serum of ARDS patients. The blood examination is a routine examination in the clinic, and serum is a suitable medium for identifying biomarkers for the early detection of human diseases. For example, miR-338-3p was demonstrated to serve as a biomarker of neonatal ARDS related with the occurrence and severity of ARDS (Zhang et al. 2022). Murray and APACHEII scores are widely employed in the evaluation of lung injury and could predict the outcomes of ARDS patients (D’Negri and De Vito 2010; Ryan et al. 2016; Akhter et al. 2019). However, the specificity of these two scores is unsatisfactory, and the scoring criteria are subjective. For instance, APACHEII cannot specifically discriminate sepsis, ARDS, and acute kidney injury patients (Chen et al. 2021b). Here, the reduced serum miR-141-3p showed significant diagnostic value in distinguishing ARDS patients from healthy individuals with satisfying sensitivity and specificity. Additionally, decreased miR-141-3p was significantly associated with the increasing Murray and APACHEII scores in ARDS patients, indicating its association with the disease severity and aggravated development.
PF is one of the major death-related factors of ARDS patients, and there was a lack of effective biomarkers to indicate the severity and disease development and predict the risk of PF in ARDS patients (Cabrera-Benitez et al. 2014). In the clinic, the diagnosis is mainly based on clinical symptoms, imaging examination, and lung function evaluation, which cannot provide an advancing assessment for PF onset (Cottin et al. 2018; Finnerty et al. 2021). Of the enrolled 137 ARDS patients in this study, 73 patients occurred PF accounting for 53% of the study subjects. The reduced serum miR-141-3p in ARDS patients was also found to be associated with the occurrence of PF. The downregulation of miR-141-3p and the increasing Murray and APACHEII scores were identified as risk factors for PF in ARDS patients. Meanwhile, miR-141-3p was also downregulated in ARDS patients with PF compared with patients who had not suffered from PF. The downregulation of miR-141-3p could also screen the occurrence of PF with high specificity, but the sensitivity is unsatisfactory. Among the clinicopathological features of ARDS patients with PF, miR-141-3p was associated with the decreased TLC, DLCO, and FVC of ARDS patients with PF. During the pathogen of PF, the total lung capacity and vital capacity of patients dramatically decreased, limiting the gas transportation and the dispersion function of the lung also decreased (Cortes-Telles et al. 2014; Aussedat et al. 2020; Sharma et al. 2021; Dirol et al. 2022). The close relationship between serum miR-141-3p and reduced lung capacity and dispersion function suggested that miR-141-3p is associated with PF progression in ARDS patients.
In conclusion, downregulated miR-141-3p in ARDS served as a diagnostic biomarker and a risk factor for the severe development of ARDS and the occurrence of PF. The downregulation of miR-141-3p was also observed in ARDS patients with PF, which screened the occurrence of PF and indicated the aggravated progression of PF. However, due to the limited study period, whether miR-141-3p also played roles in predicting outcomes of ARDS patients and the patients combined with PF remains undisclosed. The sample size of the present study is also relatively small, which needs further tracing investigations with expanding sample size. On the other hand, the underlying mechanism of miR-141-3p is also an important issue to complete the regulatory network of miR-141-3p and provide therapeutic targets and novel insights into the therapeutic strategies of PF in ARDS. Future studies would deeply explore the role of miR-141-3p in PF from the molecular perspective to reveal its regulatory mechanisms.
This work was supported by Mechanisms by which MiRNA-141 promotes lung fibrosis in ARDS rats through activation of the Keap1-Nrf2/ARE signaling pathway (Grant number: 82160021).
The authors declare no conflict of interest.