2016 Volume 39 Issue 4 Pages 556-563
2016 Volume 39 Issue 4 Pages 556-563
Lung allergic diseases sometimes accompany pulmonary vaso- and broncho-constriction. Rats are currently used for the experimental study of lung allergies. However, their hemodynamic mechanisms are not fully understood. Therefore the effects of allergic mediators were determined systematically in vivo in rats in terms of pulmonary vascular resistance (PVR), airway pressure (AWP) and total peripheral resistance (TPR). We directly measured pulmonary arterial pressure, left atrial pressure, systemic arterial pressure, central venous pressure and aortic blood flow to determine PVR and TPR, as well as AWP, following injections of platelet-activating factor (PAF), histamine, serotonin, leukotriene (LT) C4, and prostaglandin (PG) D2 in anesthetized open-chest artificially ventilated Sprague-Dawley (SD) rats. PVR was dose-dependently increased by consecutive administration of PAF, LTC4, and PGD2, with the maximal responsiveness being PAF>LTC4>PGD2. However, neither histamine nor serotonin changed PVR. TPR was decreased by all agents except LTC4 which actually increased it. PAF and serotonin, but not the other agents, increased AWP. In conclusion, allergic mediators exert non-uniform actions on pulmonary and systemic circulation and airways in anesthetized SD rats: PAF, LTC4 and PGD2, but not histamine or serotonin, caused substantial pulmonary vasoconstriction; LTC4 yielded systemic vasoconstriction, while the others caused systemic vasodilatation; only two mediators, PAF and serotonin, induce airway constriction.
Rats are currently used for investigations on pulmonary allergic diseases.1–4) However, the studies on physiological characteristics of the rat pulmonary circulation were limited. The rat pulmonary vascular responses to various endogenous allergic mediators were previously examined in isolated perfused lungs5–7): platelet-activating factor (PAF) and leukotriene (LT) C4 cause substantial vasoconstriction. In rat isolated pulmonary arteries,8,9) serotonin showed strong constriction. However, there is no systematic study in which the effects of allergic mediators on the rat pulmonary vascular resistance (PVR) and total peripheral resistance (TPR) were determined by measuring cardiac output (CO) and the inflow and outflow pressures of the systemic and pulmonary circulations. Therefore, we measured directly and continuously CO, pulmonary arterial pressure (PAP) and left atrial pressure (LAP), along with systemic arterial pressure (SAP) and central venous pressure (CVP), in order to determine the responses of PVR and TPR to allergic mediators including PAF, histamine, serotonin, LTC4, and prostaglandin (PG) D2 in anesthetized Sprague-Dawley (SD) rats. Airway pressure (AWP) was also measured to determine whether the allergic mediators cause bronchoconstriction. We hypothesized that these mediators do not exert the same directional actions on pulmonary and systemic circulation and airway.
Forty male SD rats (Japan SLC, Shizuoka, Japan) weighing 362±3 g (9 week) were used in this study. Rats were maintained at 23°C and under pathogen-free conditions on a 12 : 12-h dark/light cycle and allowed food and water ad libitum. The experiments conducted in the present study were approved by the Animal Research Committee of Kanazawa Medical University.
Surgical PreparationRats were anesthetized with pentobarbital sodium (60 mg/kg, intraperitoneally (i.p.)), placed supinely on a heating pad with body temperature at 36–37°C, and mechanically ventilated with a tidal volume of 7 mL/kg, a respiratory rate of 60/min and a positive end-expiratory pressure (PEEP) of 2.5 cmH2O.10) AWP and SAP were measured from the inspiratory line and left femoral artery, respectively. The right external jugular vein was catheterized with a 22-gauge catheter, which was connected to a Y-type tube with one twig end for measurement of CVP, and another twig end for introducing a thin inner tube tapered to around 0.1 mm in diameter for allergic mediator injections.
After a chest midline incision, polyethylene catheters (0.3 mm i.d., 0.5 mm o.d.) were inserted into the pulmonary artery via the right ventricle, and into the left atrium for measurement of PAP and LAP, respectively. The pulsed Doppler flow probe (MC2PSS; Transonic Systems, Ithaca, NY, U.S.A.) was placed on the ascending aorta for measurement of aortic blood flow (ABF).
Experimental ProtocolIn anesthetized open-chest rats, SAP, PAP, LAP, CVP and AWP were continuously monitored. These variables were recorded at 40 Hz by PowerLab (AD Instruments, Australia). PVR and TPR were calculated as follows:
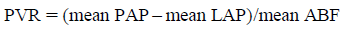 | (1) |
 | (2) |
At 20 min after surgery, the baseline measurements were performed. Then PAF, histamine, serotonin, LTC4, or PGD2 was intravenously administered via the jugular vein as a bolus consecutively basically from the starting dose of 0.01 nmol/kg, unless otherwise mentioned, with an injection volume of 50 µL. In addition, the effect of pretreatment with the thromboxane receptor antagonist SQ 29548 (0.1 mg/kg, intravenous (i.v.)) at 10 min before PAF injection on the PVR and AWP responses to PAF was studied for the post-SQ 29548 PAF group. When hemodynamic variables returned to the pre-injection levels within 10 min after preceding administration of a smaller dose, a subsequent higher dose was administered. Each animal received only one agent. We also performed the control studies in which 50 µL saline alone as the control for the histamine and serotonin groups, or 50 µL saline-diluted ethanol (20%) as the control for the PAF, post-SQ 29548 PAF, LTC4, and PGD2 groups was intravenously injected at 10 min intervals over 50 min. Five rats were assigned to each drug and control group.
DrugsAll drugs except SQ 29548 were purchased from Sigma Chemical Company (St. Louis, MO, U.S.A.), and SQ 29548 from Cayman Chemicals (Ann Arbor, MI, U.S.A.). Histamine and serotonin were dissolved in saline. PAF, LTC4, PGD2 and SQ 29548 were dissolved in 95% ethanol for stock solution, which was diluted with saline for the working solution.
Statistical AnalysisResults are expressed as the mean±standard error of the mean (S.E.M.) Intragroup comparisons were performed using two-way ANOVA for repeated measures. Intergroup comparisons were performed using one-way ANOVA. When a significant difference was observed, post-hoc test was performed by using Bonferroni. The statistical analyses were performed by Stat View, version 5.0 (SAS Institute Inc., Cary, NC, U.S.A.).
The basal hemodynamic values for each group were shown in Table 1. The summarized data of 40 rats were as follows: mean SAP, 107±5 mmHg; CVP, 3.6±0.5 mmHg; mean PAP, 18.2±0.8 mmHg; mean LAP, 4.9±0.1 mmHg; mean ABF, 44.5±3.2 mL/min; TPR, 2.4±0.2 mmHg·min/mL; PVR, 0.32±0.5 mmHg·min/mL; heart rate (HR), 412±10 beats/min; peak AWP, 10.3±0.6 cmH2O.
| Groups | MAP (mmHg) | CVP (mmHg) | PAP (mmHg) | LAP (mmHg) | ABF (mL/min) | AWP (cmH2O) | HR beats/min | TPR (mmHg·min/mL) | PVR (mmHg·min/mL) |
|---|---|---|---|---|---|---|---|---|---|
| PAF (n=5) | 107±3 | 4.1±1.0 | 19.1±0.9 | 4.6±0.1 | 42.6±4.5 | 10.6±0.1 | 422±16 | 2.5±0.3 | 0.36±0.04 |
| Post SQ 29548 PAF (n=5) | 108±4 | 3.6±0.4 | 18.8±1.1 | 4.8±0.2 | 49.5±5.2 | 10.5±0.5 | 415±11 | 2.2±0.2 | 0.29±0.04 |
| Histamine (n=5) | 112±5 | 3.6±0.5 | 18.7±1.0 | 4.9±0.2 | 44.9±5.3 | 10.5±0.5 | 428±5 | 2.6±0.5 | 0.35±0.07 |
| Serotonin (n=5) | 110±3 | 3.8±0.4 | 18.3±1.1 | 4.7±0.4 | 38.9±4.5 | 11.0±0.8 | 428±20 | 2.8±0.3 | 0.37±0.05 |
| LTC4 (n=5) | 105±5 | 3.2±0.3 | 18.3±1.0 | 5.3±0.2 | 43.5±1.9 | 10.1±0.6 | 414±13 | 2.4±0.1 | 0.30±0.03 |
| PGD2 (n=5) | 103±6 | 3.3±0.5 | 16.9±1.0 | 4.9±0.4 | 42.3±3.1 | 10.4±0.5 | 384±15 | 2.4±0.2 | 0.29±0.03 |
| Saline control (n=5) | 102±4 | 3.5±0.3 | 17.8±1.2 | 4.8±0.3 | 45.5±2.5 | 9.9±0.5 | 395±12 | 2.2±0.5 | 0.29±0.01 |
| Ethanol control (n=5) | 107±6 | 3.6±0.5 | 18.2±1.0 | 5.1±0.3 | 47.5±2.7 | 9.8±0.7 | 410±11 | 2.3±0.2 | 0.28±0.02 |
Values are the mean±S.E.M. MAP, mean systemic arterial pressure; CVP, central venous pressure; PAP, pulmonary arterial pressure; LAP, left atrial pressure; ABF, aortic blood flow; AWP, airway pressure; HR, heart rate; TPR, total peripheral resistance; PVR, pulmonary vascular resistance.
Figure 1 shows representative recordings of the changes in the variables after injections of PAF at doses ranging from 0.01 to 100 nmol/kg in an anesthetized rat. Figure 2 shows the summarized data of maximal changes in PVR, TPR, and AWP in all groups studied. At 0.1–100 nmol/kg, both SAP and ABF decreased, resulting in decreases in TPR. At 100 nmol/kg, TPR decreased until 1 min, thereafter followed by a marked increase due to a progressive decrease in ABF. At 10 and 100 nmol/kg, PAP initially and transiently increased by 1.5±0.2 and 7.5±0.8 mmHg, respectively followed by a sustained decrease which accompanied the progressive decrease in ABF. Concomitantly with the initial PAP increase, PVR significantly increased to 167±13% and 268±21% baseline within 1 min after injection of 10 and 100 nmol/kg PAF, respectively. There followed a huge increase in PVR due to a large reduction of ABF at 100 nmol/kg (Fig. 1, bottom right). We adopted the PVR values at the initial phase, but not at the late phase, as the maximal PVR shown in Fig. 2. At 1 nmol/kg PAP showed only a depressor response along with a decrease in ABF. AWP increased dose-dependently at 10 and 100 nmol/kg (Figs. 1, 2C-1).

Pulmonary vascular resistance (PVR) and total peripheral resistance (TPR) were also shown, which were automatically calculated by Figs. 1 and 2 with PowerLab. White and black arrow heads, and arrows indicate the time points when the changes in PVR, TPR, and AWP, respectively, were determined as the maximal ones.

* p<0.05, versus the baseline. The time points when the maximal changes were determined are indicated in the representative recordings (Figs. 1, 3–7) for each agent by white or black arrow heads, or arrows for PVR or TPR, or AWP, respectively. * p<0.05, versus the baseline; # p<0.017, versus the control group (black bars); † p<0.017, versus the PAF group.
Next we determined, by pretreatment with SQ 29548, the roles of thromboxane in the responses of the pulmonary vessels and airway to PAF. As expected, the PAF-induced increases in PAP, PVR and AWP, as observed in rats without SQ 29548 pretreatment (Fig. 1), were abolished by SQ 29548 (Fig. 3).

Black arrow heads indicate the time points when the changes in TPR were determined as the maximal ones. Notably, the increases in PAP, as observed in Fig. 2, were not observed.
Histamine produced significant decreases in both SAP and TPR, and an initial and transient increase in ABF at doses of 0.1 µmol/kg or higher (Figs. 2B-2, 4). At 1–100 µmol/kg, ABF showed a biphasic response of the initial increase followed by a slight decrease. PAP did not increase but decreased along with a decrease in ABF. Consequently, PVR did not change significantly at any doses studied (Figs. 2A-2, 4). AWP showed no significant change at any doses (Figs. 2C-2, 4).

Black arrow heads indicate the time points when the changes in TPR were determined as the maximal ones.
Serotonin decreased SAP and TPR at 10–300 nmol/kg (Figs. 2B-3, 5). Shortly after injections of 100 and 300 nmol/kg, PAP increased significantly but only slightly by 2.8±0.5 and 3.1±0.8 mmHg, respectively. This increase of PAP was concurrently accompanied by increases in LAP by 3.5±0.7 and 4.2±0.9 mmHg, respectively, but only small insignificant increases in ABF by 0.2±0.05 and 0.1±0.07 mL/min, respectively. Consequently, PVR did not significantly change (Figs. 2A-3, 5). AWP significantly increased at doses of 100 and 300 nmol/kg (Figs. 2C-3, 5).

Black arrow heads and arrows indicate the time points when the changes in TPR and AWP, respectively, were determined as the maximal ones.
In contrast to other mediators, LTC4 increased SAP initially and transiently, and decreased it sustainably, along with a decrease in ABF, resulting in a dose-dependent increase in TPR at 1, 10 and 30 nmol/kg (Figs. 2B-4, 6). At 1 nmol/kg and higher, PAP showed a dose-dependent decrease along with a decrease in ABF, although PAP at 10 and 30 nmol/kg an initial and transient elevation by 1.8±0.3 and 2.3±0.5 mmHg, respectively (Fig. 6). With 10 and 30 nmol/kg LTC4, the corresponding increases in PVR at the initial phase were 5.0±0.7% and 51±7% but the increases observed at late low ABF phase were 56±9 and 64±11%, respectively. Of note, the initial increase in PVR, which was accompanied by the increase in PAP, was apparently due to pulmonary vasoconstriction, and their data were shown in Fig. 2A-4. AWP did not change significantly at any doses studied (Fig. 2C-4).

White and black arrow heads indicate the time points when the changes in PVR and TPR, respectively, were determined as the maximal ones.
At 10–300 nmol/kg, SAP decreased and ABF increased, resulting in a decrease in TPR (Figs. 2B-5, 7). At 100 and 300 nmol/kg, PVR increased slightly but significantly by 26±4 and 31±5%, respectively; PAP increased substantially by 5.0±0.7 and 7.3±1.0 mmHg, respectively. AWP did not change significantly at any doses.

White and black arrow heads indicate the time points when the changes in PVR and TPR, respectively, were determined as the maximal ones.
Ethanol (20%) and saline alone exerted no significant effects on the measured variables, as shown in Fig. 2.
We determined the responses of systemic and pulmonary circulation, as well as AWP, to allergic mediators in anesthetized open-chest SD rats. There are three major findings: 1) PAF, LTC4 and PGD2, but not either histamine or serotonin, increased PVR, with the rank of the potency being PAF>LTC4>PGD2; 2) Only LTC4 increased TPR, whereas the other agents decreased it; and 3) PAF and serotonin, but not the others, increased AWP in anesthetized SD rats.
PAF is a potent smooth muscle contractor. Actually, in anesthetized rats, inhalation of PAF causes bronchoconstriction.11) Consistently, we confirmed the ability of PAF administered intravenously to increase AWP in vivo rats. In contrast, with respect to the action of PAF in pulmonary circulation, Clavijo et al. reported that PAP in in vivo rats did not increase but rather decreased along with systemic hypotension when PAF was intravenously infused.12) We here demonstrated that PAF definitely increased PVR in in vivo rats at the high doses of 10–100 nmol/kg, although the small dose of 1 nmol/kg caused only a decrease in PAP along with a decrease in ABF. Indeed, PAF-induced vasoconstriction was well known in isolated perfused rat lungs.13) On the other hand, the late increase in PVR at 100 nmol/kg might be simply due to a passive effect of lower blood flows,14,15) rather than pulmonary vasoconstriction: ABF decreased hugely, resulting in collapse of pulmonary vessels and finally development of a marked increase in PVR. Pulmonary vasoconstriction and bronchoconstriction induced by PAF in rats are reported to be largely mediated by thromboxane.13,16) Actually in in vivo rats, thromboxane analogue, U46619, causes substantially both pulmonary vasoconstriction and bronchoconstriction.10) We here reinforced this conception in in vivo rats by showing that the PAF-induced increases in PVR and AWP were abolished by pretreatment with the thromboxane receptor antagonist SQ 29548.
Histamine causes pulmonary vasoconstriction in animals such as rabbits,17,18) dogs,19) cats,20) guinea pigs,21) pigs,22) and horses.23) Histamine is also reported to exert pulmonary vasodilator actions preferentially during vasoconstriction and in other conditions of high PAP in animals18–20) including rats.20,24) However, our study showed no changes in PVR in response to histamine, indicating that histamine did not cause pulmonary vasoconstriction or vasodilatation in in vivo rat lungs. The lack of substantial pulmonary vasoconstrictive action for histamine in rats is consistent with the previous report.25) Furthermore, the present study demonstrates that histamine does not exert a vasodilatory action at the basal pulmonary vascular tone in in vivo rats. It is generally assumed that pulmonary vasodilatation is induced by activation of not only vascular smooth muscle H2 receptor but also endothelial H1 receptor which is associated with NO production, while pulmonary vasoconstriction by activation of vascular smooth muscle H1 receptor.26–28) Further study is required to determine how individual histamine receptor subtypes contribute to the absence of substantial pulmonary vasomotion of anesthetized rats.
In contrast to histamine, serotonin is currently reported to cause pulmonary vasoconstriction and bronchoconstriction in isolated pulmonary arteries8) and perfused lungs29,30) from rats. In the present in vivo rats serotonin at 100 and 300 nmol/kg significantly increased AWP and PAP. However the increase in PAP was as small as 3.1 mmHg at 300 nmol/kg, and PVR did not significantly increase due to the concurrent increase in LAP. This finding indicates that serotonin does not apparently cause pulmonary vasoconstriction in anesthetized rats. This finding is consistent with the previous report for anesthetized rats: a similar small increase in PAP of 3.0 mmHg was observed in response to an intravenous injection of serotonin at 30 µg/kg,31) i.e., 142 nmol/kg, the comparable dose to that used in the present study. The absence of pulmonary vasoconstriction in anesthetized rats is not in agreement with the previous reports on other mammals, in which activation of the 5-HT1B/1D and 5-HT2A receptors has been implicated in serotonin-induced pulmonary vasoconstriction.32,33) The reason for the absence of serotonin-induced pulmonary vasoconstriction in in vivo anesthetized rats is not known, and the further study is required.
The systemic pressor and pulmonary depressor actions of LTC4 in the rat were previously reported.34) However, this previous study was limited because of the lack of PVR determination; as the authors discussed, whether the pulmonary depressor response was due to the generation of a pulmonary vasodilator substance or resulted from a reduction in cardiac output could not be specifically determined. In contrast to this previous report, we clearly observed LTC4-induced pulmonary vasoconstriction, as evidenced by an increase in PVR along with an increase in PAP at the early phase (as indicated by white arrow heads in Fig. 6). The later increase in PVR was due to a reduction of ABF. The cysteinyl LT binds to the cysteinyl LT receptors 1, 2, and 3 or the cysteinyl LT receptor E4.35–37) Cysteinyl LTs evoke contradictory effects on vascular tone, depending on the species and the experimental preparations,38) via both endothelium- and smooth muscle-dependent actions. The functional roles of these cysteinyl LT receptors in regulation of pulmonary vessels still remain unknown.
PGD2 dose-dependently increased PVR, albeit to a small extent, in the present study. This finding is not consistent with the previous report that either PVR or the blood flow to lung did not change in response to a PGD2 receptor agonist in anesthetized rats.39) However, in this previous study, the blood flow was measured with the microsphere method only one time at the end of infusions of the agonist. Thus the maximal response of PVR might have been missed. In contrast, we measured continuously ABF as well as the inflow and outflow pressures of the lung to obtain PVR exactly. In agreement with the present result, PGD2 produces pulmonary vasoconstriction in adult gouts,40) dogs,41) sheep,42) and cats.43) On the other hand, PGD2-induced decreases in SAP were well known in rats44) as well as dogs and monkeys45); the present study reinforced these observations by showing that hypotension is caused by a decrease in TPR in anesthetized rats. DP1 receptor, one of the PGD2 receptors leads to vasodilatation,46) which seem to be responsible for the decrease in TPR, while pulmonary vasoconstriction induced by PGD2 might be mediated by thromboxane receptors.42)
In summary, we determined the responses of PVR, TPR and AWP to allergic mediators in anesthetized open-chest SD rats. PAF, LTC4 and PGD2, but not either histamine or serotonin, increased PVR, with the rank of the potency being PAF>LTC4>PGD2. However, pulmonary hypertension induced by these pulmonary vasoconstrictors was small in magnitude. In contrast, systemic hypotension or TPR reduction was induced by all mediators studied except LTC4. AWP was increased by PAF and serotonin, but not by the other mediators in the present rat in vivo preparations. The PAF-induced increases in PVR and AWP were abolished by the thromboxane receptor antagonist. These results demonstrate that allergic mediators exert non-uniform actions on the pulmonary and systemic circulation and airway in anesthetized SD rats.
The authors declare no conflict of interest.