2022 Volume 45 Issue 4 Pages 522-527
2022 Volume 45 Issue 4 Pages 522-527
The accumulation of uremic toxins is known to be one of the causes of cardiovascular disorder related to renal disease. Among the many uremic toxins, we focused on kynurenine (kyn), whose levels have been shown to be positively correlated with vascular endothelial dysfunction markers, and directly evaluated the influence of kyn on the rat thoracic aorta. Exposure of the endothelium-intact aorta to kyn markedly attenuated the acetylcholine (ACh)-induced relaxation and significantly increased superoxide anion (O2·−) production. These effects were ameliorated by pretreatment with ascorbic acid, an antioxidant, and CH223191, an aryl hydrocarbon receptor (AhR) inhibitor, but not by apocynin, a reduced nicotinamide adenine dinucleotide phosphate (NADPH) oxidase inhibitor. In the endothelium-denuded aorta, kyn significantly attenuated the nitric oxide (NO) donor sodium nitroprusside (SNP)-induced vasorelaxation and increased the O2·− production. Ascorbic acid treatment significantly ameliorated these effects, whereas CH223191 and apocynin treatments did not. Kyn had no influence on the vasorelaxant response to BAY 41-2272, a soluble guanylate cyclase stimulator. This suggested that kyn attenuates the NO-mediated vasorelaxation response by promoting O2·− production in thoracic aorta to inactivate NO. O2·− production is likely stimulated in both vascular endothelium and smooth muscle, the former of which may be mediated by AhR activation.
Chronic kidney disease (CKD), especially end-stage renal disease (ESRD), increases the incidence of cardiovascular disease (CVD).1,2) The pathogenesis of CVD associated with CKD includes classical factors such as hypertension, diabetes mellitus, dyslipidemia and hyperuricemia.3) However, in recent years, sympathetic hyperactivity, renal anemia and uremic toxins accumulation have been focused on as non-classical factors.4) In particular, uremic toxins are normally excreted in the urine, but patients with CKD have chronically impaired renal function, and uremic toxins accumulate in the body, making them prime candidates for CVD associated with CKD.5,6)
Tryptophan-derived metabolites act as typical uremic toxins.7) Tryptophan is one of the essential amino acids found in the diet and is mainly metabolized by the serotonin pathway, the indolic pathway and the kynurenine (kyn) pathway.8) In the kyn pathway, the rate-limiting enzyme, indoleamine 2,3-dioxygenase (IDO), reacts with tryptophan to produce N-formylkynurenine, which in turn reacts with formidase to produce kyn.9,10) IDO is distributed in many tissues, and is strongly induced by infections and inflammation, significantly increasing tryptophan metabolism.11,12) Indeed, increased IDO activity is observed in patients with CKD,13,14) and it has also been reported that the blood kyn level is positively correlated with the progression of CKD.15,16) In addition, kyn is not only eliminated from the body by urinary excretion, but also degraded by kynureninase, an enzyme, to reduce blood levels. In this regard, decreased activity of kynureninase has been reported in patients with CKD.15) Therefore, the blood concentration of kyn is considered to be markedly increased in CKD due to two factors: decreased urinary excretion of kyn and inhibition of its degradation.
In disease conditions, the body is chronically exposed to oxidative stress due to the increased production of reactive oxygen species (ROS) and decreased production of antioxidants,17) which leads to vascular endothelial dysfunction defined as decreased nitric oxide (NO) bioavailability.18,19) NO produced in the vascular endothelium activates soluble guanylate cyclase (sGC) to generate cyclic 3′,5′-guanosine monophosphate (cGMP), which exerts vasodilatory20) and anti-inflammatory effects.21) However, in the presence of an excess of superoxide anion (O2·−), a type of ROS, O2·− traps NO and inactivates it.22,23) In fact, it has been reported that the reduction of NO-mediated vasodilation in patients with greater oxidative stress was markedly improved by administrating ascorbic acid, an antioxidant.24) These evidences indicate the great importance of the imbalance between ROS and NO in the pathogenesis of vascular endothelial dysfunction.
Plasma kyn levels in patients with ESRD are positively correlated with endothelial dysfunction markers, such as soluble intercellular adhesion molecule-1 (sICAM-1) and von Willebrand factor (vWF),25,26) suggesting that kyn is toxic to the vasculature. In addition, kyn is also known to promote ROS production via binding aryl hydrocarbon receptor (AhR). However, the direct influence of kyn on vascular function and ROS production in thoracic aorta have not been clarified. Since regulation of vascular tone is critical for maintaining cardiovascular homeostasis in vivo, this issue is of great importance from the viewpoint of vascular physiology. In the present study, we evaluated whether kyn affects vasorelaxation through the NO/sGC pathway and whether its underlying mechanism is related to increased O2·− production.
Male Sprague–Dawley rats (total 59 rats) were purchased from Japan SLC, Inc. (Shizuoka, Japan). Rats were housed with access to food and water ad libitum. This study involving animals was approved by the Experimental Animal Committee at the Faculty of Pharmacy, Osaka Medical and Pharmaceutical University (Permission Code: 6, Permission Date: 31 March, 2020).
Ex Vivo Organ Bath StudiesThe measurement of vascular reactivity in rat thoracic aortas was described previously.27) The thoracic aortas from rats were cut into approximately 3–5-mm-long ring segments. Each ring was suspended in an organ bath (10 mL) containing Krebs–Ringer bicarbonate solution with the following composition (mM): NaCl 118.5, KCl 4.7, MgSO4 1.2, CaCl2 2.5, NaHCO3 25, glucose 10 and KH2PO4 1.2. The solution was bubbled with 5% CO2 and 95% O2 (37 °C). The changes in the vascular tone tension in response to various vasoactive substances were recorded using a force transducer (MLT0420, AD Instruments, Sydney, Australia). A computer-assisted data acquisition system (PL3508, AD Instruments) recorded the changes in isometric tension during the experiments. Before the formal experiment, the rings in which the resting tension was adjusted to 1.5 g were equilibrated for 60 min after suspension, during which time the solution was replaced every 15 min. After the tension of the rings was becoming stable, the functional endothelium was judged to be intact when marked relaxation (more than 80%) occurred in response to acetylcholine (ACh) (1 µM) in the rings precontracted with phenylephrine (Phe, 1 µM). In some experiments, vascular endothelium was removed by rubbing the aortic lumen with a cotton ball before placing the aortic rings in organ bath chambers. The absence of ACh (1 µM)-induced relaxation indicated endothelium removal.
The aortic ring was incubated with kyn (10, 100, and 500 µM, 30 min or 2 h) or vehicle (Krebs solution). After incubation with kyn or vehicle, the aortic ring was contracted with Phe (1 µM). After the contraction by Phe reached a plateau, each vasodilator (ACh [10−9–10−5 M)], sodium nitroprusside (SNP) [10−9–10−5 M)], BAY 41-2272 [10−10–10−5 M)] and forskolin [10−9–10−5 M)]) was applied in cumulative concentrations. The vasorelaxation response to vasodilators were presented as a percent relaxation of Phe-induced precontraction. Furthermore, in order to identify the mechanism of kyn-induced vascular dysfunction, the antioxidant ascorbic acid (100 µM), the AhR inhibitor CH223191 (10 µM) and the reduced nicotinamide adenine dinucleotide phosphate (NADPH) oxidase inhibitor apocynin (100 µM) were added 30 min before the addition of kyn and even incubation during the kyn procedure.
Assay of O2·− ProductionLevels of O2·− in the aortic ring was determined by measuring lucigenin-enhanced chemiluminescence using a luminometer (Lumat 3, BELTHOLD TECHNOLOGIES, Schwarzwald, Germany). The method of producing an aortic ring was the same as above. Just after, aortic ring segments transferred to test tubes containing Krebs–N-(2-hydroxyethyl)piperazine-N′-2-ethanesulfonic acid (HEPES) buffer (99.01 mM NaCl, 4.69 mM KCl, 1.87 mM CaCl2, 1.2 mM MgSO4, 1.03 mM K2HPO4, 25 mM Na–HEPES and 11.1 mM glucose, pH 7.4, 37 °C), which were bubbled with a 95% O2 and 5% CO2 gas mixture. The aortic ring was exposed for 2 h to kyn (100 µM) or vehicle in Krebs–HEPES buffer. After incubation, lucigenin (5 µM) was added to the test tube in a luminometer. The O2·− production level was expressed in relative light units (RLU)/min/mg dry tissue weight. In the experiment using pretreatment drugs, ascorbic acid, CH223191 and apocynin were added 30 min before the addition of kyn and even incubation during the kyn procedure.
DrugsThe following drugs were used: ACh, BAY 41-2272 and SNP (Sigma-Aldrich, St. Louis, MO, U.S.A.); apocynin, forskolin and kyn (Tokyo Chemical Industry Co., Ltd., Tokyo, Japan); dimethyl sulfoxide, lucigenin and Phe (Nacalai Tesque, Inc., Kyoto, Japan); ascorbic acid (Wako Pure Chemical Corporation, Osaka, Japan); CH223191 (Cayman Chemical, Ann Arbor, MI, U.S.A.). Dimethyl sulfoxide was used as a solvent for BAY 41-2272, apocynin, forskolin and CH223191. Krebs–Ringer bicarbonate solution was used to dissolve all other reagents.
Statistical AnalysisAll values were expressed as the mean ± standard error of mean (S.E.M.). Comparison between 2 groups were performed with the unpaired Student’s t-test; comparisons among three or more groups were performed with a one-way ANOVA followed by Dunnett’s test. Differences were considered to be significant at p < 0.05.
We first examined the influence of kyn on vascular endothelial function using ACh, an endothelium-dependent vasorelaxant (Fig. 1). Kyn exposure for 30 min attenuated the reactivity to ACh in a kyn concentration-dependent manner (Fig. 1A). Next, we examined the influence of 2-h exposure to kyn (Fig. 1B). Similar to the 30-min treatment, kyn concentration-dependently attenuated the reactivity to ACh. In addition, the 2-h treatment of kyn resulted in stronger attenuation than the 30-min treatment. Based on these results, the concentration of 100 µM and the exposure to 2 h were selected for subsequent experiments.

Incubation with kyn for (A) 30 min and (B) 2 h. Each point and bar represents the mean ± S.E.M. of 6–8 experiments. * p < 0.05 and ** p < 0.01, compared with vehicle. ACh, acetylcholine; kyn, kynurenine.
We evaluated the influence of kyn on O2·− production in vascular endothelium-intact aorta (Fig. 2). O2·− production in the aorta exposed to kyn was significantly higher than that in the aorta exposed to vehicle. Enhancement of O2·− production by kyn was significantly inhibited by ascorbic acid and CH223191. However, apocynin pretreatment had no effect. It was also confirmed that treatment of each drug alone in the absence of kyn did not affect O2·− production.

Each column and bar represents the mean ± S.E.M. of 5–6 experiments. ** p < 0.01, compared with vehicle and ‡ p < 0.01, compared with kyn. RLU, relative light units; O2·−, superoxide anion; kyn, kynurenine.
The influence of kyn on the ACh-induced relaxation was evaluated in the existence of the same drugs used in Fig. 2 (Fig. 3). The attenuation of the ACh-evoked relaxation associated with kyn addition was markedly improved by ascorbic acid pretreatment. In addition, CH223191 pretreatment slightly improved the response, although not significantly. On the other hand, apocynin pretreatment had no effect.

Each point and bar represents the mean ± S.E.M. of 5–8 experiments. * p < 0.05 and ** p < 0.01, compared with kyn. ACh, acetylcholine; kyn, kynurenine.
We examined the influence of kyn on endothelium-independent and NO-mediated relaxation to assess the site for vascular toxicity of kyn (Fig. 4). Kyn significantly attenuated the SNP-induced relaxation, as evidenced by a rightward shift of the concentration-response curve.

Each point and bar represents the mean ± S.E.M. of 6 experiments. * p < 0.05 and ** p < 0.01, compared with vehicle. SNP, sodium nitroprusside; kyn, kynurenine.
We surveyed whether kyn exposure to vascular endothelium-denuded aorta affects O2·− production (Fig. 5). Kyn addition markedly increased O2·− production in endothelium-denuded vascular rings. This increase was significantly inhibited by ascorbic acid treatment, while apocynin and CH223191 pretreatment showed had no effect.

Each column and bar represents the mean ± S.E.M. of 6 experiments. * p < 0.05 and ** p < 0.01, compared with kyn. RLU, relative light units; O2·−, superoxide anion; kyn, kynurenine.
We also evaluated the effects of drugs on the attenuation of SNP-induced relaxation associated with kyn (Fig. 6). Ascorbic acid significantly suppressed the decrease in SNP-induced vascular relaxation caused by kyn addition. On the other hand, apocynin and CH223191 showed no effect.

Each point and bar represents the mean ± S.E.M. of 5–6 experiments. * p < 0.05 and ** p < 0.01, compared with kyn. ACh, acetylcholine; kyn, kynurenine.
The sGC stimulator BAY 41-2272 has an ability to activate sGC in an NO-independent fashion and therefore was used to examine whether kyn acute treatment affects sGC function (Fig. 7). Kyn did not have any influence on the relaxation induced by BAY 41-2272.

Each point and bar represents the mean ± S.E.M. of 8 experiments. kyn, kynurenine.
We used the adenylate cyclase (AC) activator forskolin to determine the influence of kyn on the relaxant response mediated by the AC pathway (Fig. 8). Kyn did not affect the forskolin-evoked relaxation.
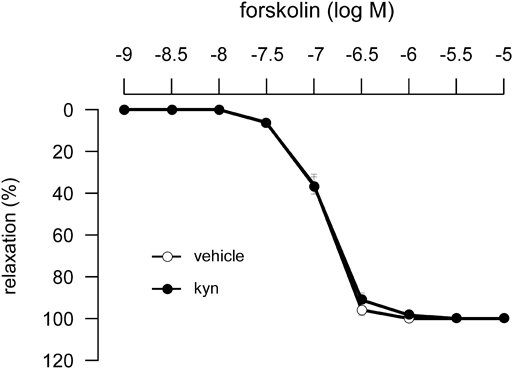
Each point and bar represents the mean ± S.E.M. of 7–8 experiments. kyn, kynurenine.
In this study using isolated rat aortas, we demonstrated that kyn significantly reduces endothelium-dependent relaxation responses. Briefly, kyn attenuated the reactivity to ACh, which was concentration and exposure time dependent. As the ACh-induced vasodilation in rat thoracic aortas was dependent on NO, kyn progressively impairs endothelium-derived NO-mediated vasorelaxation.
High Cu/Zn superoxide dismutase levels, one of the oxidative stress markers, have been reported in association with high blood kyn levels.28) Therefore, we examined the O2·− production following kyn addition in the endothelium-intact aorta. O2·− production in thoracic aorta significantly increased after the addition of kyn. This increase was significantly suppressed by pretreatment with the antioxidant ascorbic acid, and similarly, the reduction of reactivity to ACh associated with kyn was markedly ameliorated. This suggests that the kyn-induced decrease in responsiveness to ACh was due to the excessive production of O2·− production in thoracic aorta.
In an experiment using natural killer (NK) cells, kyn markedly increased ROS production, which in turn induced the apoptosis of NK cells. Furthermore, cell death was inhibited by the suppression of ROS production by NADPH oxidase inhibitor apocynin treatment.29) It is also widely known that the activation of AhR, a cytoplasmic receptor, is closely related to the activation of NADPH oxidase.30,31) Furthermore, kyn has been reported to be a ligand for AhR.32,33) Therefore, we next investigated whether AhR and NADPH oxidase are involved in the increase in O2·− production in the presence of vascular endothelium. Pretreatment with the AhR inhibitor CH223191 significantly inhibited kyn-induced O2·− production and partially recovered the decrease in ACh reactivity. This suggests that kyn stimulates AhR and accelerates O2·− production in endothelium-intact aorta. On the other hand, the NADPH oxidase inhibitor apocynin had no effect on O2·− production and reduced ACh reactivity in response to kyn addition, suggesting that kyn-induced O2·− production does not mediate NADPH oxidase activation. The treatment concentration and time of apocynin used in this experiment were sufficient to inhibit NADPH oxidase.34) In experiments in which vascular endothelial cells were treated with AhR agonist, it has been reported that the mechanism of ROS generation by AhR activation involves the activation of CYP1A1.35) In fact, an acute liver injury model mice with elevated kyn levels in the liver has been reported to have significantly increased CYP1A1 mRNA expression in liver tissue.36) Furthermore, in experiments using HepG2 cells, it has been shown that kyn increases the protein expression of CYP1A1, but the increase is cancelled by the AhR inhibitor CH223191.37) Therefore, kyn may have increased the activity of CYP1A1 after binding to AhR, enhancing ROS production.
We then assessed vascular reactivity to the NO donor SNP using endothelium-denuded vascular rings to confirm whether the site of kyn vascular toxicity is vascular smooth muscle. Kyn markedly reduced SNP-induced vasorelaxation responses. In addition, it increased O2·− production in endothelium-denuded vascular rings. The increase was significantly suppressed by ascorbic acid and the attenuation of SNP-evoked relaxation associated with kyn was also markedly ameliorated. This suggests that kyn induces O2·− overproduction in vascular smooth muscle and causes a decrease in the NO-mediated vasorelaxation response. In vitro studies using primary human aortic vascular smooth muscle cells revealed that kyn increases AhR activity in a concentration-dependent manner, and this increased activity is suppressed by CH223191 pretreatment.32) Therefore, we assessed the effects of CH223191 on the endothelial denuded vascular rings, but CH223191 pretreatment had no significant effects on kyn-induced attenuation of SNP reactivity or O2·− production. This suggests that AhR expressed in vascular smooth muscle is not involved in the O2·− production in endothelium-denuded vascular rings after kyn exposure. There is a report showing that in skeletal muscle, kyn stimulates ROS production independent of AhR activation.38) There may be a possibility that such a pathway is also present in vascular smooth muscle. In any case, as CH223191 significantly suppressed ROS production following kyn treatment in the presence of vascular endothelium, kyn is considered to produce O2·− in vascular endothelium as well as in the vascular smooth muscle. The difference in the contribution of AhR to O2·− production between vascular endothelium and vascular smooth muscle following kyn addition, in addition to the discrepancy with previous studies using cultured cells, may be because the expression pattern of AhR differs in vascular tissue. Although AhR is present in both vascular endothelium and vascular smooth muscle,39) this receptor is reportedly more abundant in the endothelium.40) This may be one of the main reasons. Therefore, we will need to examine where and how much AhR is expressed in blood vessels.
Next, to determine the influence of kyn on sGC function, which functions as a receptor for NO, we used BAY 41-2272, which is capable of activating sGC in a NO-independent manner.41) There are two types of sGC: reduced sGC that can be activated by NO, and oxidized and apo sGC that cannot be activated by NO.42) Under conditions of excess ROS, reduced sGC is converted to oxidized and apo sGC, leading to reduced bioavailability of NO.43) As kyn promotes O2·− production in thoracic aorta, it is possible that reduced sGC becomes oxidized sGC. In the present study, we used the reduced sGC stimulator BAY 41-2272 to examine the influence of kyn on sGC function, but kyn addition did not affect BAY 41-2272-induced vasorelaxation response. This suggests that acute kyn exposure does not affect the redox status of sGC. Thus, the O2·− produced by kyn addition did not affect sGC, but may function in the capture of NO.
To assess the influence of kyn on vascular relaxation other than the NO/sGC pathway-mediated response, we tested forskolin-evoked vasorelaxation that is mediated by the AC pathway. Acute kyn exposure to endothelium-denuded vascular rings had no influence on the forskolin-induced vasorelaxation response. This confirmed that kyn does not affect the vasorelaxation response mediated by the AC pathway.
There are two limitations in this study. First, the kyn concentration used in this experiment is higher than the physiological concentration (about 5–10 µM in patients with CKD)44) and chronic influence also remains unclear. Therefore, measurement of vascular function after long-term kyn administration at or near physiological levels to normal rats will improve our understanding of its pathophysiological role. The second limitation is that we did not address the influence of kyn on endothelial NO synthase (eNOS) expression and activity. Since eNOS plays a very important role in the regulation of endothelial function, it is necessary to examine whether kyn affects eNOS in the future.
In conclusion, we revealed that kyn directly induces vascular dysfunction in rat thoracic aorta. As one of the mechanisms, we found that kyn enhances O2·− production and subsequently scavenges NO, which plays an important role in regulating vascular tone. Therefore, attention should be paid to the vascular toxicity of kyn.
The authors declare no conflict of interest.