2022 Volume 45 Issue 9 Pages 1306-1311
2022 Volume 45 Issue 9 Pages 1306-1311
We aimed to determine the efficacy of zinc acetate hydrate (ZAH) treatment for hypozincemia in elderly inpatients and to identify the factors affecting its therapeutic effect. We enrolled 79 patients with a mean age of 82 years. The mean serum zinc level before ZAH administration was 53.4 ± 11.5 µg/dL. More than half of the patients (67%) had zinc deficiency (<60 µg/dL), whereas 33% had subclinical zinc deficiency (60–80 µg/dL). The median increase in serum zinc level per ZAH tablet (25 mg) was 1.00 µg/dL. Based on the cutoff value, two groups were identified: slight increase (<1.00 µg/dL) and marked increase (≥1.00 µg/dL) groups; the difference between the two groups was significant (0.57 ± 0.22 µg/dL, n = 39 vs. 1.68 ± 0.70 µg /dL, n = 40; p < 0.0001, Wilcoxon rank sum test). Logistic regression analysis using total zinc dose, serum albumin level, impaired renal function, and diuretics as multivariate variables revealed a significant difference in total zinc dose (total number of tablets per 25 mg tablet: odds ratio 1.056, 95% confidence interval 1.019–1.095, p = 0.003). A significant increase in serum zinc levels was observed in the group with a total zinc dose of less than 1000 mg. The results suggest that an increasing trend in total zinc dose is associated with a low increase in serum zinc levels. Therefore, for the treatment of zinc deficiency in elderly inpatients, serum zinc levels need to be measured once, at a total dose of 1000 mg after initiation of ZAH.
Zinc is an essential trace element in living organisms. Approximately 10% of all proteins encoded by the human genome are zinc-containing proteins. The regulation of various physiological activities including growth, skin metabolism, reproductive functions, skeletal development, maintenance of taste, mental and behavioral functions, and immune functions in children are controlled by zinc enzymes.1–3) Zinc is involved in the synthesis and release of insulin from pancreatic beta cells, which show the highest zinc content in vivo.4) Furthermore, zinc enzymes play an important role in ammonia metabolism in the liver.5)
Yasuda and Tsutsui measured age-specific zinc concentrations in hair and reported that the proportion of zinc deficiency increased with age, 20–30% of elderly individuals were zinc deficient, and the elderly were at a higher risk of zinc deficiency.6) Furthermore, a study on people aged ≥60 years (n = 853) from five European countries showed that 31% of the total population was zinc deficient.7) In particular, hypozincemia in the elderly is caused not only by inadequate zinc intake but also by impaired zinc absorption from the gastrointestinal tract. In Japan, zinc deficiency is diagnosed as subclinical zinc deficiency when serum zinc levels are within the range of 60–80 µg/dL and as true zinc deficiency when serum zinc levels are less than 60 µg/dL.8) In the Kitamimaki area, Nagano Prefecture, Japan, the serum zinc concentrations in adults (518 cases) were reported to be below the lower limit of normal (65 µg/dL) in approximately 20% of cases.9)
In Japan, zinc acetate hydrate (ZAH) is indicated by insurance to treat hypozincemia. Hosono et al. investigated the factors affecting the improvement of serum zinc levels in zinc replacement therapy for elderly patients in outpatient and inpatient settings.10) However, there have been no studies of diurnal variation in serum zinc levels or the effect of dietary zinc intake in only elderly inpatients. Diurnal variations exist in serum zinc levels.11) In the case of inpatients, blood sampling time before breakfast is a constant throughout the day, and the intake of zinc derived from meals can maintain a constant serum zinc level, minimizing variations. Thus, clarification of the appropriate dose, duration of administration, and time of testing of ZAH treatment in elderly inpatients would contribute to establishing optimal drug therapy for zinc deficiency.
In this retrospective analysis, we aimed to determine the efficacy of ZAH in the treatment of hypozincemia in elderly inpatients and identified the factors affecting its therapeutic effect.
This multicenter retrospective study was conducted with the approval of the Ethics Committee of Juntendo Tokyo Koto Geriatric Medical Center (Approval No. 104-11) and the Ethics Committee of Nihon University School of Pharmacy (Approval No. 19-013). The analytical data of this study were strictly managed to prevent leakage to outside parties and were used only for the purpose of this study, in compliance with the “Guidelines for the Appropriate Handling of Personal Information by Medical and Nursing Care Providers.”
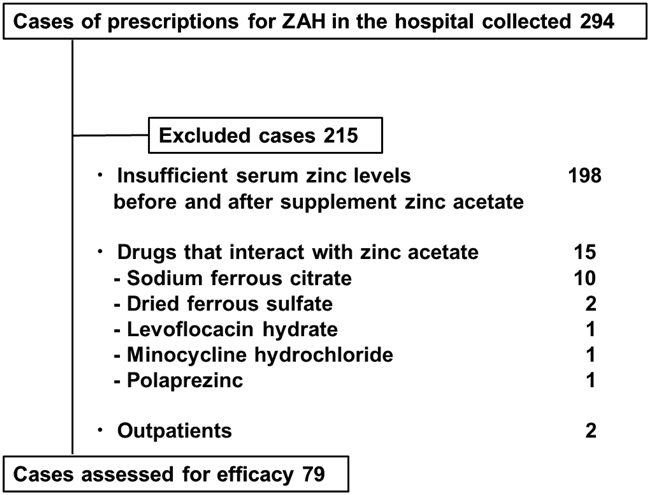
Eligible Patients and Exclusion CriteriaThe eligibility criteria included treatment with ZAH (Novelzin® Tablets, 25 mg, Nobelpharma K.K., Tokyo, Japan) for hypozincemia between December 2017 and March 2020 at Juntendo Tokyo Koto Geriatric Medical Center, Tokyo, Japan. The exclusion criteria were as follows: patients whose serum zinc level was not measured before and after treatment; patients receiving concomitant polaprezinc, tetracyclines, fluoroquinolones, cefdinir, iron formulations, bisphosphonates, eltrombopag olamine, and dolutegravir sodium; and patients defined as outpatients.
SurveyPatient BackgroundPatients’ sex, age, body weight, daily dose of ZAH, history of usage of acid-suppressing drugs and diuretics, main diseases that led to ZAH administration, and time of serum zinc level measurement before and after ZAH administration were investigated.
Clinical FindingsSerum zinc was measured by the colorimetric method, using Acuras Auto Zn (Sinotest, Tokyo, Japan) as the measuring reagent and LABOSPECT 008 (Hitachi High-Technologies, Tokyo, Japan) as the measuring instrument. Serum zinc concentrations after the start of ZAH administration were used the initial values in the measurement. The measurements were performed in the morning. The lower limit of quantification of serum zinc level was 4.0 µg/dL. Serum albumin level, serum creatinine level, and estimated glomerular filtration rate (e-GFR), extracted from the electronic medical records of clinical examination, were recorded.
Evaluation of Serum Zinc Level Improvements Following Administration of ZAHThe following equation (equation 1) was used to calculate the increase in serum zinc (µg/dL) per ZAH tablet (25 mg) to standardize the number of days and doses given for each patient:
 | (1) |
Univariate logistic regression analysis was performed to explore factors affecting serum zinc levels with ZAH administration.10) Patients were divided into markedly and slightly increasing groups, with a median cut-off value of increased serum zinc levels per ZAH tablet (25 mg) as the dependent variable. The independent variables were sex, age, body weight, total dose per 25 mg ZAH tablet (1 tablet), serum albumin level, pre-treatment serum zinc level, impaired renal function group (Stage G4&G5: defined as e-GFR <30 mL/min using Chronic kidney disease, CKD classification), and concomitant medication history (acid secretion inhibitors and diuretics).
Multivariate logistic regression analysis was performed using factors with a significance of p < 0.1 in the univariate logistic regression analysis. JMP Pro ver. 16.0.0 (SAS Institute Inc., NC, U.S.A.) was used for statistical analysis, and the significance level in the final logistic regression analysis was set at a risk rate of p < 0.05.
The process of patient selection in this study is shown in Fig. 1. Of the 294 patients administered hospital-prescribed ZAH, 215 met the exclusion criteria. The most common exclusion criteria were no measurement of serum zinc levels before and after ZAH administration (198 patients), followed by concomitant use of drugs that interacted with ZAH (15 patients). Finally, 79 patients were included in the study.
The background of the patients (n = 79) enrolled in this study is shown in Table 1. Thirty-eight patients (48%) were male and 41 (52%) were female. Patients were aged 82 ± 9 years, with an average body weight of 50.9 ± 13.5 kg and serum albumin levels of 2.8 ± 0.6 g/dL. CKD Stage G4&G5 was observed in 26 cases (32.9%). On an average, the daily dose was 52.6 ± 18.0 mg, and the dose according to the package insert (25–50 mg twice daily, up to three times) was administered for 16.6 ± 10.6 d. Zinc deficiency (<60 µg/dL) and subclinical zinc deficiency (60–80 µg/dL) were present in 53 (67%) and 26 (33%) patients, respectively, and more than half of the patients were zinc deficient. Serum zinc levels before ZAH administration were 53.4 ± 11.5 µg/dL, and population distribution in serum zinc levels before ZAH administration in the elderly inpatients included in this study are shown in Fig. 2.
| Characteristic | |
|---|---|
| Number of male patients | 38 (48%) |
| Age | 82 ± 9 (50–98) |
| Body weight (kg) | 50.9 ± 13.5 |
| Serum albumin (g/dL) | 2.8 ± 0.6 |
| e-GFR (mL/min) | 59.4 ± 47.1 |
| CKD stage G4&G5 (e-GFR <30 mL/min) | 26 (32.9%) |
| Average of daily zinc dose (mg/d) | 52.6 ± 18.0 |
| Administration period (d) | 16.6 ± 10.6 (5–51) |
| Number of days from the date of the pre-administration test to the date of administration (d) | 6.3 ± 6.0 (1–32) |
| Νumber of zinc deficiency (<60 µg/dL) | 53 (67%) |
| Number of marginal zinc deficiency (60–80 µg/dL) | 26 (33%) |
| Serum levels of zinc before supplement zinc acetate (µL/dL) | 53.4 ± 11.5 |
Each value represents the mean ± S.D., the number of patients with the percentage or ranges in parentheses. CKD: chronic kidney disease, e-GFR: estimated glomerular filtration rate.
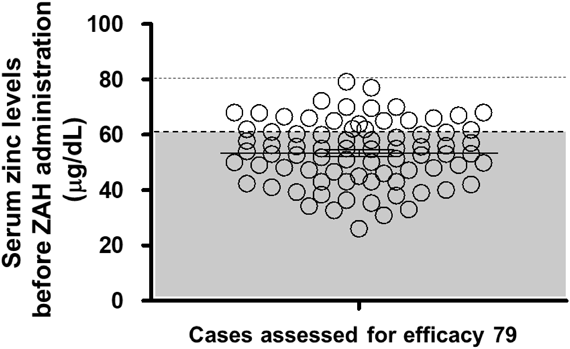
The dotted lines and the gray area in the figure indicate subclinical zinc deficiency (60–80 µg/dL) and zinc deficiency (<60 µg/dL).
Figure 3 shows the diseases that required treatment with ZAH. All patients (n = 79) exhibited low serum zinc levels, with hypozincemia being the most common cause (n = 30, 38.0%), followed by anorexia (n = 21, 26.6%). Other common causes were anemia (n = 9, 11.4%), bedsore (n = 8, 10.1%), infection (n = 6, 7.6%), and dysgeusia (n = 5, 6.3%).
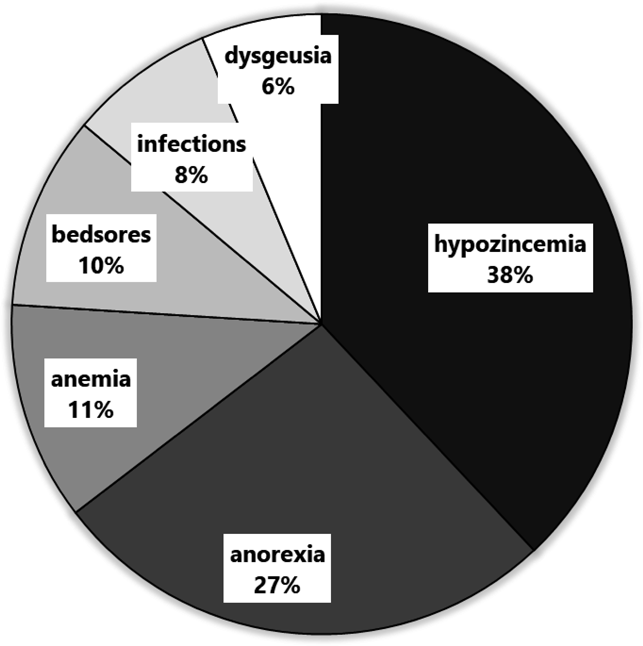
Table 2 shows drugs administered in combination with ZAH. More than half of the patients (n = 42, 53.2%) were prescribed acid-suppressing drugs, like proton pump inhibitors. Diuretics were used concomitantly in 31 patients (39.2%), with azosemide being the most commonly used.
| Drug | Use of percentage | Number of patients |
|---|---|---|
| Use of gastric acid secretion suppression drugs | 53.2% | 42 |
| Kinds of gastric acid secretion inhibitor drugs | ||
| Proton pump inhibitors | 26 | |
| Potassium-competitive acid blocker | 12 | |
| Histamine H2-receptor antagonists | 4 | |
| Use of diuretics | 39.2% | 31 |
| Kinds of diuretics | ||
| Azosemide | 16 | |
| Furosemide | 15 | |
| Spironolactone | 9 | |
| Tolvaptan | 7 | |
| Torsemide | 2 | |
| Thiazide | 2 | |
| Carperitide | 2 | |
| Eplerenone | 1 |
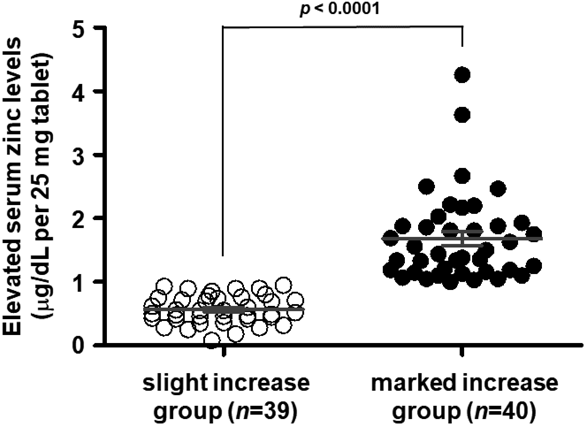
The mean increase in serum zinc (µg/dL) per ZAH tablet (25 mg) calculated from equation 1 is shown in Fig. 4. The median increase in serum zinc was 1.00 µg/dL, and the cutoff value was divided into the slight increase group (<1.00 µg/dL, n = 39) and the marked increase group (≥1.00 µg/dL, n = 40). The difference between the two groups was significant (mean ± S.D. 0.57 ± 0.22 µg/dL, n = 39 vs. 1.68 ± 0.70 µg/dL, n = 40; p < 0.0001, Wilcoxon rank sum test).
In each univariate logistic regression analysis, factors with a risk ratio of p < 0.1 were extracted, including total dose, serum albumin level, impaired renal function, and concomitant use of diuretics (Table 3). Multivariate logistic regression analysis of the extracted factors revealed a significant difference in total dose (total number of tablets per 25 mg tablet: odds ratio 1.056, 95% CI 1.019–1.095, p = 0.003). Serum zinc levels tended to not increase as the total dose of ZAH increased (Fig. 5).
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| Crude OR | 95%CI | p-Value (* p < 0.1) | Adjusted OR | 95%CI | p-Value (** p < 0.05) | |
| Male (vs. Female) | 1.287 | 0.531–3.116 | 0.577 | |||
| Age per years | 0.976 | 0.926–1.029 | 0.372 | |||
| Body weight per kg | 1.024 | 0.989–1.061 | 0.185 | |||
| Total dose (total numbers of tablets per 1 tablet = 25 mg) | 1.056 | 1.021–1.092 | 0.002 * | 1.056 | 1.019–1.095 | 0.003** |
| Serum albumin per g/dL | 0.497 | 0.220–1.125 | 0.093 * | 0.456 | 0.170–1.224 | 0.119 |
| Serum level of zinc before supplement ZAH per µg/dL | 1.009 | 0.971–1.049 | 0.638 | |||
| CKD stage (Stage G4&G5 vs. Stage G1–3) | 0.315 | 0.116–0.854 | 0.023 * | 0.725 | 0.194–2.705 | 0.632 |
| Use of acid secretion inhibiting drug (vs. none) | 0.702 | 0.289–1.705 | 0.435 | |||
| Use of diuretics (vs. none) | 0.393 | 0.155–0.999 | 0.050 * | 0.564 | 0.159–2.006 | 0.376 |
OR: odds ratio, CI: confidence interval, CKD: chronic kidney disease.
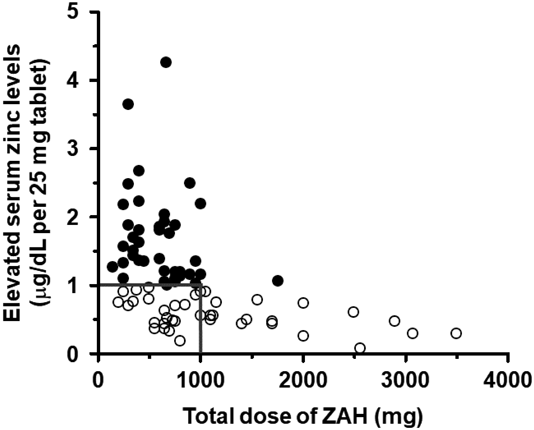
The opened and the closed circles represent the groups showing slight and marked increase, respectively. the gray line in the figure indicates the lack marked increased in patients within the total dose range of 1000 mg.
In this retrospective analysis, we aimed to explore the efficacy of ZAH and the factors affecting its replacement therapy for hypozincemia in elderly patients. The elevated serum zinc level (µg/dL), per tablet (25 mg) of ZAH, was found to be approximately three-fold higher in the markedly increased group (1.68 µg/dL) than in the slightly increased group (0.57 µg/dL) (Fig. 4). In addition, we identified the total dose (total number of tablets per 25 mg: odds ratio 1.056) as a new factor affecting the ZAH replacement therapy (Table 3).
Zinc is primarily absorbed in the duodenum and jejunum,12,13) with an absorption efficiency of approximately 20–40%; however, this rate decreases with increasing zinc intake. Therefore, the mechanism of zinc absorption best fits the saturation response model.14) In this model, the amount of zinc absorbed increases gradually until it reaches the physiological requirement that the organism needs to replenish, after which its absorption declines rapidly. Hambidge et al. modeled this phenomenon in adults.15) Liuzzi et al. demonstrated that this phenomenon is due to upregulation and downregulation of zinc transporters and other proteins involved in the small intestinal transport of zinc in rats.16,17) In the present study, the total dose of zinc (600 mg as an average) tended to be lower in the group with a marked increase in serum zinc levels, while the total dose (1200 mg as an average) tended to be higher in the group with a slight increase (data not shown). Our present results support those of previous studies of a saturation response model of zinc absorption. A unique feature of our study is that we included elderly patients during hospitalization, which allowed us to minimize the effects of dietary zinc intake and substances that inhibit zinc absorption, such as phytic acid, among individual patients.18) As a result, we were able to reliably identify factors influencing the increase in serum zinc levels.
Patients with impaired renal function (CKD stage G4&G5) exhibited significantly different levels of factors affecting the increase in serum zinc levels, as confirmed by considering ZAH in the univariate analysis (p = 0.023); however, there was no significant difference in the multivariate analysis (Table 3). Okamoto et al. reported that the response of serum zinc levels to zinc therapy in maintenance hemodialysis patients was slower in those with higher pre-dialysis serum creatinine levels than in those with lower pre-dialysis creatinine levels.19) They investigated the response of serum zinc levels to the use of an exchangeable zinc pools (EZP). EZP are mathematical estimates of the mass of zinc compartments in the body that rapidly exchange with plasma zinc, and previous studies have identified a positive correlation between EZP and body weight.20) This has been speculated to be due to the positive correlation between body weight and pre-dialysis serum creatinine levels, combined with the fact that patients with higher pre-dialysis serum creatinine levels have larger EZP. However, in the present analysis, only 3 of the patients with CKD stage G4&G5 (n = 26) were receiving dialysis, and the majority were patients with CKD stage G4&G5 without renal replacement therapy (patients with conservative stage CKD). Hypozincemia commonly occurs in patients with CKD due to inhibition of zinc absorption.21) Thus, our results suggest that patients with impaired renal function may have higher zinc deficiency, and higher zinc absorption may be required to saturate this deficiency.
For concomitant medications with ZAH, diuretics did not affect the elevated serum zinc levels per 25 mg of ZAH (Table 3). Chiba et al. concluded that the concomitant use of diuretics, particularly spironolactone and zinc preparations such as polaprezinc and ZnSO4 in cirrhotic patients, may affect serum zinc levels by causing increased zinc excretion.22) By contrast, Ozeki et al. reported that diuretic administration had no effect on the normalization of serum zinc levels by ZAH administration in patients with cirrhosis.23) Therefore, the combination of ZAH and diuretics is unlikely to affect the increase in serum zinc levels in patients other than those with cirrhosis.
Serum albumin did not modulate the increase in serum zinc levels which occurred following ZAH administration (Table 3). Impaired zinc absorption has been reported in patients with liver cirrhosis,24,25) while another study indicated that a serum albumin level of more than 3.3 g/dL is a factor contributing to the normalization of serum zinc levels after 3 months of ZAH treatment in patients with liver cirrhosis.23) Zinc is an essential cofactor in multiple enzyme functioning in the urea circuit of ammonia metabolism. Zinc deficiency results in hyperammonemia owing to decreased enzyme activity resulting in failures in ammonia breakdown.26,27) Consumption of branched-chain amino acids is increased to process this excess ammonia, resulting in a decreased ability to synthesize albumin. Therefore, a decrease in albumin causes a relative increase in zinc bound to amino acids, and the zinc bound to amino acids is excreted in the urine, resulting in a decrease in zinc.25,28) Only one of the patients involved in the study had cirrhosis, suggesting that the effect of serum albumin is small in elderly patients without cirrhosis.
In this study, patients (n = 53) with zinc deficiency (<60 µg/dL) showed an improvement to normal serum zinc levels in 43% (n = 23) of patients taking ZAH (data not shown). The median duration of treatment was 18 d (data not shown). Furthermore, in the markedly increased group, the total dose was generally below 1000 mg, whereas in the slightly increased group, the total dose was predominantly greater than 1000 mg (Fig. 5). If a starting ZAH dose of 50 mg per day is administered, the total dose will be 1000 mg after 20 d of treatment. Therefore, it is necessary to evaluate the serum zinc level to confirm the improvement of zinc deficiency at approximately 20 d after initial administration. The increase in serum zinc levels per ZAH tablet (25 mg) is low as a therapeutic efficiency because the increase in serum zinc levels is gradual as the total dosage of ZAH increases. However, increasing doses of ZAH increase serum zinc levels until saturation is reached.29) The efficiency of zinc absorption from supplements is much higher than that from diets not containing substances that inhibit zinc absorption.30)
This study had several limitations. First, it was difficult to accurately assess zinc intake and nutrition status from intravenous nutrition, enteral nutrition and dietary supplement even in hospitalized patients. Therefore, the effects of such intake could not be completely excluded in individual cases. Since hypozincemia is more likely to occur in patients with conditions such as diabetes and chronic inflammatory bowel disease,31,32) future studies are needed to examine the effect of these underlying conditions on the efficacy of ZAH. Furthermore, because this was a retrospective study, the dose and duration of ZAH administration were not homogenized. Therefore, we were unable to investigate the effect of ZAH on the improvement of hypozincemia in elderly patients. Further studies are required to analyze the effect of ZAH dose and duration on the improvement of hypozincemia in elderly inpatients. From the viewpoint of the appropriate use of ZAH for hypozincemia, it is difficult to predict the exact dose and duration of ZAH administration, but it is recommended to measure the serum zinc concentration when the total dose reaches 1000 mg after the start of ZAH administration to prevent unnecessary medication and side effects.
In this study, we retrospectively analyzed the effect of ZAH administration on serum zinc levels in elderly inpatients with hypozincemia and the factors affecting the increase in serum zinc. The elevation in serum zinc levels per ZAH tablet (25 mg) in elderly inpatients was divided into two groups: a slight increase group and a marked increase group; the increase in the marked increase group was approximately three times higher than that in the slight increase group. Furthermore, we identified that the total dose of ZAH was an important factor affecting the serum zinc level in the elderly and found that the serum zinc level did not greatly increase as the total dose of ZAH increased. These results suggest the need to measure serum zinc levels once at a total dose of 1000 mg after initiation of ZAH for optimizing the treatment of zinc deficiency in elderly inpatients.
We would like to thank Dr. Koichi Ono, Department of Ophthalmology, Juntendo Tokyo Koto Geriatric Medical Center for advice in the statistical analysis of this study.
The authors declare no conflict of interest.