2023 年 46 巻 1 号 p. 19-25
2023 年 46 巻 1 号 p. 19-25
Various factors affect the prognosis of dialysis patients. Analysis of the drugs used and clinical and demographic characteristics of the patient at the time of dialysis initiation is a useful means of estimating prognosis. In this study, we investigated the drugs used by dialysis patients during the induction phase of dialysis and performed a detailed analysis of variables predictive of prognosis. Patients who underwent dialysis between June 1998 and January 2019 and died during this period were included in the study (n = 118). The induction phase of dialysis was defined as the first month after dialysis began. Dialysis duration was defined as the time between dialysis initiation and death. A univariate regression analysis was performed, with dialysis duration as the objective variable and the drugs used during the induction phase of dialysis, blood laboratory values, age at start of dialysis, sex, body height, body weight, medical history and cause of death as the explanatory variables. In addition, multiple logistic regression analysis with stepwise variable selection of significant factors was performed to determine the factors related to dialysis duration. Antihypertensives, hemoglobin (Hb), and age at start of dialysis were found to have significant effects on dialysis duration. It was posited that antihypertensives prolong dialysis duration, thereby improving life expectancy. The regression model developed allowed estimation of prognosis based on the drugs used during the induction phase of dialysis and patient characteristics. These findings may be used to improve drug adherence in dialysis patients and guide physicians in their treatment.
Kidney failure is a major health issue worldwide. Chronic kidney disease (CKD) affects a large number of people worldwide, and more than 2 million people worldwide are treated with dialysis or kidney transplantation.1) The number of chronic dialysis patients in Japan is on the rise, exceeding 340000 in 2020, which constitutes approximately 2700 people per million of the Japanese population.2) The life expectancy of dialysis patients varies and can be affected by various factors. Healthcare providers must strive to improve the survival rate and duration, and the QOL of dialysis patients. However, since many dialysis patients must take a wide variety of drugs over a long duration of time to prevent and treat complications, it can be difficult to determine the factors that affect life expectancy.3)
Prediction of life expectancy in CKD patients4–6) prediction of life expectancy in renal replacement therapy patients,7) and prediction of life expectancy in chronic dialysis patients have been reported.8,9) Floege et al. reported cardiovascular disease, cancer complications, albumin levels, and ferritin levels as predictors of life expectancy.8) The main goal of dialysis is to save lives. Dialysis induction generally occurs when renal failure has progressed sufficiently to produce uremic symptoms that make daily life difficult. However, as the long-term survival of patients with end-stage kidney disease becomes more common, consideration of life expectancy after dialysis induction has become important.10)
Although the drugs used and patient variables at the time of dialysis induction are considered a useful means of estimating life expectancy, there has been limited research into the impact of these factors on life expectancy. Therefore, in this study, we attempted to determine the factors that affect life expectancy by examining patient characteristics and the drugs used by patients during the induction phase of dialysis.
For each patient, data were collected from medical records regarding the dialysis duration, age at start of dialysis, sex, body height, body weight, medical history, drugs used during dialysis induction, blood laboratory values, and cause of death. Patient records came from four facilities of Zelkova Medical Corporation: Kita-Hachioji Clinic, Kodaira Kitaguchi Clinic, Higashi Kurume Clinic, and Higashi Yamato Nangai Clinic. Patients who underwent dialysis and died between June 1998 and January 2019 were included in this study. The four facilities of Zelkova Medical Corporation cannot perform shunt creation surgeries. Therefore, eligible patients have shunt creation surgery at facilities other than the four facilities. Medical data were collected on the patients’ first visits to the four facilities of the Zelkova Medical Corporation during the induction phase of dialysis. Medical data collected from other facilities at the time of dialysis induction were excluded. Four patients were thus excluded. The study was approved by the Ethical Review Committee of Meiji Pharmaceutical University (Approval No. 3021). The study involved no interventions and the data were anonymized so patient consent was not required.
Data Collection and Evaluation of Clinical ParametersAll data were collected retrospectively from medical records. The induction phase of dialysis was defined as within 1 month of dialysis induction. Dialysis duration was defined as the dialysis start date to the date of death (in years) (Fig. 1).

The induction phase of dialysis was defined as within 1 month from the date of dialysis induction. The objective variable of this study was the dialysis duration. The dialysis duration was defined as the date of death minus the date of dialysis induction (in years).
The relationship between dialysis duration and the population of dialysis patients in Japan has decreased by half over a 5-year period.2) The objective variable, dialysis duration, was divided into two groups: those on dialysis for less than 5 years and those on dialysis for more than 5 years. Medical history data and the cause of death were classified according to the International Classification of Diseases, 10th Edition (ICD-10).11) Drugs were classified according to the Japan Standard Commodity Classification.12) In the analysis of blood laboratory values, laboratory values with missing values exceeding 70% of the total number of patients were deleted, and missing values were supplemented with median values. Blood urea nitrogen (BUN), serum creatinine (Cr), and uric acid values were excluded from our analysis, as they are urea toxin substances that are filtered by dialysis so their values differ a great deal before and after dialysis. The medical data collected from the patients’ first visit to the four facilities during the induction phase of dialysis included medical history and drug use. This medical data did not include the information recorded at other hospitals.
Statistical AnalysisFisher’s exact test was used for the comparison of categorical variables. Logistic regression analysis was used to compare continuous variables. Univariate regression analysis was used to identify those variables associated with dialysis duration, with age at start of dialysis, sex, body height, body weight, medical history, drugs used during dialysis induction, blood laboratory values and the cause of death as the explanatory variables. Significant factors were removed by pairwise method13) with Pearson’s coefficient of determination r, r2 > 0.9 as multicollinearity.
 |
Factors that were significant in the univariate regression analysis were evaluated by multivariate logistic regression, with variable selection performed using the stepwise method (forward-backward method). Each candidate factor was evaluated for its receiver operating characteristic (ROC) area under the curve (AUC) (Fig. 2). Data were analyzed using JMP v. 15.2.0 software (SAS Institute Inc., Cary, NC, U.S.A.). p < 0.05 was considered statistically significant.
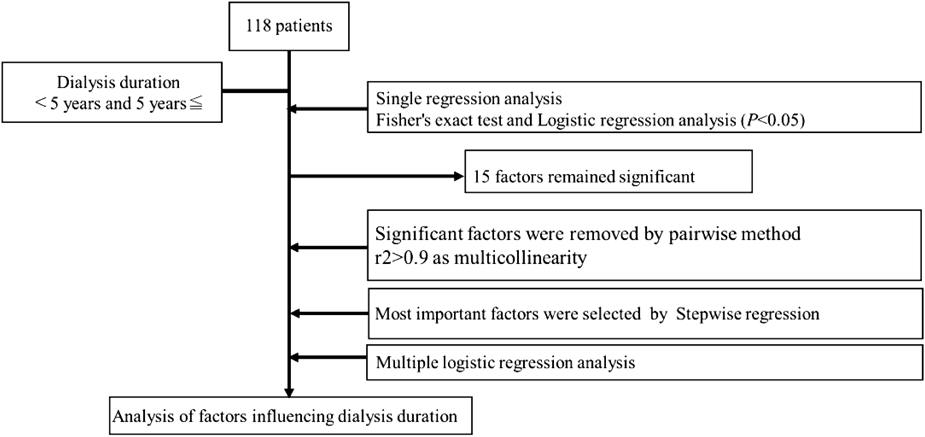
Medical data were collected on 118 patients. The objective variable was categorical variables of dialysis duration < 5 years and > 5 years. Single regression analysis was performed to identify factors associated with dialysis duration; p < 0.05 was considered significant. Factors with Pearson’s coefficient of determination r, r2 > 0.9 were removed. Variable selection was performed using a stepwise method for factors that were significant in the single regression analysis, and multiple logistic regression analysis was performed to analyze factors related to the dialysis duration.
Of the 118 eligible patients, 29 (24.6%) were from the Kita-Hachioji Clinic, 32 (27.1%) were from the Kodaira Kitaguchi Clinic, 30 (25.4%) were from the Higashi Kurume Clinic, and 27 (22.9%) were from the Higashi Yamato Nangai Clinic. The median dialysis duration was 5 years, with a range of 33 d to 19 years. For patients on dialysis for < 5 years and those on dialysis for > 5 years, the following data were collected: age at start of dialysis, body height, body weight, sex (Supplementary Table S1), medical history (Supplementary Table S2), drugs used during the induction phase of dialysis (Supplementary Table S3), laboratory blood values (Supplementary Table S4), and cause of death (Supplementary Table S5). Continuous variables were presented as means and standard deviations (S.Ds.), and categorical variables were presented as frequencies (n) and percentages (%). Patients’ medical record data are presented in Supplementary Table S6.
Univariate Regression Analysis of Factors Affecting Dialysis DurationWe identified 15 variables that significantly affected dialysis duration, which included age at start of dialysis (p = 0.0002, negative effect), body height (p = 0.0101, positive effect), body weight (p = 0.0276, positive effect), diseases of arteries, arterioles, and capillaries (p = 0.0046, negative effect), hypertensive disease (p = 0.0099, positive effect), disorders of kidney and ureter (renal osteodystrophy) (p = 0.0364, positive effect), use of antihypertensives (p = 0.0026, positive effect), use of antiplatelet drugs (p = 0.0050, negative effect), use of erythropoietin (p = 0.0099, positive effect), use of diuretics (p = 0.0112, positive effect), hemoglobin (Hb) (p = 0.0005, negative effect), erythrocytes (p = 0.0005, negative effect), hematocrit (Ht) (p = 0.0006, negative effect), C-reactive protein (CRP) (p = 0.0279, negative effect), and neoplasms (p = 0.0193, positive effect) (Table 1).
| Factors | Dialysis period | p-Value | Effect of the dialysis duration | |
|---|---|---|---|---|
| <5 years (N = 49) | ≥5 years (N = 69) | |||
| Age at start of dialysis (year) | 74.65 ± 9.83 | 66.75 ± 10.16 | 0.0002 | Negative |
| Body height (cm) | 157.73 ± 8.95 | 161.9 ± 7.72 | 0.0101 | Positive |
| Body weight (kg) | 55.65 ± 12.71 | 60.6 ± 10.69 | 0.0276 | Positive |
| Diseases of the arteries, arterioles, and capillaries | 13 (26.5) | 5 (7.2) | 0.0046 | Negative |
| Hypertensive diseases | 33 (67.3) | 60 (87) | 0.0099 | Positive |
| Disorders of kidney and ureter (renal osteodystrophy) | 0 | 6 (8.7) | 0.0364 | Positive |
| Antihypertensives | 30 (61.2) | 59 (85.5) | 0.0026 | Positive |
| Blood and body fluid preparations (antiplatelet drugs) | 25 (51.0) | 18 (26.1) | 0.0050 | Negative |
| Metabolic drugs (erythropoietin preparation) | 33 (67.3) | 60 (87.0) | 0.0099 | Positive |
| Diuretics | 23(46.9) | 48 (69.6) | 0.0112 | Positive |
| Hb (g/dL) | 9.66 ± 1.13 | 8.81 ± 1.18 | 0.0005 | Negative |
| Erythrocytes (104/µL) | 321.45 ± 52.33 | 286.39 ± 45.04 | 0.0005 | Negative |
| Ht (%) | 30.66 ± 3.97 | 27.88 ± 3.80 | 0.0006 | Negative |
| CRP (mg/dL) | 0.96 ± 1.61 | 0.39 ± 0.69 | 0.0279 | Negative |
| Neoplasms | 1 (2.0) | 10 (14.4) | 0.0193 | Positive |
Single regression analysis showed the significant factors for dialysis duration. Significant factors were described by category. The significant medical history was identified as diseases of arteries, arterioles, and capillaries, hypertensive diseases, and disorders of the kidney and ureter (renal osteodystrophy). Significant drugs used included antihypertensives, blood, and body fluid preparations (antiplatelet agents), metabolic drugs (erythropoietin preparation), and diuretics. Significant blood laboratory values were Hb, erythrocytes, Ht, and CRP. The significant cause of death was neoplasm.
Pearson’s coefficient of determination, r2, for Hb and Ht was 0.91, which was considered multicollinear as r2 > 0.9; therefore, Ht was removed. Hb, which had a large effect on dialysis duration, was used in the multivariate analysis. Variable selection was performed using a stepwise method for the 14 factors that were significant in the univariate analysis. p-Values were used to evaluate the stepwise method. Four factors were identified by multiple logistic regression analysis: Hb, age at start of dialysis, antihypertensives, and CRP (Table 2).
| Factor | Odds ratio | 95% confidence interval | p-Value |
|---|---|---|---|
| Antihypertensives | 4.020 | 1.297–12.457 | 0.0159 |
| Unit odds ratio | |||
| Factor | Odds ratio | 95% confidence interval | p-Value |
| Hb (g/dL) | 0.366 | 0.224–0.5994 | <.0001 |
| Age at start of dialysis (year) | 0.898 | 0.849–0.950 | 0.0002 |
| CRP (mg/dL) | 0.582 | 0.361–0.939 | 0.0265 |
| Range odds ratio | |||
| Factor | Odds ratio | 95% confidence interval | p-Value |
| Hb (g/dL) | 0.002 | 0.00008–0.03977 | <.0001 |
| Age at start of dialysis (year) | 0.002 | 0.00008–0.05223 | 0.0002 |
| CRP (mg/dL) | 0.016 | 0.00044–0.61988 | 0.0265 |
The odds ratios for factors that affect dialysis duration were calculated. The use of antihypertensives, Hb, age at start of dialysis, and CRP were found to be significant factors that affecting dialysis duration.
The regression model was R2 = 0.323, p < 0.001, ROC AUC = 0.860, and the lack of fit was p = 0.6045. Odds ratios (OR) were calculated for antihypertensives use (OR, 4.020; 95% confidence interval (CI), 1.297–12.457, p = 0.0159), Hb (OR, 0.002; 95% CI, 0.00008–0.03977, p < 0.001), age at start of dialysis (OR, 0.002; 95% CI, 0.00008–0.05223, p = 0.0002), CRP (OR, 0.016; 95% CI, 0.00044–0. 61988, p = 0.0265). Unit OR were also calculated for Hb (OR, 0.366; 95% CI, 0.224–0.5994, p < 0.001), age at start of dialysis (OR, 0.898; 95% CI, 0.849–0.950, p = 0.0002), and CRP (OR, 0.582; 95% CI, 0.361–0.939, p = 0.0265). The unit OR indicates the OR as the explanatory variable that changes by one unit. The range OR indicates the OR as the value of the explanatory variable that changes from the minimum to the maximum value. The use of antihypertensive, Hb levels, age at start of dialysis, and CRP levels were found to significantly affect dialysis duration.
Exclusion of Patients Who Died in the Early Stages of Dialysis Induction and Examination of Factors That Affect the Duration of DialysisThree patients died within 6 months of dialysis induction who were excluded from the 118 eligible patients, bringing the total number of eligible patients to 115. A single regression analysis was performed to identify the significant factors that affect dialysis duration. Similar variables were used for the objective and explanatory variables. Nineteen factors were significant for the duration of dialysis. Fifteen factors (Table 1) were the same as those that were significant for the 118 eligible patients. Four factors were newly identified as significant factors. Significant laboratory values included reticulated red blood cells, chloride, and aluminum. Significant cause of death was respiratory disease. Hb and Ht were significant factors for dialysis duration. Ht was removed because of multicollinearity, and Hb, which exhibited a significant effect on dialysis duration, was used in the multivariate analysis. A stepwise method was used to select variables for the 18 factors that were significant in the univariate analysis. Multiple logistic regression analysis was performed on the three factors. The selected factors were Hb, age at start of dialysis, and antihypertensive use. When patients on dialysis for ≤6 months were excluded and the factors affecting dialysis duration were examined, only CRP was not identified as a significant factor. The regression model showed R2 = 0.285, p < 0.001, ROC AUC = 0.850, and lack of fit p = 0.560. ORs for the factors that affected dialysis duration were calculated (Table 3).
| Factor | Odds ratio | 95% confidence interval | p-Value |
|---|---|---|---|
| Antihypertensives | 4.636 | 1.617–14.551 | 0.0004 |
| Unit odds ratio | |||
| Factor | Odds ratio | 95% confidence interval | p-Value |
| Hb (g/dL) | 0.378 | 0.222–0.5935 | <.0001 |
| Age at start of dialysis (years) | 0.902 | 0.850–0.9486 | <.0001 |
| Range odds ratio | |||
| Factor | Odds ratio | 95% confidence interval | p-Value |
| Hb (g/dL) | 0.002 | 0.00008–0.03737 | <.0001 |
| Age at start of dialysis (years) | 0.003 | 0.00008–0.04680 | <.0001 |
Patients with dialysis duration of ≤6 months were excluded. The odds ratios of the factors that affect dialysis duration were calculated. The use of antihypertensives, Hb, and age at start of dialysis were found to be significant factors that affect dialysis duration.
Our multiple logistic regression analysis found the age at start of dialysis to have a negative effect on dialysis duration. After adjusting for age at introduction to dialysis, antihypertensives, Hb, and CRP remained as factors affecting the dialysis duration (Table 2). There are many reports on age and mortality in maintenance dialysis patients, but few on age at introduction to dialysis and mortality.
Antihypertensives used included angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta blockers, and alpha-beta blockers. Fisher’s exact test was performed to compare ACE inhibitors, ARBs, beta blockers, and alpha-beta blockers for dialysis duration (<5 years vs. ≥5 years). The results of the analysis showed ACE inhibitors (4 vs. 6, p = 0.5975), ARBs (22 vs. 51, p = 0.0013), beta blockers (0 vs. 3, p = 0.1963), and alpha-beta blockers (11 vs. 13, p = 0.3995). ARB was identified as a significant factor for dialysis duration. Our multiple logistic regression analysis found the use of antihypertensives to have a positive effect on dialysis duration. This suggests that the prevention and treatment of hypertension during the induction phase of dialysis is important. This makes sense given that heart failure is the leading cause of death among dialysis patients.2) Heart failure results from increased cardiac burden as a consequence of cardiac hypertrophy in patients with poorly controlled blood pressure and prolonged hypertension. ACE inhibitors and ARBs are used to treat heart failure by lowering blood levels of angiotensin II and aldosterone, which are involved in blood pressure elevation.14) Adrenergic beta-receptor blockers and alpha- and beta-receptor blockers are used to treat heart failure. These drugs improve cardiac function by blocking the action of noradrenaline, reducing the cardiac workload.15,16) Early intervention for hypertensive symptoms in dialysis patients can prevent heart failure, which explains why we found antihypertensive use to contribute to improved life expectancy. Although drug use may affect survival, the presence of comorbidities must also be considered, especially since the relationship between drug use and life expectancy is influenced by comorbidities.
Hb levels at the start of dialysis had a negative effect on dialysis duration. In other words, low Hb at dialysis initiation contributed to longer survival of dialysis patients. This supports the findings of previous research.17) Although the mechanism behind the relationship between low Hb and survival remains unclear, the renal anemia that is characteristic of dialysis patients may be involved. Renal anemia is a condition in which the kidneys are unable to maintain Hb levels due to decreased erythropoietin production as a result of kidney damage. CRA syndrome (cardio-renal anemia syndrome) is a vicious cycle of chronic renal failure, renal anemia, and chronic heart failure often seen in dialysis patients.18) Singh et al. analyzed CKD patients receiving erythropoietin preparation. In those with high Hb levels, they reported an increase in the incidence of cardiovascular symptoms and mortality and a two-fold increase in erythropoietin preparation use compared to those with lower Hb levels.17) Patients on maintenance dialysis may have low Hb levels even when receiving high doses of erythropoietin. Such erythropoietin hyporesponsiveness is thought to predispose the individual to cardiovascular symptoms.19) We speculate that in patients with high Hb levels, erythropoietin hyporesponsiveness may complicate cardiovascular symptoms and worsen life expectancy. In patients with high Hb levels during the induction phase of dialysis, attention to the possibility of erythropoietin hyporesponsiveness may be important to improve prognosis.
The two groups were divided according to the dialysis duration: low Hb group for ≥5 years and high Hb group for < 5 years, with the high Hb group demonstrating the poorest prognosis. Darbepoetin alpha was used as an erythropoietin agent. t-Test was performed on the units of darbepoetin alpha used and the low and high Hb groups, and significant differences were found. The high Hb group used approximately twice as much darbepoetin alpha as the low Hb group (30.0 vs. 54.5, p = 0.0005).
The Japan Erythropoietin Treatment (JET) Study20) is a prospective observational study designed to evaluate the relationship between Hb levels and the prognosis of patients on HD following epoetin beta administration. The JET study compared the prognosis of patients with Hb levels of 11–12 and ≥12 g/dL and reported that 11–12 g/dL was the optimal concentration, with an increased risk of death in the ≥12 g/dL group.20) The high Hb group showed a worse prognosis, whereas the low Hb group showed a better prognosis. This information has been published in the Japanese guidelines.21) The reasons behind the increased risk of death in the high Hb group are discussed below. Elevated Hb levels may induce vascular disease by increasing blood viscosity.22) Despite poor response to erythropoietin preparations, the excessive use of erythropoietin preparations to elevate Hb levels may increase the risk of death.23,24) The results of our analysis support those of this repor.20,21) Conversely, a higher risk of death has been reported in the low Hb group than in the high Hb group.8,9) In a cohort study of patients with chronic dialysis, the life expectancies of each group with Hb levels < 10 and > 10 g/dL were compared and an increased risk of death in the < 10 g/dL group was reported.8) In a randomized controlled trial comparing the risks of developing cardiovascular disease in patients with chronic dialysis, the group at a high risk of developing cardiovascular disease reported lower Hb levels than the group at a low risk of developing the disease.9) The mechanism of poor prognosis caused by low Hb levels in these reports8,9) is unclear, but it is assumed to be related anemia.25) Since the results of this analysis have been reported to be contradictory to those of the present study, we need to carefully investigate the relationship between Hb levels and prognosis in the future.
CRP levels demonstrated a negative effect on dialysis duration. Zimmermann et al. have similarly reported that CRP > 0.8 mg/dL increases mortality from cardiovascular disease in dialysis patients.26) We found CRP levels of 0.96 ± 1.61 (mean ± S.D.) in patients on dialysis for < 5 years supports previous reports26) (Table 1). Inflammation can complicate cardiovascular disease and reduce survival duration. The management of CRP during the induction phase of dialysis may help prevent and treat cardiovascular disease. Patients on dialysis for ≤6 months exhibited severe complications, such as cerebrovascular diseases and neoplasms. One patient had cerebral infarction, including cerebrovascular diseases, and one had pharyngeal cancer that included malignant neoplasms of the lips, mouth, and pharynx (Supplementary Table S2). Patients with CKD have a high mortality rate from cardiovascular diseases.27) Especially, in Japan, CKD has been reported to be a risk factor for cerebral infarction.28) The death of patients after a short period of dialysis may be because of CKD. When patients on dialysis for ≤6 months were excluded and the factors that affected dialysis duration were examined, only CRP was not identified as a significant factor. This suggests that CRP may be related to the pathogenesis of serious cerebrovascular diseases and neoplasms.
The interpretation of high CRP values is complicated by the persistent infection seen in many dialysis patients due to periodontitis, arteriosclerosis, and cardiovascular disease.29) The present study was limited in its CRP data from the induction phase of dialysis. More detailed information about the pathophysiology of CRP is needed and the collection of laboratory data and medical history before dialysis induction and during the preservation phase.
The sample size in this study was small. To increase the sample size, it is necessary to collect data regarding the patients who died during the induction phase of dialysis at other facilities. We evaluated data only for the induction phase of dialysis. In the future, data regarding CKD should also be collected to identify the factors that contribute to deaths from CKD. Prospective studies are warranted to estimate the causal relationship between CKD and mortality. Although drug use may affect survival, the presence of comorbidities also needs to be considered. The relationship between drug use and life expectancy is influenced by comorbidities.
Medical data from dialysis patients from four centers were analyzed. The results of this analysis suggest that the use of antihypertensives during the induction phase of dialysis, along with low Hb may improve life expectancy. These findings may also be useful for estimating life expectancy after dialysis induction and may help improve drug adherence and contribute to treatment guidelines for dialysis patients and their physicians.
We thank our colleagues from Meiji Pharmaceutical University whose insight and expertise greatly assisted this research.
The authors declare no conflict of interest.
This article contains supplementary materials.