2023 Volume 46 Issue 4 Pages 533-541
2023 Volume 46 Issue 4 Pages 533-541
C-C motif chemokine ligand 17 (CCL17), an important chemokine, plays a vital role in regulating immune balance in the central nervous system. In this study, we explored the potential roles of CCL17 in a rat postoperative pain model and that of blocking CCL17 in the prevention of postoperative pain in rats. A right plantar incision in rat was used as a model of postoperative pain. A behavioral change was measured preoperatively and postoperatively using mechanical withdrawal thresholds and thermal withdrawal latency. CCL17 and its upstream Jmjd-3 mRNA levels in the spinal cord were detected using real-time PCR, CCL17 levels in the serum were measured using enzyme-linked immunosorbent assay (ELISA), and the expression of interferon regulatory factor 4 (IRF4), which interacts with Jmjd-3, was detected by immunohistochemistry staining. After that, rats were intraperitoneally injected with either anti-CCL17 monoclonal antibody (mAb) or GSK-J4 (the Jmjd3 inhibitor) to evaluate the protective effects of blocking CCL17 on postoperative pain. We found that CCL17 and Jmjd-3 were significantly increased in the spinal cords of the postoperative pain rat, consistent with changes in hyperalgesia. In addition, our results showed that the mechanical and thermal allodynia was significantly ameliorated using anti-CCL17mAb or GSK-J4. Moreover, we found that anti-CCL17mAb or GSK-J4 treatment decreased c-fos expression in response to peripheral stimulation. Finally, our preliminary exploration found that anti-CCL17mAb or GSK-J4 had a protective effect on tissue damage. These findings indicated that high expression of CCL17 played a critical role in postoperative pain induced by plantar incision and that CCL17 blockade may serve as an effective approach to managing postoperative pain.
Approximately 300 million surgical procedures are performed annually worldwide,1) and even with medication, approximately 40% of patients experience moderate or severe postoperative pain.2,3) In the management of postoperative pain, traditional analgesics and interventions are often ineffective or only partially effective.4–6) Despite the fact that postoperative pain is prevalent, and the pathological mechanism of postoperative pain has been further investigated, inadequate postoperative pain control remains a challenge for physicians.
Chemokines are a class of low molecular weight cytokines that play an important role in the immune system and nervous system.7,8) C-C motif chemokine ligand 17 (CCL17), a specific ligand of CC chemokine receptor (CCR4), was originally implicated in the preferential attraction of Th2 lymphocytes.9–13) There has been considerable evidence that CCL17 is expressed at elevated levels in many inflammatory conditions.14–16) Studies have found that the application of CCL17 drives inflammatory pain in a cyclooxygenase (COX)-dependent manner, while treatment with anti-CCL17 blocks the effects.9) It has been demonstrated that human microglial cells express CCR4, suggesting that CCL17 may also act on microglial cells in a pain-producing manner.17) The interferon regulatory factor 4 (IRF4) is a hemopoietic-specific transcription factor essential for the development and function of myeloid and lymphoid cells. It has been regarded as a signal that reduces inflammation. IRF4 has been identified as an important intermediary in the upregulation of CCL17 expression.18,19) A number of evidence indicate that CCL17, via Jmjd3-IRF4, is involved in inflammation, and that blocking CCL17 can alleviate inflammatory pain and arthritic disease.18,20–22)
As a member of the JmjC family of histone demethylases, Jmjd-3 regulates the expression of correlation genes.23) Furthermore, Jmjd-3 mediates chromatin modifier interactions that activate targeted genes in the absence of its demethylase activity.24) Jmjd-3 expression is normally low in organizations, but it is highly induced by cellular stress.25–27) The jmjd-3 protein plays a crucial role in development, physiology, and disease.24,27,28) The Jmjd-3 specific inhibitor GSK-J4 has been used in targeted pharmacological interventions for the treatment of several mouse diseases.29) It has been demonstrated that Jmjd3 plays a crucial role in the direct regulation of IRF4 and ultimately CCL17. The production of CCL17 was closely related to IRF4 and Jmjd3 in vitro and in vivo studies.30,31) In their study of the mouse model of osteoarthritis (CiOA), Lee et al. demonstrated that CCL17 and IRF4 were important in the occurrence and development of inflammatory pain.8,31,32) The study indicated that therapeutic neutralization of CCL17 and Jmjd3 alleviated pain, and concluded that CCL17 was a potential therapeutic target for the treatment of CiOA pain through the Jmjd3/IRF4 pathway.6,31,32)
As of now, little is known about the effects of CCL17 on postoperative pain. We examined the role of CCL17 in postoperative pain induced by plantar incision in rats and examined the protective effects of blocking CCL17 with ani-CCL17 monoclonal antibody (mAb)/GSK-J4 (the Jmjd3 inhibitor). The findings of this study will provide a novel insight into the mechanism of postoperative pain and a potential therapeutic avenue to treat it.
Adult male Sprague–Dawley rats (250 ± 20 g; 6–8 weeks) were ordered from Jinan Pengyue Animal Breeding Co., Ltd. (Jinan, China). In a controlled environment with constant temperature (20–22 °C) and 12-h/12-h light/dark cycles, rats were housed individually with access to water and food. A week prior to the behavioral procedure, rats were familiarized with the behavioral equipment. National Institutes of Health (NIH) guidelines were followed for all experiment regulations. Moreover, the study was approved by Weifang Medical University’s Laboratory Animal Ethics Committee.
Surgical ProcedureBased on the procedures used by Brennan et al, the rat model of postoperative pain was prepared using the plantar incision (PI) method.33) The rats were anesthetized with sevoflurane. Aseptic preparation of the plantar surface of the right hindpaw was carried out three times with povidone-iodine. After that, a cut was made with a No. 11 blade on the right hindpaw, starting 0.5 cm from the heel and extending to the toes, through the plantar skin and fascia, as well as the underlying muscles. It was necessary to separate the plantar muscles, elevate them slightly, cut them lengthwise, and then reassemble them. Following the bleeding had stopped, the incision sites were sutured with 4-0 silk suture. For the purpose of promoting rat awakening, the rats were kept warm following the operation. Sham operation participants were anesthetized and disinfected without making any incisions on the right hindpaw.
Experimental DesignRats were randomly divided into different groups (n = 7 in each group). The rats in the PI + GSK-J4 group were injected intraperitoneally with GSK-J4 (0.35 mg/kg, R&D, U.S.A.) 30 min prior to surgery. CCL17mAb (16 mg/kg) (R&D) was intraperitoneally administered to rats in the PI + CCL17mAb group 30 min prior to surgery. It was done by dissolving GSK-J4 in dimethyl sulfoxide (DMSO), then diluting the solution with sodium chloride so that the concentration of DMSO would be less than 2%. A day prior to operation, baseline thresholds of rat behavior were determined. Following surgery, the mechanical withdrawal threshold (MWT) and thermal withdrawal latency (TWL) were measured at 2, 4, 8, and 24 h. Following the behavioral tests, CCL17 and Jmjd-3 levels were measured using real-time PCR, enzyme-linked immunosorbent assay (ELISA), and immunohistochemistry, 24 h after the plantar incision. Hematoxylin–eosin (H&E) staining was performed to investigate the protective effect of anti-CCL17mAb or GSK-J4 on tissue damage 24 h after surgery.
Behavioral MeasurementThe MWT was determined using the up-down method, and the range of Von Frey Hairs chosen for measurement was 0.4, 0.6, 1.0, 1.4, 2.0, 4.0, 6.0, 8.0, 10.0, 15.0 (unit: grams).34) Using 2.0 g as a starting point, Von Frey Hairs were vertically stabbed to the rat’s proximal medial position for approximately five seconds. If the rats raised their hindpaws or retreated from the stimulus, it was considered a positive response; otherwise, they were considered to have exhibited a negative response. Rats showed suspicious positive reactions such as walking after the stimulus occurred, and repeated measurements were required with the same value of Von Frey Hairs. As a result of a positive result, the next measurement was conducted using the adjacent filaments of smaller values. As a result, a negative result was obtained; the next test was conducted with filaments of adjacent larger values. It is recommended that there be at least three minutes between measurements. The upper and lower limits of Von Frey Hairs were 0.4 and 15g, respectively. All values were calculated with the formula 50% MWT THRESHOLD = (10[Xf + kδ])/10000, Xf = the logarithm of the last test; k value can be obtained from the withdrawal response pattern table. δ = the mean of the logarithmic differences between groups. Postoperatively, the threshold of mechanical stimulation was measured and calculated based on the above methods at, 4, 8, and 24 h.
A procedure based on Hargreaves et al. was used to determine the TWL.35,36) Rats were caged individually and measured using PL-200 radiant equipment (Taimeng Technology Market Company, China), under natural lighting. It should be noted that the stimulation point was located on the inner side of the proximal incision of the right hindpaw, avoiding the footpad and heel. As soon as the rats lifted the hindpaw during the test, the timing of the device was stopped automatically and the duration of the thermal stimulus was recorded. There should be a minimum three-minute interval between two measurements. The maximum and minimum values of five measurements were removed, and the average value was determined from the remaining values. In order to prevent tissue damage, a maximum cutoff time of 30 s was set. All behavioral tests were carried out by the same person blind to the experimental design.
Real-Time Quantitative PCRSamples were collected 24 h following surgery. A TRIzol reagent (Invitrogen, Thermo Fisher Scientific, U.S.A.) was used to extract RNA samples from the spinal cords of rats. In this study, reverse transcription was carried out using the BeyoRTTTM II cDNA kit (Beyotime Biotechnology, China) according to the manufacturer’s instructions. As part of the real-time quantitative PCR analysis, the synthesized cDNA products were amplified using the SYBR Green Real-Time PCR Master Mix (Beyotime Biotechnology) on a CFX96TM real-time PCR system (Bio-Rad, U.S.A.). Using glyceraldehyde-3-phosphate dehydrogenase (GAPDH) as a normalization factor, the data were analyzed. The forward and reverse sequences of primers were shown in Table 1.
| Gene | Forward primer sequence | Reverse primer sequence |
|---|---|---|
| CCL17 | GACTTTTCTGCAGCAGTGCCAG | CCGAGAGTGCTGCCTGGATTACTTCAA |
| Jmjd3 | CTACACCCAGCATTTATTTGGAG | GCCTAAGTTGAGCCGAAGTG |
| GAPDH | AGGTCATCCATGACAACTTT | AGTCTTCTGGGTGGCAGT |
After blood samples were collected, held for 30 min, and centrifuged at 3500 × g for 15 min at 4 °C, the supernatant was collected. The levels of CCL17 in serum were determined using an ELISA kit (Multi Sciences Biotech, Ltd., China) according to the instructions provided by the manufacturer. In this study, optical density (OD) values were determined by using a microplate reader (Bio-Rad) at a wavelength of 450 nm. The cytokine concentrations for the various groups were determined by comparing sample values to a standard curve.
Immunofluorescence StainingThe fluorescence immunohistochemistry procedure was carried out following the previous step.37,38) We perfused rats from the ascending aorta with PBS followed by 4% paraformaldehyde in 0.1 M phosphate buffer. Following perfusion, the spinal cord was collected, post-fixed in 4% paraformaldehyde for 2 h, and then resuspended in 30% sucrose phosphate buffer over a period of 48 h. The sections of the tissues (10 µm) were prepared using a cryostat (Leica, CM1950) for immunofluorescence staining. We washed the sections in phosphate buffer and blocked them with 5% goat serum in 0.3% Triton X-100 for 1 h at 37 °C. Primary antibody (CCL17, 1 : 200, Bioss antibodies, China), c-fos (1 : 200, Bioss antibodies), or IRF4 (1 : 200, Bioss antibodies) was then applied overnight at 4 °C, followed by a secondary antibody conjugated to fluorescein isothiocyanate (FITC) for 2 h at 37 °C. 4′-6-Diamidino-2-phenylindole (DAPI) was incubated with the sections for 10 min at room temperature. Images were captured with a CCD camera and analyzed with image J.
H&E StainingAfter collecting tissues around the hindpaw incision, they were fixed for 24 h with 4% paraformaldehyde. The tissues were then dehydrated in sequence using sucrose solutions of 10, 20, and 30%. This was followed by embedding these samples in a compound with an optimal cutting temperature and preparing slices of 5 mm thick. Step-by-step H&E staining was performed on the slides in accordance with the instructions provided by the manufacturer. In the final step, the sections are examined under a microscope and photographed.
Statistical AnalysisStatistical analysis was conducted using SPSS 25.0 software. First, all data were analyzed for normality and homogeneity of variance. In the case of a normal distribution, data are represented as mean ± standard deviation. Data from repeated measures were then analyzed using the spherical method. The one-way ANOVA method was used when p > 0.05. Otherwise, repeated-measures ANOVA was used to analyze the data. Using the LSD test, comparisons were made between the groups. p < 0.05 was considered statistically significant.
First, we explored whether CCL17 was involved in the postoperative pain induced by a plantar incision. Sprague–Dawley rats were randomly assigned to either a sham group or a PI group. In the PI group, rats suffered significant mechanical and thermal allodynia after incisions of the hind paws. It is apparent in Fig. 1A that the rats in the PI group developed mechanical allodynia following the operation as compared to the rats in the sham group (p < 0.001 (2 h), p < 0.001 (4 h), p < 0.001 (8 h), p < 0.001 (24 h)). In addition, as shown in Fig. 1B, there was a remarkable reduction in thermal allodynia in the rats of the PI group following surgery (p < 0.001 (2 h), p < 0.001 (4 h), p < 0.001 (8 h), p < 0.001 (24 h)). Specifically, it has been demonstrated that Jmjd-3 plays an important role in the upregulation of CCL17, which, in turn, is involved in inflammatory responses. As part of our study, real-time PCR analyses were performed to assess simultaneously the levels of CCL17 and its upstream partner, Jmjd-3, in the spinal cord of a postoperative pain rat in order to confirm its role in postoperative pain. It can be seen in Fig. 1C that the CCL17 level was significantly higher (p < 0.001) in the PI group compared with the sham group. Moreover, CCL17 levels in serum were also assessed, and the results showed that the PI group’s level was significantly higher than that of the sham group in Fig. 1D. Jmjd-3 levels in the PI group also increased significantly (p < 0.001), as predicted in Fig. 1E. Additionally, we performed immunohistochemical analysis to detect the levels of IRF4 in the spinal cord. We found that the expression of IRF4 was significantly upregulated by peripheral stimulation, as expected in Figs. 1G–I. All of these findings suggest that CCL17 is implicated in the pain caused by a plantar incision in the postoperative period.
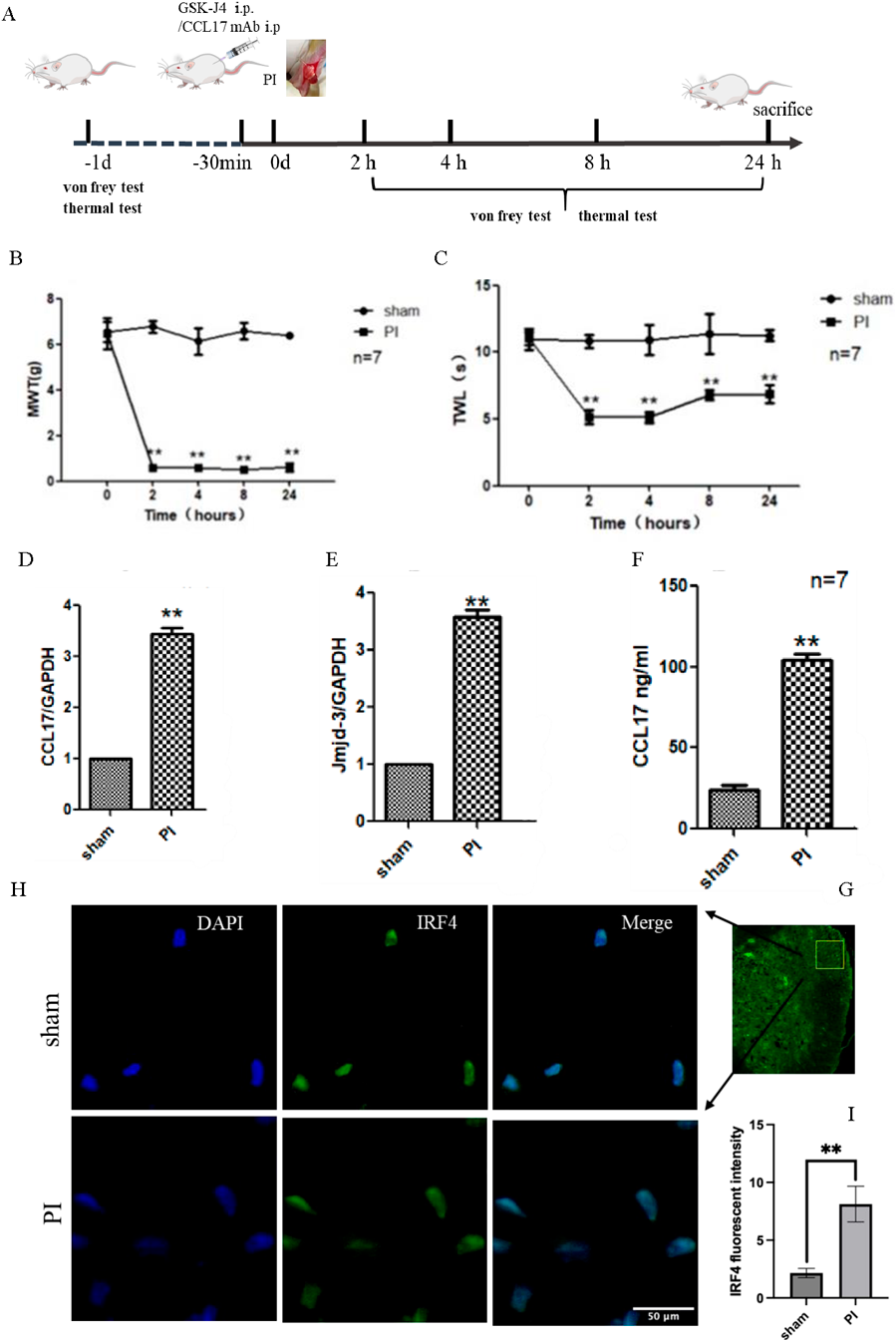
(A) Diagram illustrating the progress of the study protocol throughout the experiment. Rats from the PI group experienced mechanical (B) and thermal (C) allodynia after injury compared with rats from the sham group. The mechanical withdrawal thresholds (MWT) of the hindpaw were determined by the von Frey hair, and the thermal withdrawal latency (TWL) was evaluated at 2, 4, 8 and 24 h postoperatively, respectively. # p < 0.05, compared to the sham group. (D) A quantitative analysis of CCL17 mRNA levels in the spinal cord was conducted using real-time PCR. (E) A quantitative analysis of the levels of Jmjd3 mRNA in the spinal cord was conducted using real-time PCR. (F) CCL17 levels in the serum were measured by ELISA analysis. (G, H) Immunofluorescence microscopy-based IHC was utilized to investigate the expression of IRF4 in the spinal cord horn. Calibration bars: 50 µm. (I) Quantification of IRF4 in the Spinal dorsal horn. * p < 0.05,** p < 0.01, *** p < 0.001, compared with the sham group.
The effect of CCL17 blocking on postoperative pain was then investigated so as to further clarify the role of CCL17 in postoperative pain. Briefly, animals were injected intraperitoneally with anti-CCL17mAb 30 min prior to surgery, and then postoperative pain models were established using these animals. As a follow-up, behavioral tests were performed at 2, 4, 8, and 24 h following the operation. In Fig. 2A, we found that rats treated with anti-CCL17mAb showed significantly higher MWT 2 to 24 h after surgery when compared with rats in the PI group (p = 0.002(2 h), 0.006(4 h), 0.005(8 h), 0.015(24 h)). Similar trends were observed for thermal hyperalgesia in rats administered anti-CCL17mAb. Figure 2B shows that rats treated with anti-CCL17mAb display longer TWLs and less thermal hyperalgesia than rats treated with PI (p < 0.001 (2 h), p < 0.001 (4 h), p < 0.001 (8 h), p < 0.001 (24 h)).
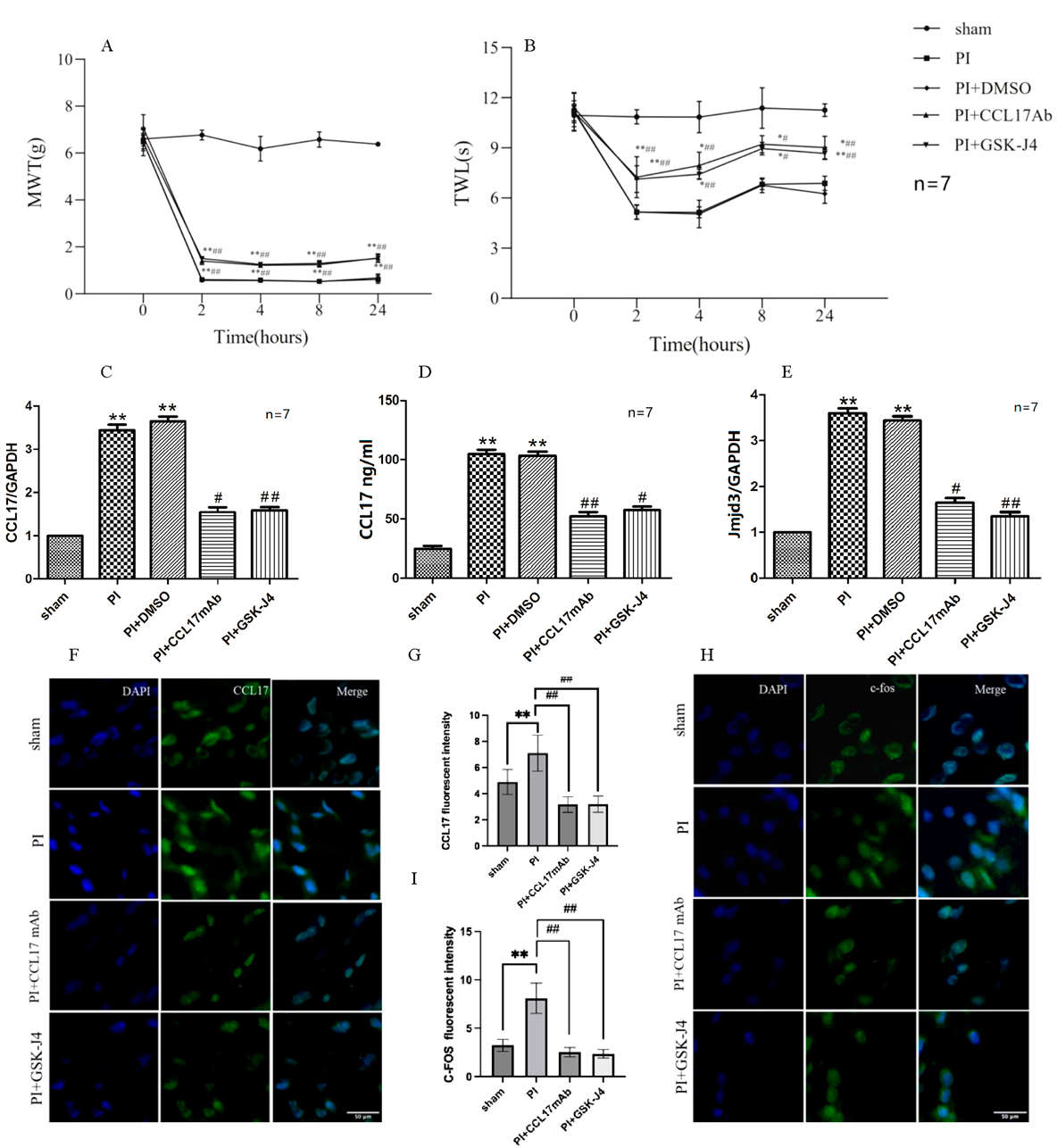
MWT of hindpaw was determined by the von Frey hair, and TWL was measured by thermal tests 2, 4, 8, and 24 h after surgery. By blocking CCL17, anti-CCL17mAb/GSK-J4 attenuated the effects of both mechanical allodynia (A) as well as thermal hypersensitivity (B) caused by surgical injury. The levels of CCL17 and Jmjd3 were reduced in the PI group when CCL17 was blocked with anti-CCL17mAb/GSK-J4. By using real-time PCR analysis, the levels of CCL17 in rats from sham, PI, PI + CCL17 mAb, PI + GSK-J4, and PI + DMSO were determined. The CCL17 mRNA (C) levels were quantified by real-time PCR in the spinal cord. (D) CCL17 levels in serum were examined by ELISA. Jmjd3 mRNA levels (E) in the spinal cord were quantified using real-time PCR. (F) The slices of the spinal cord were stained for CCL17 by the CCL17-specific antibody (green), and nuclei by Hoechst (blue) using immunofluorescence staining. (G) Quantification of CCL17 in the spinal cord horn. (H) The slices of the spinal cord were stained for c-fos by the c-fos-specific antibody (green), and nuclei by Hoechst (blue) using immunofluorescence staining. (I) Quantification of c-fos in the spinal cord horn.Compared to the sham group, * p < 0.05, ** p < 0.01, *** p < 0.01. Compared to the PI group, # p < 0.05, ## p < 0.01, ### p < 0.001.
In an effort to further confirm the important role of CCL17 in postoperative pain, we used GSK-J4, a specific inhibitor of Jmjd-3, to inhibit the production of CCL17 to observe its effect on postoperative pain. A direct target of Jmjd-3-mediated demethylation is IRF4, which is key in the up-regulation of CCL17 formation. A greater understanding has been gained that Jmjd3 is important in the direct upregulation of IRF4 and, ultimately, CCL17-mediated inflammation.39) To begin with, we examined whether Jmjd-3 inhibitor GSK-J4 ameliorated hyperalgesia in rats suffering from PI. The results of this study showed that rats administered with GSK-J4 were attenuated of mechanical and thermal allodynia from 2 to 24 h after the operation. The same trend was observed when the rats were administered with an anti-CCL17mAb. As shown in Fig. 2A, rats injected with GSK-J4 had decreased mechanical allodynia and increased MWT at 2, 4, 8, and 24 h after surgery (p < 0.001 (2 h), 0.011 (4 h), 0.002 (8 h), and p < 0.001 (24 h) compared to rats injected with PI. Furthermore, for thermal hyperalgesia, the rats treated with GSK-J4 showed much longer TWL and less thermal allodynia at 2, 4, 8, and 24 h following surgery (p < 0.001 (2 h), p < 0.001 (4 h), p < 0.001 (8 h), and p < 0.001 (24 h)) in Fig. 2B. Taking these findings into account, it can be concluded that the blockade of CCL17 with anti-CCL17mAb or GSK-J4 had an ameliorative effect on mechanical allodynia and thermal hyperalgesia in a rat model of PI.
Anti-CCL17mAb/GSK-J4 Inhibited CCL17-Mediated Injury in Rats with Postoperative PainAdditionally, we investigated the potential effects of anti-CCL17mAb/GSK-J4 in rat models of postoperative pain. We used real-time quantitative PCR analyses to measure CCL17 and Jmjd-3 levels in rats in the following groups: sham, PI, PI+ CCL17mAb, PI+ GSK-J4, and PI + DMSO. As shown in Fig. 2C, the levels of CCL17 were significantly decreased in the PI+ CCL17mAb (p = 0.001) and PI+ GSK-J4 (p < 0.001) groups compared with the PI + DMSO group. As shown in Fig. 2D, rats treated with anti-CCL17mAb (p < 0.001) or GSK-J4 (p = 0.001) exhibited significantly reduced serum levels of CCL17 in comparison with rats with PI. In addition, Jmjd-3 levels were simultaneously decreased in the PI+ CCL17mAb (p < 0.001) and PI+ GSK-J4 (p < 0.001) groups compared with the PI + DMSO group in Fig. 2E. To further confirm the role of CCL17 in PI pain, we also used an immunohistochemical technique to detect the levels of CCL17 in the spinal cord. As seen in Figs. 2F–G, the immunohistochemical results were in agreement with the Western blot and real-time PCR data obtained previously. In order to determine the effect of anti-CCL17 mAb or GSK-J4 on neurons, immunohistochemistry analysis was conducted to measure levels of c-fos in the spinal cord of rats. We found that significant activation of c-fos was observed in rats of the PI group in response to peripheral stimulation, as predicted. However, c-fos levels were reduced by using anti-CCL17 mAb or GSK-J4 (Figs. 2H–I). Consequently, these results indicate that anti-CCL17mAb and GSK-J4 inhibit surgical-mediated CCL17 and allodynia in rats suffering from postoperative pain.
CCL17 Blockade Relieved Tissue Injury after SurgeryFurther, we evaluated the effects of CCL17 blockade on rats suffering from postoperative pain using the method of dyeing with H&E. It was observed that compared with the Sham group, rats in the PI group had a large number of inflammatory cells infiltrating the area of the plantar incision, swelling and deformation of the cells, an arrangement of dermal tissue that was disturbed, a rupture of the fibrous tissue, and a loose and disordered arrangement of tissue. It can be seen, however, that their conditions were improved in the PI+ CCL17mAb group and the PI + GSK-J4 group. The plantar tissue of the rats treated with PI+ CCL17mAb or PI + GSK-J4 showed less infiltration of inflammatory cells, increased cell regularity, and less rupture of fibrous tissue (Fig. 3) compared to PI. It was found that the inhibition of CCL17 by PI+ CCL17mAb or PI + GSK-J4 regulator reduced tissue injury.

The tissues around the plantar incision of rats from following groups, including sham; PI; PI + CCL17 mAb; PI + GSK-J4; PI + DMSO group, were detected by H&E dyeing. Compared with the sham group (A, a), the tissues around the plantar incision of rats in the PI group (B, b) and the PI + DMSO (E, e) showed a large number of inflammatory cells infiltration, cell swelling and deformation, and fibrous tissue rupture, loose and disorder. Anti-CCL17mAb/GSK-J4 ameliorated the tissue damage in the PI group. The plantar tissue of the rats showed that less infiltration of inflammatory cells, increased regularity of cell arrangement, and less rupture of fibrous tissue in the PI + CCL17mAb (C, c) and the PI + GSK-J4 groups (D, d), compared with the PI group.
In our study, we found a significant increase in CCL17 in the spinal cord of rats suffering from postoperative pain, which is consistent with the changes in hyperalgesia observed in these rats. A significant reduction in mechanical hyperalgesia and thermal allodynia was observed with anti-CCL17mAb/GSK-J4 treatment in PI rats as well. In conclusion, these findings suggest that plantar incision-induced postoperative pain is associated with high expression of CCL17 and that CCL17 blockade may be an effective treatment strategy.
The immune system and the nervous system are closely related to each other. A chemokine acts as a multifunctional messenger of the immune system, and it plays an influential role in the development of the central nervous system, neurophysiology homeostasis, and neuroinflammation.40,41) The chemokines and their receptors, including CXCL1/CXCR2, CCL2/CCR2, and CX3CL1/CX3CR1, contribute to the association of myeloid cells with the brain in neuroinflammatory diseases, such as multiple sclerosis.42) Researchers have also shown that chemokines are used by neurons and glial cells to promote the discovery of axonal pathways, the migration of neuronal stem cells, and modulate synaptic transmission under dynamic equilibrium conditions.43) The high-affinity receptor for CCL17, CCR4, in addition to being expressed in a variety of immune cells, is also expressed in astrocytes, neurons, and microglia, playing both homeostasis and an inflammatory role.44) A study has shown that systemic application of CCL17 leads to inflammatory pain in a COX-dependent manner.9) An anti-CCL17mAb blocking pain was demonstrated to be effective in human microglia by showing CCR4 expression.45) Based on the findings above, it appears that CCL17 plays an important role in pain and that inhibition of CCL17 has analgesic effects.7) We established a rat model of plantar incision (PI) and detected CCL17 levels by real-time PCR and ELISA, indicating that CCL17 may play a role in acute postoperative pain. Specifically, the inhibition of CCL17 expression reduced pain performance in rats within 24 h of surgery, further indicating that CCL17 is an important cause of plantar incision pain.
It has been established that chemokine-related neuroinflammatory responses contribute to opioid-induced hyperalgesia, the development of neuropathic pain, and the development of inflammatory pain.46–50) It has been demonstrated that the chemokine CCL3 plays an important role in the facilitation of opioid-induced pain.50) The spinal cord is highly upregulated for CXCL10, which may contribute to the development of neuropathic pain following peripheral sciatic nerve injury or ligation of the sciatic nerve49) Furthermore, the chemokine CXCL5 is associated with an increase in hyperalgesia in inflammatory conditions.51) Pain caused by arthritis is mediated by CCL17, and blockade of CCL17 alleviates pain. In clinic, it is vital to identify the underlying mechanisms of postoperative pain and then seek appropriate treatment methods for them. In our study, we found significant increases in CCL17 levels in the spinal cord as a result of plantar incisions, which were associated with postoperative pain. The present study is the first to report that inhibiting CCL17 significantly reduces postoperative pain. Based on these results, it appears that the CCL17 plays an important role in the pathogenesis of postoperative pain.
The granulocyte macrophage-colony stimulating factor (GM-CSF) plays an essential role in inflammatory and arthritic disorders.52,53) There is, however, a possibility that therapies that target GM-CSF function directly may cause adverse side effects, in which case downstream pathways and mediators need to be identified.53) It has been shown that GM-CSF stimulates CCL17 via Jmjd3-regulated IRF4 to mediate inflammation and that CCL17 blockade ameliorates GM-CSF-dependent inflammatory pain and arthritic pain.32) Studies have demonstrated that the GM-CSF/Jmjd-3/IRF4/CCL17 pathway in monocytes and macrophages of humans and mice plays an important role in pain occurrence and development.7,9) It is interesting to note that CCL17 was the most up-regulated gene in mouse macrophages and human monocytes subjected to GM-CSF treatment.31,32) The presence of high levels of CCL17 has been shown to contribute to inflammation caused by GM-CSF, as well as symptomatic pain associated with GM-CSF-induced and dependent arthritis.7,53) The pro-inflammatory response induced by GM-CSF via CCL17, in turn, requires the activity of IRF4 and Jmjd3.7,54,55) Application of the Jmjd-3 inhibitor GSK-J4 intervened in GM-CSF-driven inflammatory pain. Recent studies have demonstrated that the GM-CSF/CCL17 pathway alleviates experimental osteoarthritis pains and related diseases, which led to the opening of clinical trials utilizing CCL17 antagonists for osteoarthritis.6–9,56) Meanwhile, CCL17 also mediates IL-4-driven inflammatory pain through Jmjd3-regulated IRF4, and blocking CCL17 relieves inflammatory pain.55) CCL17 expression in human monocytes is regulated by Jmjd3 demethylase activity on the IRF4 promoter, which has been shown to play a role in IL4-induced IRF4 and CCL17 expression.7,55) It has been shown that CCL17 is responsible for GM-CSF-induced inflammatory pain, which is itself a source of pain. In previous studies, it has been demonstrated that GM-CSF can cause mechanical hyperalgesia and is essential for the development of inflammatory pain and inflammation.7,53,57,58) Currently, local inflammatory reactions have been found in postoperative incision pain, leading to infiltration and activation of lots of inflammatory cells.
We found that Jmjd-3/IRF4/CCL17 were highly expressed in this PI model, which is consistent with the observed behavioral allodynia. By comparing the postoperative pain thresholds of mechanical pain and thermal stimulation in the anti-CCL17mAb or GSK-J4 (Jmjd-3) administration group and the PI group, it was observed that the pain thresholds in the drug administration group were significantly higher than those in the PI group, and the hyperalgesia was ameliorated by blocking CCL17. H&E staining was used to observe the tissues around the plantar incision of the rats after surgery. It was found that inhibition of CCL17 expression could not only improve the postoperative pain threshold of the rats, but also relieve hyperalgesia, and promote tissue recovery. It should be noted, however, that our experiment still has some shortcomings. Our follow-up study will investigate further the role of the GM-CSF/Jmjd3/IRF4/CCL17 pathway in postoperative pain pathology and conduct a long-term intervention for chronic pain using either anti-CCL17-mAb or GSK-14, as well as observe its therapeutic effects.
In conclusion, in this study, we first investigated that CCL17 is closely related to the post-operative pain induced by the plantar incision pain model, and it is likely to be one of the inducing factors of postoperative pain. Additionally, our results suggest that CCL17 blockade may be an effective method of treating postoperative pain.
Several Grants were awarded to this research, including Grant No. 81300969 from the National Natural Science Foundation of China; Grant No. ZR2020MH130 from the Shandong Province Natural Science Foundation of China; and Grant No. 202004070430 from the Shandong Health and Medical Innovation Project of China.
Yingxia Liang designed the study. Tian Zhang and Yijia Zhang performed the experiments, analyzed and interpreted the data. Zhiyu Zhang designed, drafted and revised the manuscript. All authors read and approved the final manuscript.
The authors declare no conflict of interest.