2024 年 47 巻 10 号 p. 1668-1674
2024 年 47 巻 10 号 p. 1668-1674
β-Adrenergic receptor blockers (β-blockers) are used to treat hypertension, ischemic heart disease, chronic heart failure, and tachyarrhythmia. The main side effects of treatment include bradycardia, atrioventricular block, and hypotension. Bradycardia may result in pacemaker implantation as well as the discontinuation of β-blockers. Bradycardia is difficult to confirm at a single institution because it diagnosed only by symptoms when electrocardiogram (ECG) are not routinely performed. Previous studies reported an increase in bradycardia in heart failure patients treated with β-blockers; however, limited information is currently available for non-heart failure patients. Bradycardia induced by β-blockers has not yet been comprehensively examined. Therefore, the present study investigated data on the incidence and duration of bradyarrhythmia caused by β-blockers using the Japanese Adverse Drug Event Report database (JADER). Cases of adverse effects associated with this medication were extracted from JADER and Fisher’s exact test was performed to assess whether each β-blocker caused bradyarrhythmia. In addition, only data from patients who reported bradyarrhythmia after β-blocker treatment were extracted, and the Weibull distribution was used to analyze the time-to-onset of bradyarrhythmia. Thirteen β-blockers caused bradyarrhythmia and signals were observed for 12 drugs, except nadolol. Bradyarrhythmia induced by oral β-blockers was more likely to be of the early failure type, and developed within 2 months of treatment initiation with most β-blockers. A comprehensive analysis of bradyarrhythmia with β-blockers suggests that careful monitoring is needed, particularly early in the initiation of treatment.
β-Adrenergic receptor blockers (β-blockers) are widely used to treat hypertension, ischemic heart disease, chronic heart failure, and tachyarrhythmia. There are three subtypes of β-receptors: β1, β2, and β3, which differ in affinity to catecholamines and tissue distribution.1,2) β1-Receptors are present in the heart and increase heart rate by their positive chronotropic action and myocardial contractions by their positive inotropic action. β2-Receptors are present in bronchial smooth muscle, vascular smooth muscle, and uterine smooth muscle and exert bronchodilator, vasodilatory, and uterine muscle relaxant effects. β3-Receptors are present in adipose tissue and bladder smooth muscle and are involved in lipolysis and smooth muscle relaxation. β-Blockers are classified according to their affinity for β1-receptors, the presence or absence of αl-receptor blockade, the presence or absence of intrinsic sympathomimetic activity (ISA), and whether they are lipophilic or hydrophilic.3) α-Receptors are involved in vasoconstriction. ISA characterizes a group of β-blockers that are able to stimulate β-adrenergic receptors (agonist effect) and oppose the stimulating effects of catecholamines (antagonist effect) in a competitive manner. β-Blockers without ISA are recommended in antihypertensive therapy for hypertensive patients with concomitant coronary artery disease and in heart rate control therapy for patients with atrial fibrillation.4,5) Since lipophilic drugs cross the blood-brain barrier, central nervous system side effects, such as sleep disturbances and depression, need to be considered.
In addition to central nervous system side effects, β-blocker side effects include bradycardia, atrioventricular block, and hypotension in the cardiovascular system, bronchospasms in the respiratory system, and impaired glucose tolerance and decreased insulin sensitivity in the metabolic and endocrine systems.3) Bradycardia may result in pacemaker implantation as well as the discontinuation of β-blockers. Bradycardia is suspected in clinical practice based on subjective symptoms, such as dizziness and lightheadedness, and is diagnosed by electrocardiogram (ECG) findings. However, physicians who do not routinely conduct ECG are considered to diagnose bradycardia based on subjective symptoms alone.
The CIBIS-II trial, which investigated the efficacy of bisoprolol in patients with heart failure and left ventricular systolic dysfunction, reported that mortality was lower with bisoprolol than with a placebo; however, bradycardia and hypotension were observed in the bisoprolol group.6) In the US Carvedilol program, the CIBIS trial and MERIT-HF trial, which examined the efficacy of β-blockers for heart failure, bradycardia was one of the most common reasons why the target dose was not up-titrated for patients. However, the discontinuation of β-blockers due to a low heart rate was rare in large outcome trials (0.3–0.9%).7) A systematic review that examined the effects of β-blockers on clinical endpoints in patients with chronic kidney disease (CKD) stages 3 to 5, including those on dialysis, reported an increased risk of bradycardia and hypotension with β-blockers than with a placebo in heart failure patients. However, limited information is currently available on whether treatment with β-blockers was associated with a reduced heart rate or bradycardia in non-heart failure patients.8) A Japanese study on the efficacy of bisoprolol in patients with paroxysmal atrial fibrillation reported that severe bradycardia occurred in 3 out of 136 patients, which required the discontinuation of treatment.9)
The Pharmaceuticals and Medical Devices Agency (PMDA) released the Japanese Adverse Event Reporting Database (JADER), collected through the Adverse Event Reporting System, which is available to the public. To verify drug safety, an analysis using a spontaneous reporting system (SRS) database of adverse events, such as JADER, is considered to be useful.10,11) Signal detection using SRS provides important information on the risk populations, risk factors, and clinical characteristics of known serious adverse drug reactions.12) Further information on adverse events may help medical staff select drugs based on their properties, differences, and propensity to cause adverse events.
To the best of our knowledge, bradycardia induced by β-blockers has not yet been comprehensively examined. In the present study, we investigated data on the propensity and duration of bradyarrhythmia induced by β-blockers using the JADER database.
Since April 2004, PMDA has reported cases of adverse events associated with medications in the JADER database.13) The JADER database may be downloaded from the PMDA website. In the present study, we accessed the JADER database from the PMDA website and conducted an analysis using data reported between April 2004 and July 2022.13)
Production of a Data Analysis TableJADER data consist of four tables: (a) patient demographic information (DEMO), (b) drug information (DRUG), (c) adverse events (REAC), and (d) medical history (HIST). Figure 1 shows the number of reports in each table obtained between April 2004 and July 2022. Of these four tables, the DEMO, DRUG, and REAC tables were used for analyses in the present study.
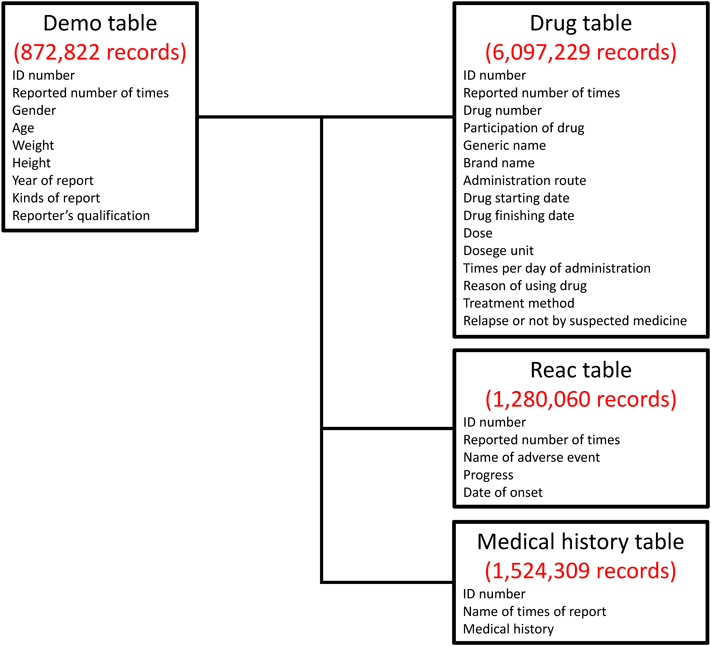
Four tables were included in the JADER database. The red number shows the number of reports obtained between April 2004 and July 2022.
Duplicate data were initially removed from the DRUG and REAC tables.14) Tables with duplicates removed were then combined using patient identification numbers to create the DRUG_REAC table. The DEMO table was then merged into the DRUG_REAC table using patient identification numbers. This table was named the “All Data Table.” Figure 2 shows a flow chart for the construction of data analysis tables. In each case, the contribution of the drug to the adverse event was classified into three categories: suspect drug, concomitant drug, and interaction. All cases classified by these categories were extracted for analysis.

We removed duplicate data from the drug information table and REAC table.11) The DEMO table was combined with the REAC table and drug information table using the ID number for each table. This table was called the “All data table.” In each patient, the causes of medication-related adverse events were classified into three categories: “suspected medicine,” “concomitant medicine,” and “interaction.” We extracted cases that were all category data (“suspected medicine,” “concomitant medicine,” and “interaction”). We then extracted cases with the adverse effect of “bradyarrhythmia” from this table.
A β-blocker is a drug that binds selectively to β adrenoceptors, producing the competitive and reversible antagonism of the effects of β adrenergic stimuli on various organs.15) In this analysis, external medicines, such as patches and eye drops, were excluded.
Definition of BradyarrhythmiaAdverse event terms in the JADER database are recorded based on the Preferred Terms in the Medical Dictionary for Regulatory Activities/Japanese version (MedDRA/J). Adverse events reported in the JADER database that corresponded to bradyarrhythmia were retrieved from the Standardized MedDRA Queries. In the present study, 45 preferred terms were extracted from the narrow scope term “bradyarrhythmia (including conduction disorders and sinus node dysfunction)” in the Standardized MedDRA Queries listed in MedDRA 25.0 (Supplementary Table S1).
Relationship between Suspected Medicines and BradyarrhythmiaThe reporting odds ratio (ROR) and Fisher’s exact test were used to assess the risk of bradyarrhythmia for each registered drug. The presence or absence of β1-receptor selectivity and the ISA of each β-blocker for which bradyarrhythmia was reported were also examined. A 2 × 2 contingency was initially created based on two classifications: the presence or absence of bradyarrhythmia and the presence or absence of the suspected medicine. Therefore, we calculated the p-value in Fisher’s exact test and the ROR (Table 1). Since it was not possible to calculate the 2 × 2 contingency table with zero cells and the estimation may become unstable with a small cell frequency, 0.5 was added to all cells as a correction (Haldane Anscombe half correction).16) The ROR calculation and associated 95% confidence intervals (CI) and Fisher’s exact test were comprehensive for all registered drug and bradyarrhythmia combinations. In the present study, a signal was considered present if ROR > 1, the lower limit of 95% CI for ROR > 1, and the number of cases ≥3. A scatter plot consisting of ROR and p-values was subsequently created for the visual interpretation of adverse drug events. A scatter plot was constructed by plotting the negative log of the p-value (−log [p-value]) from Fisher’s exact test on the y-axis and the x-axis showed the log of ROR (ln ROR)17) (Fig. 3). The scatter plot corresponded to the volcano plots frequently used to examine gene expression trends in bioinformatics.
| Bradyarrhythmia | Non-bradyarrhythmia | |
|---|---|---|
| Reports with the suspected medicine | a | c |
| All other reports | b | d |
ROR (reporting odds ratio) = (a/b)/(c/d) = ad/bc. Cross-tabulation is structured with reports on the suspected medicine, all other reports, reports with bradyarrhythmia, and reports without bradyarrhythmia (a–d indicate the number of cases). The reporting odds ratio (ROR) was calculated as shown.

This figure shows the relationship between bradyarrhythmia and the medicine suspected to have caused it. The X-axis shows the natural logarithm of odds ratio (ln ROR) values, while the Y-axis shows the common logarithm of inverse p-values (−log [p-value]) obtained by Fisher’s exact test. The dotted line on the Y-axis represents a p-value of 0.05. Plot colors represent the number of reported adverse events. Blue, green, and red dots are common logarithms of total reported numbers (from 1.0 to 4.6).
In the analysis of the time-to-onset of adverse events, only data from patients who reported bradyarrhythmia after receiving β-blockers were extracted. Among the β-blockers, the injectable form was excluded from this analysis because it is mainly used in the acute setting and therefore is considered to have a different purpose of use and patient background. The analysis of the time-to-onset of bradyarrhythmia was also conducted with or without β1-receptor selectivity or the ISA of each β-blocker. The number of days until the development of bradyarrhythmia was calculated from the date of the initial administration of the drug and the date of development of bradyarrhythmia reported in the JADER database. Unknown reports with missing information on the date of treatment initiation or the development of adverse events were excluded. The number of days until the onset of an adverse event was calculated as “date of the adverse event-date of the start of treatment +0.5.”18) In the present study, the upper limit of the time-to-onset of adverse events was set at 365 d.
The Weibull shape parameter test is used to analyze time-to-onset data and describes the non-constant rate of the incidence of adverse events.19) A time-to-onset analysis using the Weibull distribution was performed and the Weibull parameters α and β were calculated. The shape parameter α of the Weibull distribution represents the spread of the distribution, while the shape parameter β represents the failure rate distribution against time. The failure rate corresponds to the development of an adverse reaction: when β < 1 (early failure type), the incidence of adverse reactions decreases with time; when β = 1 (random failure type), adverse reactions develop at a constant pace; and when β > 1 (wear-out failure type), the incidence of adverse reactions increases with time.20)
Statistical AnalysisMeans (± standard deviation) were calculated for all continuous variables. p-Values <0.05 were considered to be significant. All data analyses were performed using JMP® Pro 16.2.0 (SAS Institute Inc., NC, U.S.A.) software.
The DRUG table included 6097229 records, the REAC table included 1280060 records, and the DEMO table included 872882 records. The total number of cases is shown in the “all data table” and was 6618979 records (Fig. 2).
Bradyarrhythmia-Inducing MedicationsBased on aggregate results of reports for drugs causing bradyarrhythmia, bradyarrhythmia was reported for 13 β-blockers and signals were observed for 12 drugs, except nadolol (Table 2). The most reported drug was carvedilol (β1 non-selective, without ISA) (n = 440), with an ROR of 2.824 (95% CI: 2.569–3.649), followed by bisoprolol (β1 selective, without ISA) (n = 342, ROR 2.487, 95% CI: 2.234–2.768) and atenolol (β1 selective, without ISA) (n = 122, ROR 3.051, 95% CI: 2.551–3.649).
| Drug | β1-Selectivity | ISA | Reporting times | Odds ratio | 95%CI | p-Value |
|---|---|---|---|---|---|---|
| Carvedilol | No | No | 440 | 2.824 | 2.569–3.105 | p < 0.001 |
| Bisoprolol | Yes | No | 342 | 2.487 | 2.234–2.768 | p < 0.001 |
| Atenolol | Yes | No | 122 | 3.051 | 2.551–3.649 | p < 0.001 |
| Metoprolol | Yes | No | 57 | 4.176 | 3.214–5.427 | p < 0.001 |
| Propranolol | No | No | 55 | 3.362 | 2.577–4.386 | p < 0.001 |
| Landiolol | Yes | No | 34 | 4.042 | 2.883–5.667 | p < 0.001 |
| Carteolol | No | Yes | 31 | 5.701 | 3.996–8.135 | p < 0.001 |
| Arotinolol | No | No | 28 | 3.397 | 2.344–4.924 | p < 0.001 |
| Betaxolol | Yes | No | 20 | 5.980 | 3.848–9.294 | p < 0.001 |
| Celiprolol | Yes | Yes | 15 | 3.885 | 2.347–6.429 | p < 0.001 |
| Acebutolol | Yes | Yes | 5 | 8.137 | 3.455–19.162 | p < 0.001 |
| Nipradilol | No | No | 3 | 3.249 | 1.128–9.360 | 0.097 |
95% CI: 95% confidence interval. “Reporting times” shows the number of cases that reported a medicine suspected as a cause of bradyarrhythmia.
Figure 3 shows a volcano plot of drugs suspected of causing bradyarrhythmia. The X-axis shows ln ROR. The positive direction of the X-axis indicated that more cases of bradyarrhythmia were reported than other adverse effects. The Y-axis shows the negative log of the p-value (−log [p-value]) of Fisher’s exact test. The positive Y-axis direction indicated a significant difference. Drugs in the upper right quadrant were significantly different from the ROR and were more likely to induce bradyarrhythmia. The results of the volcano plot indicated that β-blockers were associated with the development of bradyarrhythmia.
Among the 12 β-blockers that showed a signal in the present study, 11, with the exception of nipradilol, were in the upper right and were presumed to correlate with bradyarrhythmia.
Time-of-Onset of BradyarrhythmiaOf the 40612 records reporting bradyarrhythmia in the “all data table,” 1141 were caused by treatment with oral β-blockers. The median time-to-onset of bradyarrhythmia and Weibull shape parameters are summarized in Table 3.
| Drug | β1-Selectivity | ISA | n | Median (d) | Scale parameter: α | Shape parameter: β | Pattern | ||
|---|---|---|---|---|---|---|---|---|---|
| α | 95%CI | β | 95%CI | ||||||
| Bisoprolol | Yes | No | 108 | 46 (26.5–56.5) | 60.76 | 45.94–79.70 | 0.73 | 0.62–0.84 | Early failure |
| Carvedilol | No | No | 95 | 37.5 (20.5–60.5) | 60.62 | 45.25–80.43 | 0.74 | 0.63–0.87 | Early failure |
| Atenolol | Yes | No | 25 | 46.5 (25.5–112.5) | 66.84 | 36.59–118.34 | 0.73 | 0.52–1.00 | Random failure |
| Metoprolol | Yes | No | 17 | 25.5 (0.5–53.5) | 35.75 | 11.55–102.91 | 0.49 | 0.32–0.70 | Early failure |
| Propranolol | No | No | 9 | 4.5 (0.5–20.5) | 5.89 | 2.09–15.46 | 0.78 | 0.43–1.24 | Random failure |
| Arotinolol | No | No | 8 | 186.5 (0.5–307.5) | 130.31 | 30.92–503.23 | 0.62 | 0.31–1.09 | Random failure |
| Carteolol | No | Yes | 8 | 3 (0.5–68.5) | 18.50 | 2.74–110.32 | 0.45 | 0.25–0.71 | Early failure |
| Betaxolol | Yes | No | 6 | 38.5 (8.5–343.5) | 68.91 | 17.69–248.48 | 0.75 | 0.37–1.27 | Random failure |
95% CI: 95% confidence interval. “Median” shows the time-of-onset of bradyarrhythmia for each β-blocker. β < 1, early failure; β = 1, random failure; β > 1, wear-out failure.
The median times-to-onset of bradyarrhythmia induced by β-blockers were 37.5, 46, and 46.5 d for carvedilol, bisoprolol, and atenolol, respectively, which were the most frequently reported to cause bradyarrhythmia, respectively, and most β-blockers caused bradyarrhythmia within 2 months (Table 3).
The shape parameter β of carvedilol, bisoprolol, metoprolol (β1 selective, without ISA), and carteolol (β1 non-selective, with ISA) were 0.74 (95% CI: 0.63–0.87), 0.73 (95% CI: 0.62–0.84), 0.49 (95% CI: 0.32–0.70), and 0.45 (95% CI: 0.25–0.71), respectively, and the upper limit of 95% CI was less than 1, suggesting an early failure type with a decreasing incidence over time. The onset of bradyarrhythmia with β-blockers was the fastest for carteolol (β1 non-selective, with ISA) and the slowest for arotinolol (β1 non-selective, without ISA).
Among 872882 JADER adverse effect records, bradyarrhythmia due to oral β-blockers was reported in 1141 records (rate, 0.13%). There are currently no randomized controlled trials on β-blockers for hypertensive patients that evaluated bradycardia as an outcome,4) and bradycardia was not examined in a trial that investigated the heart rate-lowering effect of bisoprolol in patients with atrial fibrillation.21) In a large study on β-blockers in heart failure patients, bradycardia developed in between 2.3 and 12.9% of patients.7) Since patients may not consider mild dizziness or lightheadedness as an adverse event, they may not report it to their physicians unless it is serious, which may lead to ECG not being performed. By only analyzing suspected medicines reported in JADER, we may have limited the identification of risk factors for bradyarrhythmia. Therefore, we examined all data, including the suspected medicine, concomitant medicine, and interactions, in this analysis.
In the present study, many β-blockers were suspected to cause bradyarrhythmia. When noradrenaline released from sympathetic nerve endings binds to β-receptors in cardiomyocytes, intracellular G proteins and adenylate cyclase are activated and cAMP levels increase. cAMP then increases Ca2+ influx from Ca2+ channels via the activation of phosphatase and from the sarcoplasmic reticulum.22) β-Blockers suppress this cascade, thereby inhibiting cardiac contractions and lowering the heart rate. They also block the β-receptors on sinus node cells that serve as physiological stimulus generators, resulting in a decreased heart rate by slowing stimulus generation. They also exert a blocking effect on atrioventricular nodal cells, the relay pathway from the atria to the ventricles, and slow conduction, thereby accelerating decreases in the heart rate.
In the CIBIS-ELD study, which investigated the tolerability of bisoprolol and carvedilol in elderly heart failure patients, bisoprolol, with its greater β1 selectivity, was more effective at reducing heart rate and more frequently induced bradycardia.23) β-Blockers with ISA may be preferable for patients with bradycardia; however, their clinical benefits have not yet been clearly established because of their weaker heart rate-reducing effect due to a β2-receptor stimulation.
Nevertheless, in the present study, it was estimated that carvedilol, a β1-receptor non-selective drug, and acebutolol with ISA were also associated with bradyarrhythmia. Therefore, the development of bradyarrhythmia did not appear to differ between β1-receptor selectivity or the presence or absence of ISA.
In the present study, oral β-blockers with reported bradyarrhythmia were more likely to be of the early failure type. The median time-to-onset of bradyarrhythmia was often within 2 months of the initiation of treatment. β-Blockers may induce decreases in cardiac function, bradycardia, and blood pressure; therefore, in patients with atrial fibrillation, the initiation of treatment with a low dose, followed by adjustments according to symptoms, blood pressure, chest X-ray, and ECG, is recommended.5) In patients with hypertension, the dose needs to be increased at intervals of 4 weeks to 3 months based on cerebral ischemic signs, such as dizziness and orthostatic syncope, angina pectoris, myocardial ischemia findings on ECG, and the deterioration of QOL.4) In patients with heart failure, it is preferable to start with a very low dose followed by gradual increases every few days to two weeks.24)
It is reasonable to assume that bisoprolol and carvedilol, which are commonly used to treat heart failure and atrial fibrillation, are of the early failure type because, in the process of dose escalations, ECG was performed at the time of consultation and revealed bradyarrhythmia. The other β-blockers are mainly used to treat hypertension, and their doses are not increased as frequently as those for heart failure or atrial fibrillation, resulting in bradyarrhythmia early in the course of treatment and an increased likelihood of the early failure type. It is possible that β-blockers with fewer reports of bradyarrhythmia may have been of the random failure type because of the wider 95% confidence interval for the duration of onset. Furthermore, in consideration of the interval between dose escalations in heart failure and hypertension, the time until the onset of bradyarrhythmia was most likely within 2 months of the initiation of treatment. Bisoprolol and carvedilol, both general-purpose β-blockers, have been reported to cause a large number of bradyarrhythmia in this study, and the fact that they were the early failure type may indicate the occurrence of bradyarrhythmia in clinical practice.
In the present study, early failure β-blockers included bisoprolol and carvedilol, which do not have ISA, as well as carteolol, which has ISA. Carteolol, which had an earlier onset of bradyarrhythmia, is a non-selective β1-blocker, and arotinolol, which had a later onset of bradyarrhythmia, is also a non-selective β1-blocker.3,25) Therefore, other mechanisms may be involved. However, since there were only 1141 records of bradyarrhythmia caused by oral β-blockers in the JADER database, it may be necessary to consider an analysis of FEARS, which has more data than the JADER database, in order to examine the characteristic effects of β-blockers. A more detailed of the underlying causative mechanisms of β-blockers is needed to increase their safety.
There are several limitations that need to be addressed. The JADER database is based on SRS, and studies using spontaneous reporting adverse event databases have various biases. Mild adverse events are only occasionally reported, while severe adverse events are more frequently reported. This is a reporting bias and characteristic of a self-report database.26) Furthermore, this database is problematic because the relationships between drugs and adverse events is not clear.27) Assuming that several drugs are concomitantly administered to a single patient, it is difficult to identify the cause of the adverse event.11,28,29) Moreover, PMDA verifies details on fatal cases due to adverse events and examines the relationship between medicines and adverse events. However, other cases are reported based on judgments by the reporters. Cases in JADER included not only true, but also suspected adverse effects. Fourth, although the JADER database includes a list of reasons for drug use, it is incomplete, with missing information, so it is difficult to determine whether the purpose of β-blockers use is heart failure, atrial fibrillation, hypertension, or ischemic heart disease in this analysis. Fifth, in spontaneous reports such as the JADER database, it is difficult to identify risk factors because event rates cannot be calculated and there may be missing or inconsistent information or erroneous entries.30) Further analysis through medical record surveys and medical information databases is desirable to examine risk factors for bradyarrhythmia caused by β-blockers, such as concomitant medications, since concomitant use of β-blockers with non-dihydropyridine calcium channel blockers and antiarrhythmic drugs such as amiodarone may lower heart rate.
In conclusion, the present study investigated data on the incidence and duration of bradyarrhythmia induced by β-blockers using the JADER database. The present findings suggest that, during the initial period of β-blockers initiation, inpatients should be monitored for subjective symptoms such as dizziness and lightheadedness in addition to blood pressure and heart rate, and outpatients should be carefully monitored for symptoms such as dizziness and lightheadedness by consulting the prescribing physician if they are severe and by visiting the hospital every 1 to 2 weeks.
We would like to thank Miss Mana Shiraishi, Mr. Shunsuke Nagasawa, and Mr. Takuma Arakaki of the Meiji Pharmaceutical University, Department of Pharmacology for their great cooperation in conducting this research. We would like to express our gratitude here.
The authors declare no conflict of interest.
This article contains supplementary materials.